38
DNA Nonenveloped Viruses
CHAPTER CONTENTS
ADENOVIRUSES
Diseases
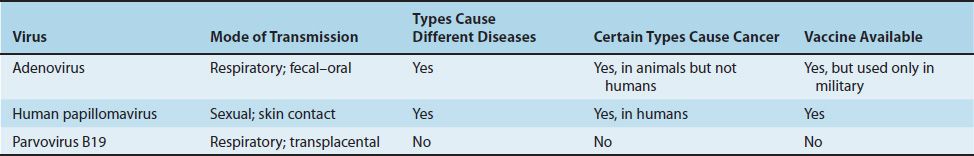
Adenoviruses cause a variety of upper and lower respiratory tract diseases such as pharyngitis, conjunctivitis (“pink eye”), the common cold, and pneumonia. Keratoconjunctivitis, hemorrhagic cystitis, and gastroenteritis also occur. Some adenoviruses cause sarcomas in rodents. Table 38–1 describes some of the important clinical features of adenoviruses and compares them with features of the other two medically important viruses in this chapter, human papillomavirus (HPV) and parvovirus B19.
Important Properties
Adenoviruses are nonenveloped viruses with double-stranded linear DNA and an icosahedral nucleocapsid. They are the only viruses with a fiber protruding from each of the 12 vertices of the capsid. The fiber is the organ of attachment and is a hemagglutinin. When purified free of virions, the fiber is toxic to human cells.
There are 41 known antigenic types; the fiber protein is the main type-specific antigen. All adenoviruses have a common group-specific antigen located on the hexon protein.
Certain serotypes of human adenoviruses (especially 12, 18, and 31) cause sarcomas at the site of injection in laboratory rodents such as newborn hamsters. There is no evidence that adenoviruses cause tumors in humans.
Summary of Replicative Cycle
After attachment to the cell surface via its fiber, the virus penetrates and uncoats, and the viral DNA moves to the nucleus. Host cell DNA-dependent RNA polymerase transcribes the early genes, and splicing enzymes remove the RNA representing the introns, resulting in functional mRNA. (Note that introns and exons, which are common in eukaryotic DNA, were first described for adenovirus DNA.) Early mRNA is translated into nonstructural proteins in the cytoplasm. After viral DNA replication in the nucleus, late mRNA is transcribed and then translated into structural virion proteins. Viral assembly occurs in the nucleus, and the virus is released by lysis of the cell, not by budding.
Transmission & Epidemiology
Adenoviruses are transmitted by several mechanisms: aerosol droplet, fecal–oral route, and direct inoculation of conjunctivas by tonometers or fingers. The fecal–oral route is the most common mode of transmission among young children and their families. Many species of animals are infected by strains of adenovirus, but these strains are not pathogenic for humans.
Adenovirus infections are endemic worldwide, but outbreaks occur among military recruits, apparently as a result of the close living conditions that facilitate transmission. Certain serotypes are associated with specific syndromes (e.g., types 3, 4, 7, and 21 cause respiratory disease, especially in military recruits; types 8 and 19 cause epidemic keratoconjunctivitis; types 11 and 21 cause hemorrhagic cystitis; and types 40 and 41 cause infantile gastroenteritis).
Pathogenesis & Immunity
Adenoviruses infect the mucosal epithelium of several organs (e.g., the respiratory tract [both upper and lower], the gastrointestinal tract, and the conjunctivas). Immunity based on neutralizing antibody is type-specific and lifelong.
In addition to acute infection leading to death of the cells, adenoviruses cause a latent infection, particularly in the adenoidal and tonsillar tissues of the throat. In fact, these viruses were named for the adenoids, from which they were first isolated in 1953.
Clinical Findings
In the upper respiratory tract, adenoviruses cause such infections as pharyngitis, pharyngoconjunctival fever, and acute respiratory disease, characterized by fever, sore throat, coryza (runny nose), and conjunctivitis. In the lower respiratory tract, they cause bronchitis and atypical pneumonia. Hematuria and dysuria are prominent in hemorrhagic cystitis. Gastroenteritis with nonbloody diarrhea occurs mainly in children younger than 2 years of age. Most adenovirus infections resolve spontaneously. Approximately half of all adenovirus infections are asymptomatic.
Laboratory Diagnosis
The most frequent methods of diagnosis are isolation of the virus in cell culture and detection of a fourfold or greater rise in antibody titer. Complement fixation and hemagglutination inhibition are the most important serologic tests.
Treatment
There is no antiviral therapy.
Prevention
Three live, nonattenuated vaccines against serotypes 4, 7, and 21 are available but are used only by the military. Each of the three vaccines is monovalent (i.e., each contains only one serotype). The viruses are administered separately because they interfere with each other when given together. The vaccines are delivered in an enteric-coated capsule, which protects the live virus from inactivation by stomach acid. The virus infects the gastrointestinal tract, where it causes an asymptomatic infection and induces immunity to respiratory disease. This vaccine is not available for civilian use.
Epidemic keratoconjunctivitis is an iatrogenic disease, preventable by strict asepsis and hand washing by health care personnel who examine eyes.
PAPILLOMAVIRUSES
Diseases
Human papillomavirus causes papillomas, which are benign tumors of squamous cells (e.g., warts on the skin). Some HPV types, especially types 16 and 18, cause carcinoma of the cervix, penis, and anus.
Important Properties
Papillomaviruses are nonenveloped viruses with double-stranded circular DNA and an icosahedral nucleocapsid. Two of the early genes, E6 and E7, are implicated in carcinogenesis. They encode proteins that inactivate proteins encoded by tumor suppressor genes in human cells (e.g., the p53 gene and the retinoblastoma [RB] gene, respectively). Inactivation of the p53 and RB proteins is an important step in the process by which a normal cell becomes a cancer cell.
There are at least 100 types of papillomaviruses, classified primarily on the basis of DNA restriction fragment analysis. There is a pronounced predilection of certain types to infect certain tissues. For example, skin warts are caused primarily by HPV-1 through HPV-4, whereas genital warts are usually caused by HPV-6 and HPV-11. Approximately 30 types of HPV infect the genital tract.
Summary of Replicative Cycle
Little is known of the specifics of viral replication, because the virus grows poorly, if at all, in cell culture. In human tissue, infectious virus particles are found in the terminally differentiated squamous cells rather than in the basal cells. Note that HPV initially infects the cells of the basal layer in the skin, but no virus is produced by those cells. Rather, infectious virions are produced by squamous cells on the surface, which enhances the likelihood that efficient transmission will occur.
In malignant cells, viral DNA is integrated into host cell DNA in the vicinity of cellular proto-oncogenes, and E6 and E7 are overexpressed. However, in latently infected, nonmalignant cells, the viral DNA is episomal, and E6 and E7 are not overexpressed. This difference occurs because another early gene, E2, controls E6 and E7 expression. The E2 gene is functional when the viral DNA is episomal but is inactivated when it is integrated.
Transmission & Epidemiology
Papillomaviruses are transmitted primarily by skin-to-skin contact and by genital contact. Genital warts are among the most common sexually transmitted diseases. Skin warts are more common in children and young adults and tend to regress in older adults. HPV transmitted from an infected mother to the neonate during childbirth causes warts in the mouth and in the respiratory tract, especially on the larynx, of the infant. Many species of animals are infected with their own types of papillomaviruses, but these viruses are not an important source of human infection.
Pathogenesis & Immunity
Papillomaviruses infect squamous epithelial cells and induce within those cells a characteristic cytoplasmic vacuole. These vacuolated cells, called koilocytes, are the hallmark of infection by these viruses. Most warts are benign and do not progress to malignancy. However, HPV infection is associated with carcinoma of the uterine cervix and penis. The proteins encoded by viral genes E6 and E7 interfere with the growth-inhibitory activity of the proteins encoded by the p53 and RB tumor suppressor genes and thereby contribute to oncogenesis by these viruses. The E6 and E7 proteins of HPV-16 bind more strongly to p53 and RB proteins than the E6 and E7 proteins of HPV types not implicated in carcinomas—a finding that explains why HPV-16 causes carcinomas more frequently than the other types of HPV.
Both cell-mediated immunity and antibody are induced by viral infection and are involved in the spontaneous regression of warts. Immunosuppressed patients (e.g., patients with acquired immunodeficiency syndrome [AIDS]) have more extensive warts, and women infected with human immunodeficiency virus (HIV) have a very high rate of carcinoma of the cervix.
Clinical Findings
Papillomas of various organs are the predominant finding. These papillomas are caused by specific HPV types. For example, skin and plantar warts (Figure 38–1) are caused primarily by HPV-1 through HPV-4, whereas genital warts (condylomata acuminata) (Figure 38–2) are caused primarily by HPV-6 and HPV-11. HPV-6 and HPV-11 also cause respiratory tract papillomas, especially laryngeal papillomas, in young children.
FIGURE 38–1 Papillomas (warts) on finger—note dry, raised verrucous lesions caused by human papillomavirus. (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree