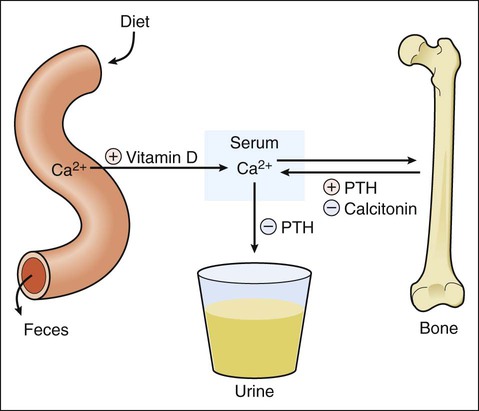
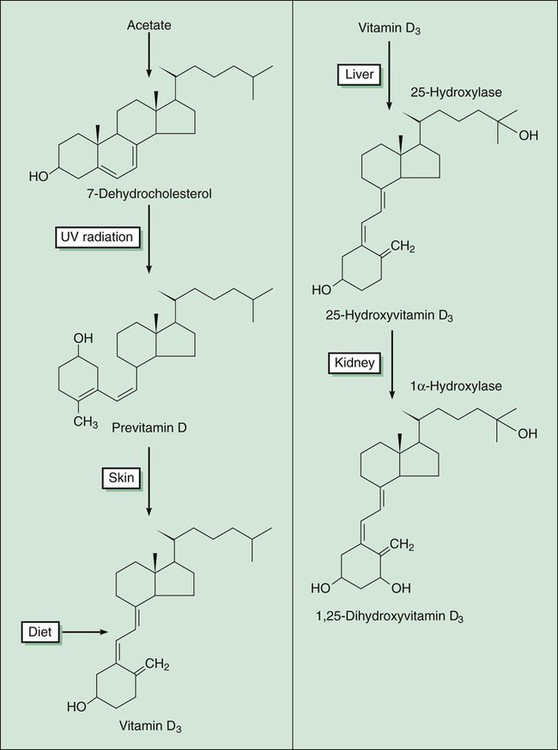
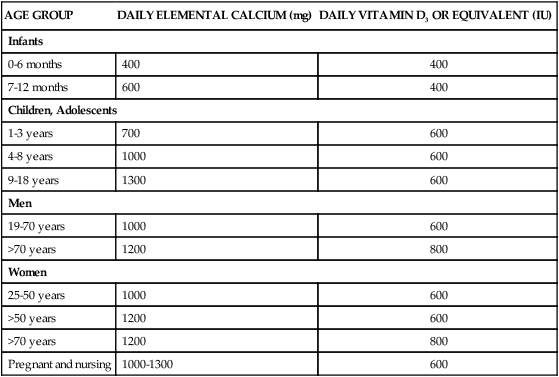
Control of the extracellular calcium concentration depends on hormonal regulation of the absorption and excretion of calcium, as well as on the exchange of ionized calcium with bone. As shown in Figure 36-1, the hormones involved in this regulation include vitamin D, parathyroid hormone (PTH), and calcitonin. PTH has four actions that increase the extracellular calcium concentration. First, it stimulates resorption of calcium by renal tubules. Second, it decreases resorption of phosphate by renal tubules. This decreases the extracellular phosphate concentration, which in turn tends to increase the extracellular calcium concentration. Third, PTH stimulates the hydroxylation of vitamin D in the kidneys (Fig. 36-2). Fourth, PTH increases bone resorption by stimulating osteoclast activity, which enables bone calcium to enter the extracellular pool. Bone remodeling (Fig. 36-3) consists of a sequence of events involving the dynamic interaction of osteoclasts (bone-resorbing cells) and osteoblasts (bone-forming cells). The recruitment and activation of osteoclasts are mediated by compounds released from osteoblasts and peripheral leukocytes called bone cell cytokines. The cytokines include interleukins, tumor necrosis factor, colony-stimulating factors, and other factors that alter gene expression. After the osteoclasts are activated, they adhere to the bone surface and release hydrogen ions and proteases to break down the bone. The destroyed bone releases growth factors that increase osteoblast production and decrease osteoclast activity. The osteoblasts then lay down new bone in the cavity created by osteoclasts. The entire remodeling process takes about 100 days on average. Trabecular bone (internal, spongy, cancellous bone) undergoes more remodeling than cortical (hard compact outer layer) bone (25% versus 3% annually). Osteoporosis, the most common bone disorder, is characterized by a gradual reduction in bone mass that weakens bones and leads to the occurrence of fractures after minimal trauma, such as falls. Vertebral fractures are the most frequent type of fracture in patients with postmenopausal osteoporosis, a disorder partly caused by decreased estrogen secretion in this population; hip, humerus, and pelvis fractures are also major causes of immobility, morbidity, and mortality in older persons. In the United States the annual cost of osteoporotic hip fractures is currently about $11 billion, and the cost is projected to rise to $240 billion by the year 2040 if more effective methods of prevention and treatment are not developed and implemented (Box 36-1). An adequate intake of calcium and vitamin D is essential for optimal bone formation in children and to prevent osteoporosis in adults. All persons should be encouraged by health professionals to meet the recommendations of the Institute of Medicine of the National Academies of the United States, or similar agencies in other countries, for daily calcium and vitamin D intake (Table 36-1). These recommendations can be met by ingesting calcium-rich foods, which are primarily dairy products, and by taking oral calcium and vitamin D supplements if dietary intake is inadequate. Studies have shown that adequate calcium and vitamin D intake prevents loss of bone mass and osteoporosis. For example, nursing-home residents who were given 800 International Units (IU) of vitamin D3 and 1200 mg of calcium were found to have an increased bone density and a decreased incidence of hip and nonvertebral fractures in comparison with those who were given placebos. In another study, administration of vitamin D3 was found to decrease the incidence of vertebral and nonvertebral fractures in women with previous fractures. TABLE 36-1 Recommended Dietary Allowances for Calcium and Vitamin D* *Food and Nutrition Board, Institute of Medicine of the National Academies. In the United States, it is estimated that two thirds of women age 18 and over have an inadequate calcium intake, which predisposes them to postmenopausal osteoporosis. Most people get 300 mg of calcium daily in their diet from nondairy sources, and adding two servings of dairy products typically brings the total calcium intake to 900 mg. Supplementing with just 300 mg of calcium or adding another high-calcium dairy product would provide about 1200 mg and thereby fulfill the daily requirement for all adults and children except adolescents (see Table 36-1).
Drugs Affecting Calcium and Bone
Overview
Calcium and Bone Metabolism
Bone Disorders
Calcium and Vitamin D
AGE GROUP
DAILY ELEMENTAL CALCIUM (mg)
DAILY VITAMIN D3 OR EQUIVALENT (IU)
Infants
0-6 months
400
400
7-12 months
600
400
Children, Adolescents
1-3 years
700
600
4-8 years
1000
600
9-18 years
1300
600
Men
19-70 years
1000
600
>70 years
1200
800
Women
25-50 years
1000
600
>50 years
1200
600
>70 years
1200
800
Pregnant and nursing
1000-1300
600
Calcium
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs Affecting Calcium and Bone
Only gold members can continue reading. Log In or Register to continue