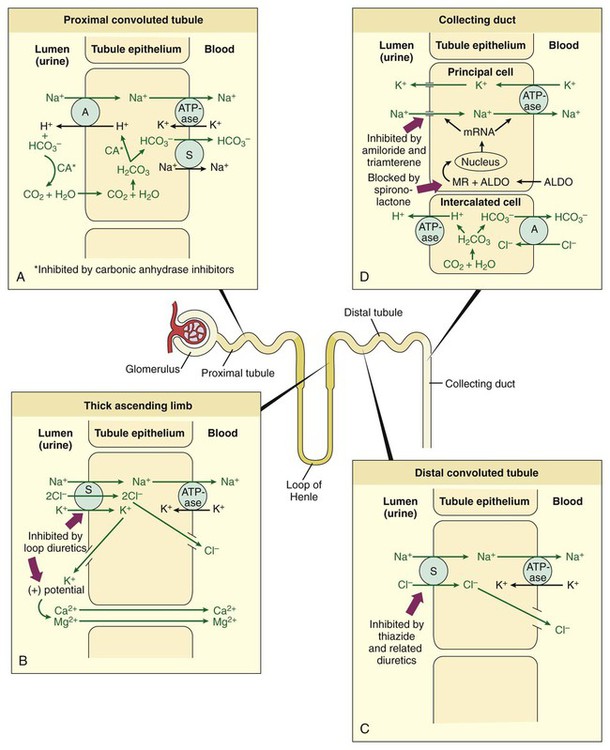
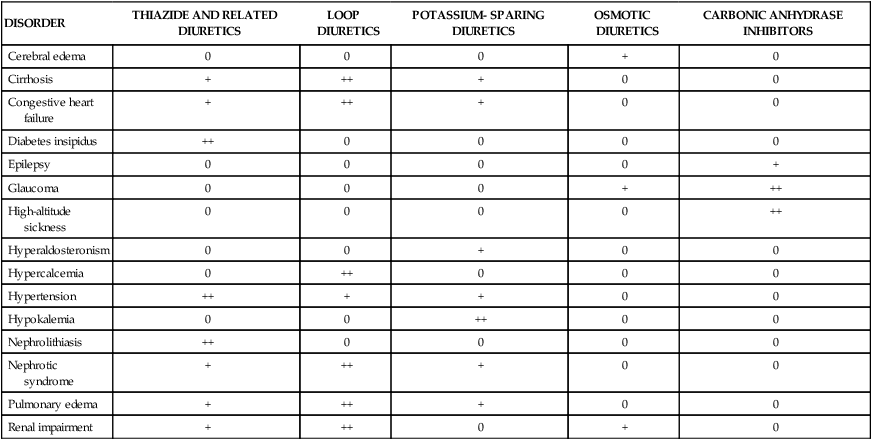
Diuretics are used in the management of edema associated with cardiovascular, renal, and endocrine abnormalities, as well as in the treatment of hypertension, glaucoma, and several other clinical disorders (Table 13-1). The drugs act at various sites in the nephron to cause diuresis (an increase in urine production). Most diuretics inhibit the reabsorption of sodium from the nephron into the circulation and thereby increase natriuresis (the excretion of sodium in the urine). Several types of diuretics also increase kaliuresis (the excretion of potassium in the urine) and affect the excretion of magnesium, calcium, chloride, and bicarbonate ions. TABLE 13-1 Usefulness of Diuretics in the Management of Various Clinical Disorders* Sodium and other electrolytes are reabsorbed into the circulation at various sites throughout the nephron by active and passive processes that involve ion channels, transport proteins, and the sodium pump (Na+,K+-ATPase). Ion channels are unique membrane proteins through which a specific ion moves across the cell membrane in the direction determined by the electrochemical gradient for the ion. The transport proteins include symporters, which transport two or more ions in the same direction, and antiporters, which transport ions in opposite directions across cell membranes. Most diuretics block a specific ion channel or transporter in the tubular epithelial cells. The sites and mechanisms by which diuretics affect ion reabsorption and secretion in the nephron are illustrated in Box 13-1. Urine formation begins with glomerular filtration, a process in which an ultrafiltrate of blood is forced out of the glomerular capillaries and into the nephron lumen by the hydrostatic pressure in these capillaries. In healthy individuals this filtrate is essentially free of blood cells and plasma proteins. Digitalis glycosides and other cardiac stimulants can indirectly cause diuresis by increasing cardiac output, renal blood flow, and the glomerular filtration rate. These drugs are described in greater detail in Chapter 12. The diuretic drugs described in this chapter do not increase the glomerular filtration rate, and some of them may indirectly reduce it by decreasing plasma volume and renal blood flow. Thiazides are sulfonamide compounds and were the first orally administered diuretics to be widely used for the treatment of hypertension and edema. Thiazides exhibit good oral bioavailability and are actively secreted into the nephron by proximal tubular cells, and they travel through the nephron lumen to reach their site of action in the distal tubule. Some of the thiazides are partially metabolized before excretion in the urine (Table 13-2). TABLE 13-2 Pharmacokinetic Properties of Diuretics*
Diuretics
Overview
DISORDER
THIAZIDE AND RELATED DIURETICS
LOOP DIURETICS
POTASSIUM- SPARING DIURETICS
OSMOTIC DIURETICS
CARBONIC ANHYDRASE INHIBITORS
Cerebral edema
0
0
0
+
0
Cirrhosis
+
++
+
0
0
Congestive heart failure
+
++
+
0
0
Diabetes insipidus
++
0
0
0
0
Epilepsy
0
0
0
0
+
Glaucoma
0
0
0
+
++
High-altitude sickness
0
0
0
0
++
Hyperaldosteronism
0
0
+
0
0
Hypercalcemia
0
++
0
0
0
Hypertension
++
+
+
0
0
Hypokalemia
0
0
++
0
0
Nephrolithiasis
++
0
0
0
0
Nephrotic syndrome
+
++
+
0
0
Pulmonary edema
+
++
+
0
0
Renal impairment
+
++
0
+
0
Nephron Function and Sites of Drug Action
Glomerular Filtration
Diuretic Agents
Thiazide and Related Diuretics
Drug Properties
Chemistry and Pharmacokinetics
DRUG
ORAL BIOAVAILABILITY
ELIMINATION HALF-LIFE (HOURS)
ROUTE OF ELIMINATION
DURATION OF ACTION (HOURS)
Thiazide and Related Diuretics
Hydrochlorothiazide
70%
5
60% R and 40% M
12 for oral
Indapamide
90%
16
70% R and 30% M
30 for oral
Metolazone
65%
8
80% R and 20% M
18 for oral
Loop Diuretics
Bumetanide
85%
1.25
65% R and 35% M
5 for oral
1 for IV
Ethacrynic acid
100%
1
65% R and 35% M
7 for oral
2 for IV
Furosemide
60%
2
60% R and 40% M
7 for oral
2 for IV
Torsemide
80%
3.5
30% R and 70% M
7 for oral
7 for IV
Potassium-Sparing Diuretics
Amiloride
20%
8
R
24 for oral
Spironolactone
65%
1.5
M
60 for oral
Triamterene
50%
4
M
14 for oral
Osmotic Diuretics
Glycerol
95%
0.07
M
1 for oral
Mannitol
NA
1
R
7 for IV
Carbonic Anhydrase Inhibitors
Acetazolamide
70%
7.5
R
10 for oral
Dorzolamide
NA
Biphasic†
R and M
8 for topical ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diuretics
Only gold members can continue reading. Log In or Register to continue