NEPHRON FUNCTION AND SITES OF DRUG ACTION
Sodium and other electrolytes are reabsorbed into the circulation at various sites throughout the nephron by active and passive processes that involve ion channels, transport proteins, and the sodium pump (Na+,K+-ATPase). Ion channels are unique membrane proteins through which a specific ion moves across the cell membrane in the direction that is determined by the electrochemical gradient for the ion. The transport proteins include symporters, which transport two or more ions in the same direction, and antiporters, which transport ions in opposite directions across cell membranes. Most diuretics act by blocking a specific ion channel or transporter in the tubular epithelial cells. The effects of diuretics on ion reabsorption and secretion in the nephron are illustrated in Box 13–1.
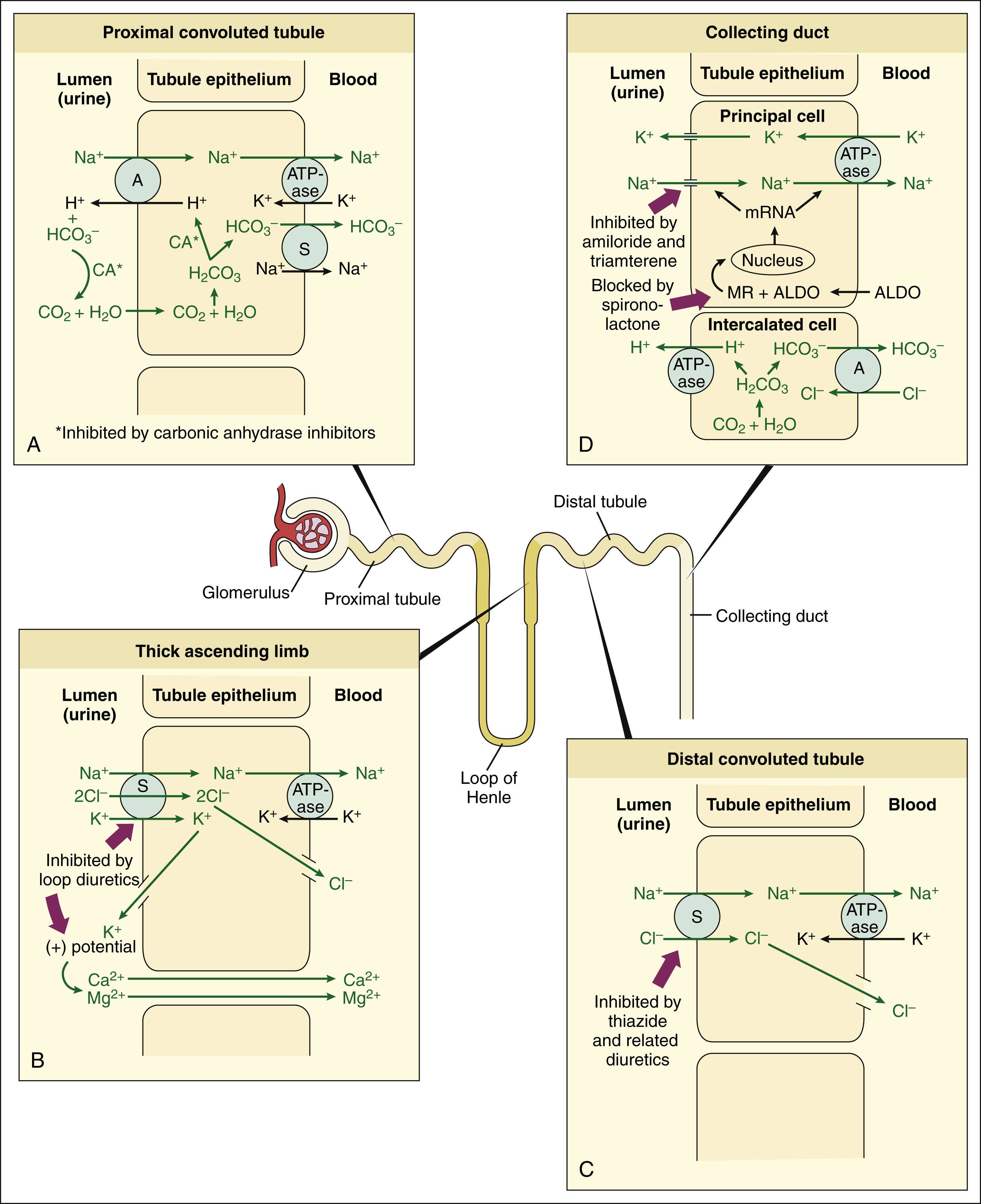
BOX 13–1 SITES AND MECHANISMS OF ACTION OF DIURETICS
In the proximal tubule (A), carbonic anhydrase catalyzes the reversible conversion of hydrogen ion and bicarbonate to carbon dioxide and water, thereby enabling the reabsorption of sodium bicarbonate. This process is inhibited by carbonic anhydrase inhibitors, such as acetazolamide.
In the thick ascending limb of the loop of Henle (B), the Na+,K+,2Cl− symporter transports sodium, potassium, and chloride ions into the tubular cells, and then sodium is transferred to the interstitial fluid by the sodium pump. Potassium back-diffuses into the lumen and contributes to the positive transepithelial potential that drives paracellular calcium and magnesium reabsorption. By inhibiting the symporter, the loop diuretics reduce the back-diffusion of potassium and increase the excretion of calcium and magnesium.
In the distal tubule (C), sodium is transported into tubular epithelial cells by the Na+,Cl− symporter and then is transferred to interstitial fluid by the sodium pump. The Na+,Cl− symporter is inhibited by thiazide and related diuretics.
In the collecting duct (D), sodium enters the principal cells through sodium channels. Sodium is then transferred into the interstitial fluid by the sodium pump, while potassium is pumped in the opposite direction and then moves through potassium channels into the tubular fluid. Aldosterone stimulates these processes by increasing the synthesis of messenger RNA that encodes for sodium channel and sodium pump proteins. The potassium-sparing diuretics exert their effects via two mechanisms: amiloride and triamterene inhibit the entrance of sodium into the principal cells, whereas spironolactone blocks the mineralocorticoid receptor and thereby inhibits sodium reabsorption and potassium secretion.
A = antiporter; ALDO = aldosterone; CA = carbonic anhydrase; MR = mineralocorticoid receptor; mRNA = messenger RNA; S = symporter.
Glomerular Filtration
Urine formation begins with glomerular filtration, a process in which an ultrafiltrate of blood is forced out of the glomerular capillaries and into the nephron lumen by the hydrostatic pressure in these capillaries. In healthy individuals, this filtrate is essentially free of blood cells and plasma proteins. Digitalis glycosides and other cardiac stimulants can indirectly cause diuresis by increasing cardiac output, renal blood flow, and the glomerular filtration rate. The renal actions of these drugs are described in greater detail in Chapter 12. The diuretic drugs described in this chapter do not increase the glomerular filtration rate, and some of them may indirectly reduce it by decreasing plasma volume and renal blood flow.
Proximal Tubule
The proximal tubule is an important site of tubular reabsorption and secretion. Essentially all of the filtered glucose, amino acids, and other organic solutes are reabsorbed in the early portion of the proximal tubule. About 85% of filtered sodium bicarbonate is reabsorbed in the proximal tubule, and this reabsorption is inhibited by a class of diuretics known as carbonic anhydrase inhibitors. For reasons described later in this chapter, these drugs are relatively weak diuretics and are seldom used for this purpose, although their actions are useful in the treatment of glaucoma and other conditions.
About 40% of filtered sodium chloride is reabsorbed in the proximal tubule. This is a relatively unimportant site of diuretic action, however, because inhibition of sodium chloride reabsorption in the proximal tubule almost invariably leads to increased sodium chloride reabsorption in more distal segments of the nephron.
The proximal tubule is the major site of the active tubular secretion of organic acids and bases into the nephron lumen, including natural compounds (e.g., uric acid) and drugs (e.g., penicillins). The loop diuretics and thiazide diuretics are also secreted by proximal tubular cells, and then these drugs are carried in the tubular fluid to their site of action in the loop of Henle and the distal tubule, respectively.
Loop of Henle
The loop of Henle is responsible for the reabsorption of about 35% of the filtered sodium chloride. This segment also participates in the formation of a concentrated urine by transporting sodium chloride into the surrounding interstitium, where a hypertonic interstitial fluid is formed. This fluid attracts water from the collecting duct under the influence of antidiuretic hormone. The reabsorption of sodium from the thick ascending limb is inhibited by loop diuretics, which produce a greater diuretic effect than any other class of diuretics.
Distal Tubule
The early distal tubule is responsible for the reabsorption of 5% to 10% of the filtered sodium chloride, and this reabsorption is inhibited by thiazide and related diuretics. Because a relatively small percentage of sodium reabsorption can be inhibited by these drugs, they have a more modest diuretic action than the loop diuretics.
Collecting Duct
The collecting duct serves to adjust the final composition and volume of urine to regulate extracellular fluid composition and pH and thereby maintain physiologic homeostasis. The collecting duct is the site of action of aldosterone and antidiuretic hormone. Aldosterone is a mineralocorticoid that increases sodium reabsorption, thereby promoting sodium retention by the body. Antidiuretic hormone increases the reabsorption of water from the collecting duct, which conserves body water and concentrates the urine. The actions of these hormones are partly responsible for maintaining plasma volume and osmolality in the normal range.
The collecting duct is responsible for the reabsorption of about 3% of the filtered sodium chloride. This reabsorption is coupled with potassium and hydrogen excretion. The potassium-sparing diuretics inhibit these processes and are used to reduce potassium excretion and prevent hypokalemia.
DIURETIC AGENTS
Thiazide and Related Diuretics
The thiazides and related diuretics are the most commonly used diuretics. They are orally efficacious, have a moderate natriuretic effect, and have few adverse effects in most patients.
Drug Properties
CHEMISTRY AND PHARMACOKINETICS
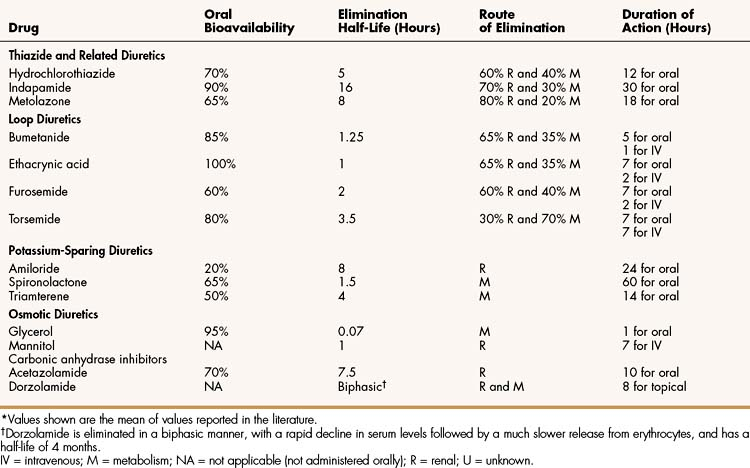
Thiazides are sulfonamide compounds that contain a benzothiadiazide (thiazide) moiety. They exhibit good oral bioavailability and were the first orally administered diuretics to be widely used for the treatment of hypertension and edema. Thiazides are actively secreted into the nephron by proximal tubular cells, and they travel through the nephron lumen to reach their site of action in the distal tubule. Some of the thiazides are partially metabolized before excretion in the urine (Table 13–2).
MECHANISMS AND PHARMACOLOGIC EFFECTS
Thiazide diuretics act primarily on the early portion of the distal tubule to inhibit the Na+,Cl− symporter that participates in the reabsorption of sodium and chloride from this segment of the nephron (see Box 13–1). This action leads to the delivery of a greater volume of sodium chloride-enriched tubular fluid to the late distal tubule and collecting duct, which in turn stimulates the exchange of sodium and potassium at these sites. In the process, a small amount of sodium is reabsorbed as potassium is secreted into urine in the tubules. By this mechanism, thiazides have a kaliuretic effect that leads to hypokalemia in some patients.
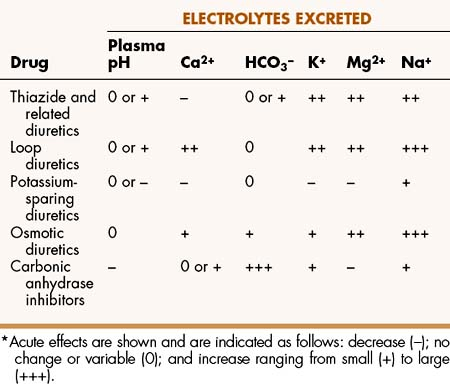
As shown in Table 13–3, thiazides increase magnesium excretion, but (unlike many diuretics) they decrease calcium excretion in the urine. The hypocalciuria induced by thiazides appears to result from decreased expression of calcium transport proteins, including the epithelial calcium channel, calbindin, and the sodium-calcium exchanger protein, in renal tubules. The ability of thiazides to reduce calcium excretion is the basis for their use in the treatment of kidney stones caused by excessive calcium in the urine.
ADVERSE EFFECTS AND INTERACTIONS
Table 13–4 lists the common adverse effects and interactions of thiazides and other diuretics.
TABLE 13–4 Adverse Effects and Drug Interactions of Diuretics
| Drug | Common Adverse Effects | Common Drug Interactions |
|---|---|---|
| Thiazide and Related Diuretics | ||
| Hydrochlorothiazide | Blood cell deficiencies; electrolyte imbalances; and increased blood cholesterol, glucose, or uric acid levels. | Potentiates the diuretic effect of loop diuretics. |
| Indapamide | Electrolyte imbalances and increased blood cholesterol, glucose, or uric acid levels. | Same as hydrochlorothiazide. |
| Metolazone | Blood cell deficiencies; electrolyte imbalances; and increased blood cholesterol or glucose levels. | Same as hydrochlorothiazide. |
| Loop Diuretics | ||
| Bumetanide | Blood cell deficiencies; electrolyte imbalances; hearing impairment; and hypersensitivity reactions. | Diuretic effect decreased by NSAIDs. Administration with ACE inhibitors may cause excessive hypotension. |
| Ethacrynic acid | Blood cell deficiencies; electrolyte imbalances; hearing impairment; and rash. | Diuretic effect decreased by NSAIDs. |
| Furosemide | Blood cell deficiencies; electrolyte imbalances; hearing impairment; hypersensitivity reactions; increased blood cholesterol, glucose, or uric acid levels; and photosensitivity. | Same as bumetanide. |
| Torsemide | Electrolyte imbalances and increased blood cholesterol, glucose, or uric acid levels. | Same as bumetanide. |
| Potassium-Sparing Diuretics | ||
| Amiloride | Blood cell deficiencies; gastrointestinal distress; and hyperkalemia. | Administration with ACE inhibitors or potassium supplements may cause hyperkalemia. Administration with NSAIDs may cause renal failure. |
| Spironolactone | Gynecomastia; hyperkalemia; and impotence. | Administration with ACE inhibitors or potassium supplements may cause hyperkalemia. |
| Triamterene | Same as amiloride. | Same as amiloride. |
| Osmotic Diuretics | ||
| Glycerol | Heart failure; nausea and vomiting; and pulmonary congestion and edema. | Potentiates effects of other diuretics. |
| Mannitol | Same as glycerol. | Same as glycerol. |
| Carbonic Anhydrase Inhibitors | ||
| Acetazolamide | Blood cell deficiencies; drowsiness; hepatic insufficiency; hyperglycemia; hypokalemia; metabolic acidosis; paresthesia, and uremia. | Serum levels of weak bases, such as amphetamine, ephedrine, and quinidine, are increased by CA inhibitors. Serum levels of CA inhibitors are increased by salicylates. |
| Dorzolamide | Bitter taste; blurred vision; ocular discomfort and allergic reactions. | Unknown. |
ACE = angiotensin-converting enzyme; CA = carbonic anhydrase; NSAIDs = nonsteroidal anti-inflammatory drugs.
Thiazide diuretics sometimes cause hypokalemia, particularly in patients whose dietary potassium intake is inadequate. Hypokalemia can eventually lead to hypokalemic metabolic alkalosis (Fig. 13–1). In this disorder, hydrogen ions enter body cells as potassium leaves these cells in an attempt to correct the plasma potassium deficiency. As the plasma potassium level falls, more hydrogen ions are secreted into urine in the tubules in exchange for sodium, and this further contributes to the development of metabolic alkalosis. In cases of hypokalemic metabolic alkalosis, potassium chloride is administered intravenously and orally. Correction of the serum potassium level then leads to correction of the acid-base disturbance as potassium displaces hydrogen ions from body cells and fewer hydrogen ions are secreted by the collecting duct.
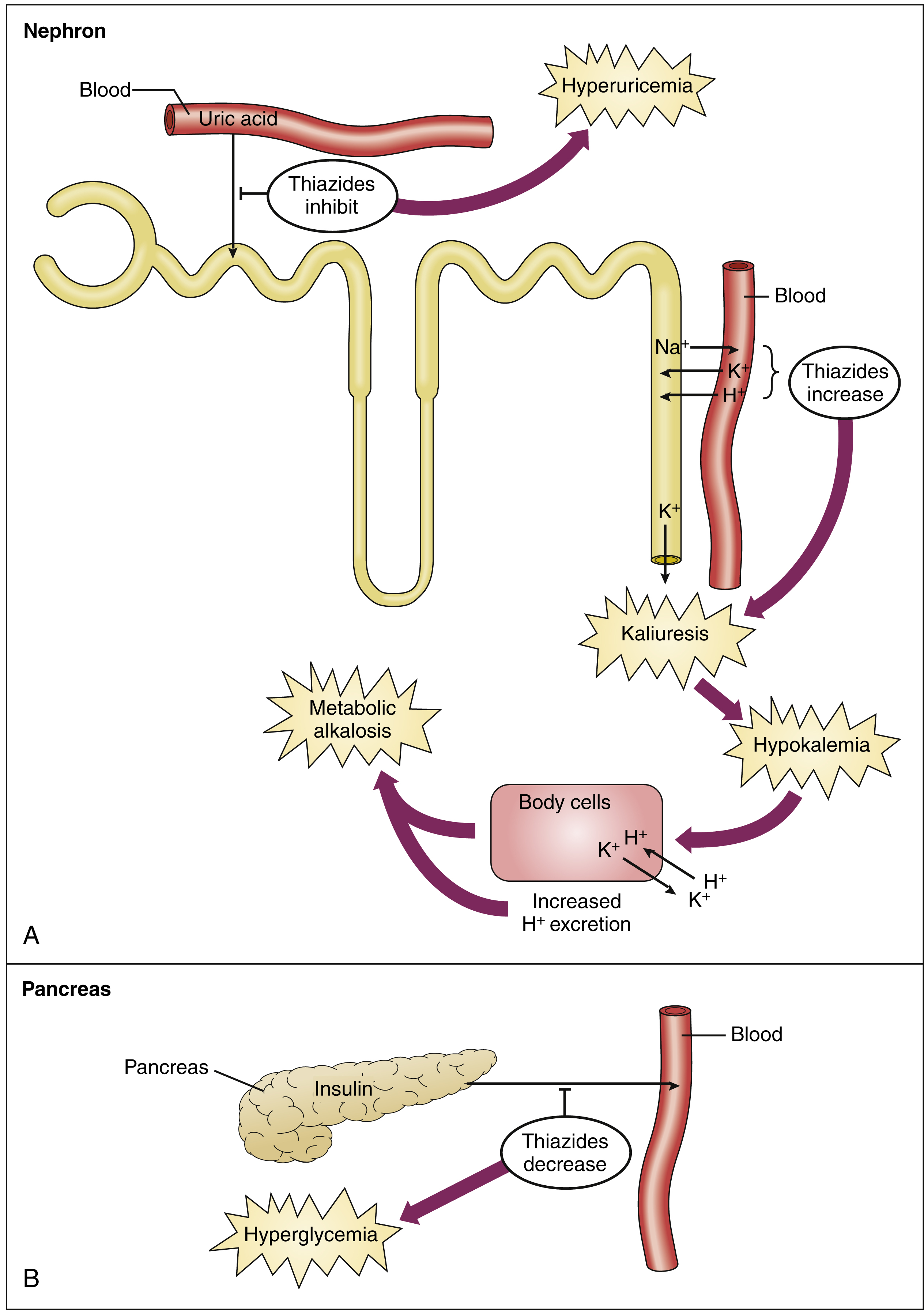
Figure 13–1 Adverse effects of thiazide diuretics. (A) Inhibition of uric acid secretion in the proximal tubule can lead to hyperuricemia and gout. Increased potassium secretion in the collecting duct can cause hypokalemia. Hypokalemia can lead to metabolic alkalosis by promoting the exchange of intracellular potassium for hydrogen ions and by increasing the excretion of hydrogen ions. The increased excretion is caused by lack of availability of potassium for exchange with sodium in the collecting duct. (B) In the presence of hypokalemia, the amount of insulin secreted by the pancreas can be reduced, thereby leading to hyperglycemia. Other mechanisms can also be involved in the development of hyperglycemia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree