Chapter 37 Drugs and Substance Abuse, Addiction, and Treatment
| Abbreviations | |
|---|---|
| AIDS | Acquired immunodeficiency syndrome |
| CNS | Central nervous system |
| DA | Dopamine |
| GABA | γ-Aminobutyric acid |
| GHB | γ-Hydroxybutyrate |
| 5-HT | Serotonin |
| IV | Intravenous |
| LSD | d-Lysergic acid diethylamide |
| MDMA | Methylenedioxymethamphetamine |
| NAcc | Nucleus accumbens |
| NE | Norepinephrine |
| NMDA | N-methyl-D-aspartate |
| NRT | Nicotine replacement therapy |
| PCP | Phencyclidine |
| THC | Tetrahydrocannabinol |
| VTA | Ventral tegmental area |
Therapeutic Overview
In a 2006 survey conducted by the U.S. Substance Abuse and Mental Health Services Administration, more than 20 million Americans aged 12 and older had used illicit drugs in the month before the survey, representing more than 8% of the population. The most commonly used illicit drug was marijuana, followed by prescription pain relievers, cocaine, stimulants, and the hallucinogens (Table 37-1). In addition, more than 50% of Americans used ethanol, with 23% reporting binge drinking (five or more drinks on one occasion) and nearly 7% reporting heavy drinking (binge drinking on at least five occasions) during the past month. Nearly 73 million Americans use some form of tobacco.
TABLE 37–1 Prevalence of Illicit Drug Use in the Unites States in 2006*
| Marijuana | 14.8 |
| Prescription pain relievers | 5.2 |
| Cocaine | 2.4 |
| Stimulants | 1.2 |
| Hallucinogens | 1.0 |
| Inhalants | 0.76 |
* Data from the U.S. Substance Abuse and Mental Health Services Administration; numbers represent millions of persons.
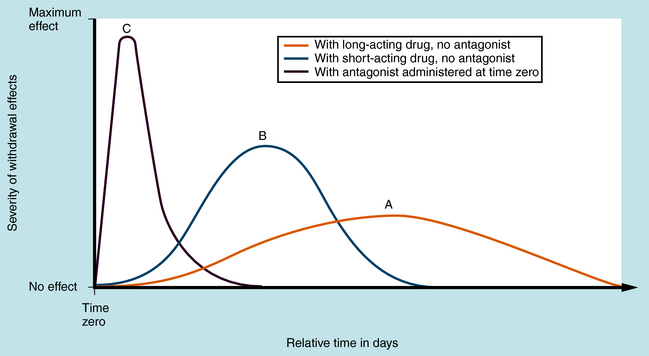
Dependence is characterized by physiological or behavioral changes after discontinuation of drug use, effects that are reversible on resumption of drug administration. Psychological dependence is characterized by intense craving and compulsive drug-seeking behavior. Abused substances often possess reinforcing effects accompanied by intense euphoria and feelings of well-being that foster their continued use. This is particularly true of stimulants such as cocaine and amphetamine. Physical dependence is associated with characteristic withdrawal signs upon cessation of drug administration. The withdrawal syndrome is similar for drugs within a pharmacological class but differs between classes. Its time course varies according to the rate of elimination of the drugs or their active metabolites. Withdrawal from long-acting drugs has a delayed onset, is relatively mild, and occurs over many days or weeks (Fig. 37-1, A), whereas withdrawal from more rapidly inactivated or eliminated drugs is more intense but of shorter duration (Fig. 37-1, B). Typically, physical dependence occurs when substances are used over extended times—usually days, weeks, or months. With repeated use, dependence becomes increasingly severe. Normally, occasional drug use does not result in clinically significant withdrawal. Spontaneous withdrawal occurs on cessation of drug taking. Precipitated withdrawal occurs when an antagonist is administered to displace the drug from its receptors, causing more rapid and severe effects (Fig. 37-1, C). An example is the administration of the opioid antagonist naltrexone to heroin-dependent individuals.
| Therapeutic Overview | |
|---|---|
| Cannabinoids | Hashish, marijuana |
| Depressants | Barbiturates, benzodiazepines, ethanol, GHB, methaqualone |
| Dissociative compounds | PCP, ketamine |
| Hallucinogens | LSD, mescaline, psilocybin |
| Opioids | Codeine, fentanyl, heroin, hydrocodone, hydromorphone, meperidine, morphine, opium, oxycodone |
| Stimulants | Amphetamine, cocaine, MDMA, methamphetamine, methylphenidate, nicotine |
| Anabolic steroids | Nandrolone, oxandrolone, oxymetholone, stanozolol, testosterone |
| Inhalants | Volatile solvents (toluene), gases (N2O), nitrites (amyl nitrite) |
Mechanisms of Action
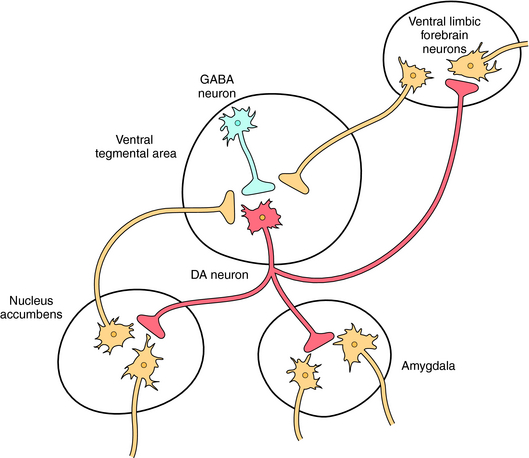
Several pharmacological classes of abused drugs including the cannabinoids, depressants, opioids, and the stimulants all share the ability to activate the mesolimbic dopamine (DA) “reward” pathway in the brain (see Fig. 27-8). These agents either directly activate these dopaminergic neurons or alter the activity of other neurotransmitters such as acetylcholine, γ-aminobutyric acid (GABA), glutamate, serotonin (5-HT), and norepinephrine (NE), which modulate the activity of these neurons. A diagram of ventral tegmental area (VTA)-nucleus accumbens (NAcc) dopamine neurons and pathways affecting the activity of these neurons is shown in Figure 37-2.
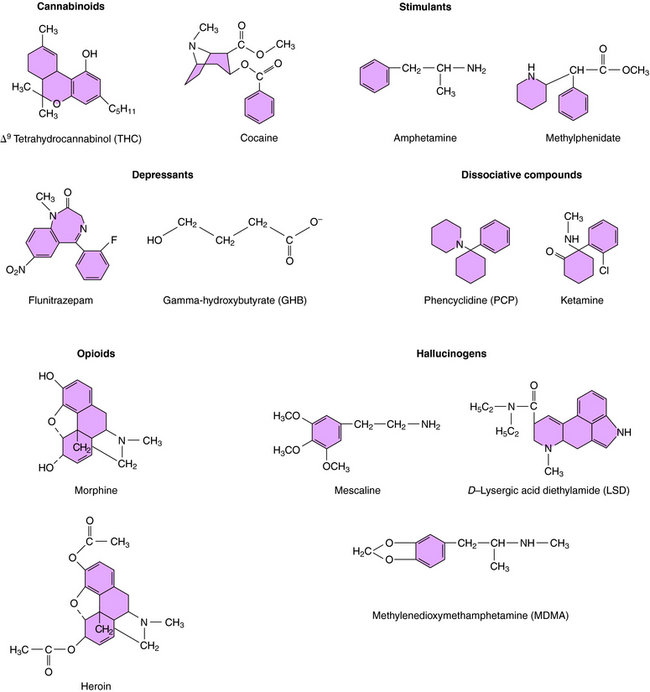
Marijuana (cannabis) is the dried leaf material, buds, and flowering tops from the common hemp plant Cannabis sativa. It has a variety of names including “pot,” “weed,” “grass,” and “maryjane.” Hashish is the dried resinous material exuded by mature plants. Cannabis is the most commonly abused illegal drug in the United States (see Table 37-1). Its major active chemical is Δ9-tetrahydrocannabinol (Δ9-THC; Fig. 37-3). Δ9-THC and related molecules are termed cannabinoids and exert their effects by binding to specific CB1 and CB2 cannabinoid G protein-coupled receptors (see Chapter 1). CB1 receptors are expressed in the brain and gastrointestinal tract and CB2 receptors in the periphery and immune system. The endogenous ligand for these receptors is anandamide, a long-chain arachidonic acid derivative.
CB1 receptors are found in high levels in the cerebellum (coordination of movement), cerebral cortex (cognitive functions), hippocampus (learning and memory), VTA and NAcc (rewarding effects), hypothalamus (satiety/feeding area), and basal ganglia (control of movement). The cannabinoids activate CB1 receptors in both the VTA and NAcc and increase the firing rate of VTA-NAcc neurons. Cannabinoids also increase corticotropin-releasing factor in the amygdala, a common action of many rewarding drugs.
CNS depressants such as barbiturates, non-barbiturate sedatives, and benzodiazepines enhance inhibitory GABA transmission by enhancing the action of endogenous GABA at GABAA receptors (see Chapter 31). Flunitrazepam is a particularly notoriously abused benzodiazepine known as “roofies” or “rophies.”
GABA interneurons in the VTA express GABAA receptors that normally function to tonically suppress the firing of DA neurons (see Fig. 37-2). GABAA receptors are also located on DA cell bodies in the VTA, but these receptors lack α1 subunits and thus are a different subunit composition than those expressed by the GABA neurons. Studies suggest that the depressants, by hyperpolarizing GABA interneurons in the VTA, produce a disinhibition of mesolimbic DA neurons, thereby increasing DA release.
GHB, which is produced endogenously at low levels during GABA metabolism, also belongs in this group (see Fig. 37-3) and is commonly called “liquid ecstasy,” “G,” “grievous bodily harm,” or “Georgia Home Boy.” Studies suggest that GHB interacts with specific binding sites on GABAB receptors, which are present on both GABA interneurons and DA neurons in the VTA, the former more sensitive to GHB than the latter. At low concentrations reflecting those used by the typical abuser, GHB is thought to activate only the receptors expressed by the GABA neurons, thereby inhibiting GABA activity, promoting DA release.
Alcohol is also a CNS depressant that activates the mesolimbic DA pathway. Although several mechanisms have been postulated to be involved in the actions of ethanol including effects of GABAA receptors (see Chapter 32), recent studies suggest that the ability of ethanol to promote DA release in the NAcc may involve its ability to release endocannabinoids and activate CB1 receptors. Further studies are warranted to discern the specific cellular mechanisms mediating the rewarding effects of alcohol.
Opiates are compounds isolated from the opium poppy that act at opioid receptors, whereas opioids are any synthetic or natural compounds that interact with opioid receptors; however, these terms are often used interchangeably. The two principal naturally occurring opiates are morphine and codeine. Heroin (“H” or “smack”), which is 3-,6-diacetylmorphine (Fig. 37-3), is the most commonly abused opioid and is approximately three times more potent than morphine, but the two have very similar effects. Heroin is metabolized to 6-acetylmorphine and morphine to exert its effects. Codeine, which is 3-methoxymorphine, is also demethylated to the more potent morphine by cytochrome P450 enzymes (see Chapter 2). The isoform involved is genetically polymorphic, and persons with mutated forms are unresponsive to codeine. Other synthetic opioids are widely available and abused, often as diverted prescription medications.
The reinforcing actions of the opioids are mediated by μ opioid receptors on GABA interneurons in the VTA, which inhibit GABAergic inhibitory activity (see Chapter 36).
The stimulant drugs are sympathomimetic amines that act on the CNS by enhancing NE and DA neurotransmission. Cocaine (“coke,” “snow,” “blow,” or “crack” for the free base; see Fig. 37-3) is the active ingredient of the South American coca bush. Amphetamines are structurally related to catecholamine neurotransmitters and ephedrine (see Chapter 11) and include amphetamine, N-methylamphetamine (methamphetamine, known as “speed,” “meth,” or “ice”), and others such as methylphenidate.
The reinforcing effects of stimulants arise from enhanced neurotransmission at dopaminergic synapses in the mesolimbic and mesocortical pathways (see Fig. 37-2). Cocaine binds to DA transporters and blocks the reuptake of DA, increasing its synaptic concentration. Amphetamines also act on DA transporters to enhance DA release and may increase its concentrations by inhibiting destruction by monoamine oxidase. Amphetamines may also directly activate postsynaptic receptors. Nicotine interacts directly with nicotinic receptors on DA neurons in the VTA to increase the firing of these neurons.
PCP (“angel dust”) and ketamine (“K” or “special K”) were originally developed as anesthetics (see Fig. 37-3). Ketamine is still used for changing burn dressings, for anesthesia in children (see Chapter 35), and for short-duration anesthesia in veterinary medicine. PCP is not used therapeutically because of the severity of emergence delirium in patients. Dextromethorphan (“DXM” or “robo”) is an over-the-counter cough suppressant and when taken in high doses, produces effects similar to those of PCP and ketamine.
PCP, ketamine, and high-dose dextromethorphan produce their effects through a use-dependent noncompetitive antagonism at excitatory glutamate N-methyl-D-aspartate (NMDA) receptors throughout the CNS (see Chapter 1).
Hallucinogens produce changes in mood, thought, and sensory perception such that colors, sounds, and smells are intensified. Because of the latter actions, these compounds are referred to as psychedelic or psychotomimetic agents. The hallucinogens have no recognized medical uses. Abused hallucinogens fall into two chemical classes, the substituted phenethylamines, of which mescaline is the prototype, and the indoleamines, of which D-lysergic acid diethylamide (LSD) is the prototype (see Figure 37-3). Others hallucinogens include psilocybin (from mushrooms) and dimethyltryptamine.
MDMA (“ecstasy” or “XTC”) is a substituted amphetamine (see Fig. 37-3) and has properties of both a hallucinogen and a stimulant. MDMA acts to increase the release of DA and 5-HT. Methylenedioxyamphetamine is a related compound.
Anabolic steroids are synthetic substances related to androgens, male sex hormones. These drugs promote growth of male sexual characteristics and have important clinical uses (see Chapter 41). However, steroid abuse is widespread in body-building and sports for enhancement of skeletal muscle growth. Abused steroids include testosterone itself as well as synthetic compounds, such as nandrolone, oxandrolone, oxymetholone, and stanozolol. The mechanism of action of these compounds is discussed in Chapter 41.