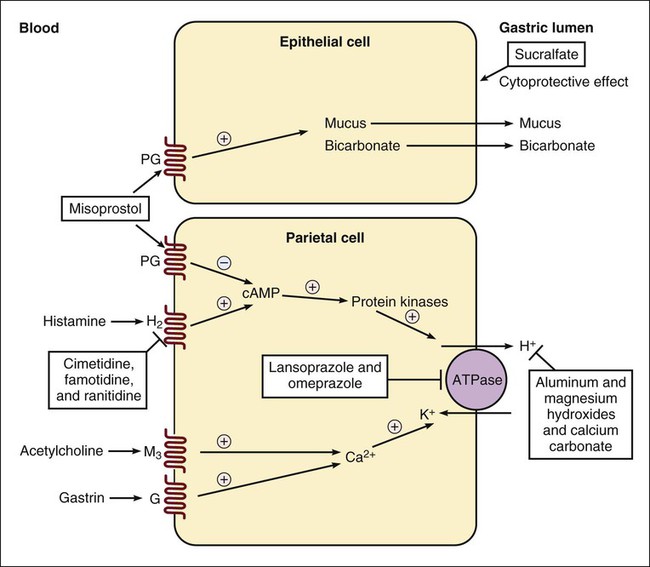
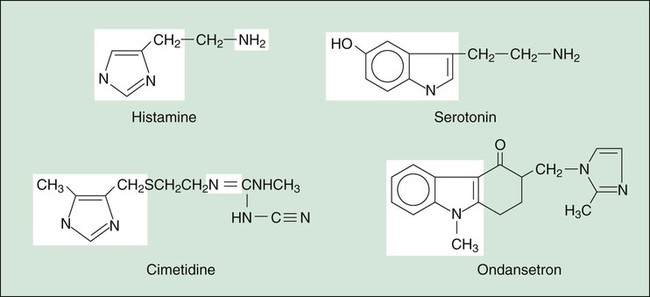
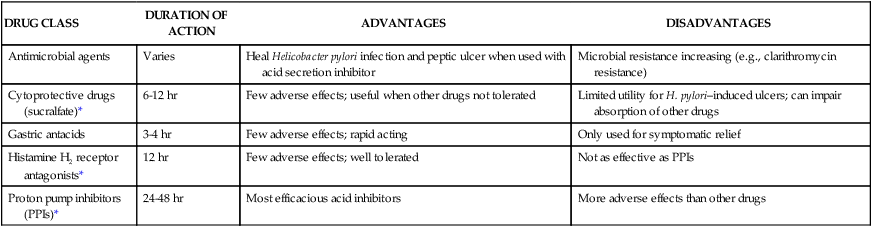
The structure of H2 blockers is similar to that of histamine (Fig. 28-2), and this enables the drugs to compete with histamine for binding to H2 receptors on gastric parietal cells (see Fig. 28-1). The H2 blockers have been shown to be potent inhibitors of both meal-stimulated secretion and basal secretion of gastric acid. When they reduce the volume and concentration of gastric acid, they produce a proportionate decrease in the production of pepsin because gastric acid catalyzes the conversion of inactive pepsinogen to pepsin. The H2 blockers also reduce the secretion of intrinsic factor, but not enough to significantly reduce vitamin B12 absorption. They have no effect on gastric emptying time, esophageal sphincter pressure, or pancreatic enzyme secretion. The H2 blockers are well absorbed from the gut and undergo varying degrees of hepatic inactivation before being excreted in the urine. Although the half-life of most H2 blockers is only 2 to 3 hours, their duration of action is considerably longer (Table 28-1), and these drugs are usually administered once or twice daily. TABLE 28-1 Properties of Drugs for Peptic Ulcer Disease *Recurrence rates are high when patients with peptic ulcer disease are not treated for H. pylori infection. The PPIs include esomeprazole, omeprazole, pantoprazole, and rabeprazole. The active metabolites of PPIs form a covalent disulfide link with a cysteinyl residue in the proton pump (H+,K+-ATPase) found in the luminal membrane of gastric parietal cells (see Fig. 28-1). The drugs irreversibly inhibit the proton pump and prevent the secretion of gastric acid for an extended period. The drugs can produce a dose-dependent inhibition of up to 95% of gastric acid secretion, and a single dose can inhibit acid secretion for 1 to 2 days. Hence the PPIs are more efficacious than the H2 blockers for most conditions (see Table 28-1). Sucralfate and misoprostol both protect the gastrointestinal mucosa, but they do so by different means (see Fig. 28-1). As discussed in Chapter 26, misoprostol is a prostaglandin E1 analogue. The drug exerts a cytoprotective effect by inhibiting gastric acid secretion and promoting the secretion of mucus and bicarbonate. It is primarily indicated for the prevention of gastric and duodenal ulcers in patients who are taking NSAIDs on a long-term basis for the treatment of arthritis and other conditions. Because misoprostol is expensive, it is usually reserved for patients at high risk of NSAID-induced ulcers, including the elderly and those with a history of peptic ulcer disease.
Drugs for Gastrointestinal Tract Disorders
Drugs for Peptic Ulcer Disease
Histamine H2 Receptor Antagonists
Chemistry, Mechanisms, and Effects
Pharmacokinetics
DRUG CLASS
DURATION OF ACTION
ADVANTAGES
DISADVANTAGES
Antimicrobial agents
Varies
Heal Helicobacter pylori infection and peptic ulcer when used with acid secretion inhibitor
Microbial resistance increasing (e.g., clarithromycin resistance)
Cytoprotective drugs (sucralfate)*
6-12 hr
Few adverse effects; useful when other drugs not tolerated
Limited utility for H. pylori–induced ulcers; can impair absorption of other drugs
Gastric antacids
3-4 hr
Few adverse effects; rapid acting
Only used for symptomatic relief
Histamine H2 receptor antagonists*
12 hr
Few adverse effects; well tolerated
Not as effective as PPIs
Proton pump inhibitors (PPIs)*
24-48 hr
Most efficacious acid inhibitors
More adverse effects than other drugs
Proton Pump Inhibitors
Mechanisms and Effects
Cytoprotective Drugs
Misoprostol
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs for Gastrointestinal Tract Disorders
Only gold members can continue reading. Log In or Register to continue