In addition to the nephrons, the collecting ducts (the tubules into which the nephrons pour their contents) play a critical role in kidney function. The final segment of the distal convoluted tubule (4b) plus the collecting duct into which it empties (5) can be considered a single functional unit: the distal nephron.
Physiology
Overview of Kidney Functions
The kidney serves three basic functions: (1) cleansing of extracellular fluid (ECF) and maintenance of ECF volume and composition; (2) maintenance of acid-base balance; and (3) excretion of metabolic wastes and foreign substances (e.g., drugs, toxins). Of the three, maintenance of ECF volume and composition is the one that diuretics affect most.
The Three Basic Renal Processes
Effects of the kidney on ECF are the net result of three basic processes: (1) filtration, (2) reabsorption, and (3) active secretion. To cleanse the entire ECF, a huge volume of plasma must be filtered. Furthermore, to maintain homeostasis, practically everything that has been filtered must be reabsorbed—leaving behind only a small volume of urine for excretion.
Filtration
Filtration occurs at the glomerulus and is the first step in urine formation. Virtually all small molecules (electrolytes, amino acids, glucose, drugs, metabolic wastes) that are present in plasma undergo filtration. In contrast, cells and large molecules (lipids, proteins) remain behind in the blood. The most prevalent constituents of the filtrate are sodium ions and chloride ions. Bicarbonate ions and potassium ions are also present, but in smaller amounts.
The filtration capacity of the kidney is very large. Each minute the kidney produces 125 mL of filtrate, which adds up to 180 L/day. Because the total volume of ECF is only 12.5 L, the kidneys can process the equivalent of all the ECF in the body every 100 minutes. Hence, the ECF undergoes complete cleansing about 14 times each day.
Be aware that filtration is a nonselective process and therefore cannot regulate the composition of urine. Reabsorption and secretion—processes that display a significant degree of selectivity—are the primary determinants of what the urine ultimately contains. Of the two, reabsorption is by far the more important.
Reabsorption
More than 99% of the water, electrolytes, and nutrients that are filtered at the glomerulus undergo reabsorption. This conserves valuable constituents of the filtrate while allowing wastes to undergo excretion. Reabsorption of solutes (e.g., electrolytes, amino acids, glucose) takes place by way of active transport. Water then follows passively along the osmotic gradient created by solute reuptake. Specific sites along the nephron at which reabsorption takes place are discussed later. Diuretics work primarily by interfering with reabsorption.
Active Tubular Secretion
The kidney has two major kinds of “pumps” for active secretion. These pumps transport compounds from the plasma into the lumen of the nephron. One pump transports organic acids, and the other transports organic bases. Together, these pumps can promote the excretion of a wide assortment of molecules, including metabolic wastes, drugs, and toxins. The pumps for active secretion are located in the proximal convoluted tubule.
Processes of Reabsorption That Occur at Specific Sites Along the Nephron
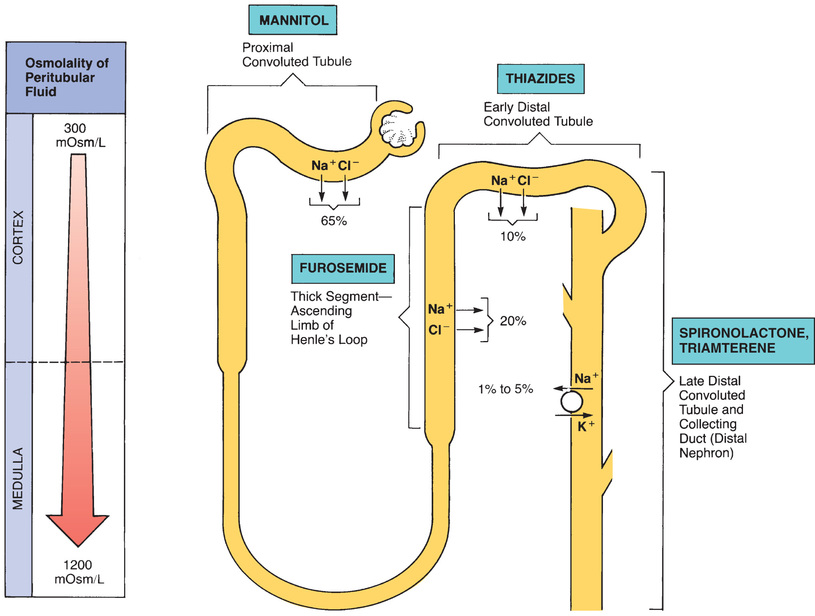
Because most diuretics act by disrupting solute reabsorption, to understand the diuretics, we must first understand the major processes by which nephrons reabsorb filtered solutes. Because sodium and chloride ions are the predominant solutes in the filtrate, reabsorption of these ions is of greatest interest. As we discuss reabsorption, numeric values are given for the percentage of solute reabsorbed at specific sites along the nephron. Bear in mind that these values are only approximate. Fig. 35.2 depicts the sites of sodium and chloride reabsorption, indicating the amount of reabsorption that occurs at each site.
Proximal Convoluted Tubule
The proximal convoluted tubule (PCT) has a high reabsorptive capacity. A large fraction (about 65%) of filtered sodium and chloride is reabsorbed at the PCT. In addition, essentially all of the bicarbonate and potassium in the filtrate is reabsorbed here. As sodium, chloride, and other solutes are actively reabsorbed, water follows passively. Because solutes and water are reabsorbed to an equal extent, the tubular urine remains isotonic (300 mOsm/L). By the time the filtrate leaves the PCT, sodium and chloride are the only solutes that remain in significant amounts.
Loop of Henle
The descending limb of the loop of Henle is freely permeable to water. Hence, as tubular urine moves down the loop and passes through the hypertonic environment of the renal medulla, water is drawn from the loop into the interstitial space. This process decreases the volume of the tubular urine and causes the urine to become concentrated (tonicity increases to about 1200 mOsm/L).
Within the thick segment of the ascending limb of the loop of Henle, about 20% of filtered sodium and chloride is reabsorbed (see Fig. 35.2). Because, unlike the descending limb, the ascending limb is not permeable to water, water must remain in the loop as reabsorption of sodium and chloride takes place. This process causes the tonicity of the tubular urine to return to that of the original filtrate (300 mOsm/L).
Distal Convoluted Tubule (Early Segment)
About 10% of filtered sodium and chloride is reabsorbed in the early segment of the distal convoluted tubule. Water follows passively.
Distal Nephron: Late Distal Convoluted Tubule and Collecting Duct
The distal nephron is the site of two important processes. The first involves exchange of sodium for potassium and is under the influence of aldosterone. The second determines the final concentration of the urine and is regulated by antidiuretic hormone (ADH). Although sodium-potassium exchange is discussed in more detail, we will not continue discussion of ADH because it has little to do with the actions of diuretics.
Sodium-Potassium Exchange
Aldosterone, the principal mineralocorticoid of the adrenal cortex, stimulates reabsorption of sodium from the distal nephron. At the same time, aldosterone causes potassium to be secreted. Although not directly coupled, these two processes—sodium retention and potassium excretion—can be viewed as an exchange mechanism. This exchange is shown in Fig. 35.2. Aldosterone promotes sodium-potassium exchange by stimulating cells of the distal nephron to synthesize more of the pumps responsible for sodium and potassium transport.
Introduction to Diuretics
How Diuretics Work
Most diuretics share the same basic mechanism of action: blockade of sodium and chloride reabsorption. By blocking the reabsorption of these prominent solutes, diuretics create osmotic pressure within the nephron that prevents the passive reabsorption of water. Hence diuretics cause water and solutes to be retained within the nephron and thereby promote the excretion of both.
The increase in urine flow that a diuretic produces is directly related to the amount of sodium and chloride reabsorption that it blocks. Accordingly, drugs that block solute reabsorption to the greatest degree produce the most profound diuresis. Because the amount of solute in the nephron becomes progressively smaller as filtrate flows from the proximal tubule to the collecting duct, drugs that act early in the nephron have the opportunity to block the greatest amount of solute reabsorption. As a result, these agents produce the greatest diuresis. Conversely, because most of the filtered solute has already been reabsorbed by the time the filtrate reaches the distal parts of the nephron, diuretics that act at distal sites have very little reabsorption available to block. Consequently, such agents produce relatively scant diuresis.
It is instructive to look at the quantitative relationship between blockade of solute reabsorption and production of diuresis. Recall that the kidneys produce 180 L of filtrate a day, practically all of which is normally reabsorbed. With filtrate production at this volume, a diuretic will increase daily urine output by 1.8 L for each 1% of solute reabsorption that is blocked. A 3% blockade of solute reabsorption will produce 5.4 L of urine a day—a rate of fluid loss that would reduce body weight by 12 pounds in 24 hours. Clearly, with only a small blockade of reabsorption, diuretics can produce a profound effect on the fluid and electrolyte composition of the body.
Adverse Impact on Extracellular Fluid
To promote excretion of water, diuretics must interfere with the normal operation of the kidney. By doing so, diuretics can cause hypovolemia (from excessive fluid loss), acid-base imbalance, and altered electrolyte levels. These adverse effects can be minimized by using short-acting diuretics and by timing drug administration such that the kidney is allowed to operate in a drug-free manner between periods of diuresis. Both measures will give the kidney periodic opportunities to readjust the ECF to compensate for any undesired alterations produced under the influence of diuretics.
Classification of Diuretics
There are four major categories of diuretic drugs: (1) loop diuretics (e.g., furosemide); (2) thiazide diuretics (e.g., hydrochlorothiazide); (3) osmotic diuretics (e.g., mannitol); and (4) potassium-sparing diuretics. The last group, the potassium-sparing agents, can be subdivided into aldosterone antagonists (e.g., spironolactone) and nonaldosterone antagonists (e.g., triamterene).
In addition to the four major categories of diuretics, there is a fifth group: the carbonic anhydrase inhibitors. Although the carbonic anhydrase inhibitors are classified as diuretics, these drugs are employed primarily to lower intraocular pressure (IOP) and not to increase urine production. Consequently, the carbonic anhydrase inhibitors are discussed in Chapter 84.
Loop Diuretics
The loop agents are the most effective diuretics available. These drugs produce more loss of fluid and electrolytes than any other diuretics. They are known as loop diuretics because their site of action is in the loop of Henle.
Furosemide
Furosemide [Lasix] is the most frequently prescribed loop diuretic and will serve as our prototype for the group.
Mechanism of Action
Furosemide acts in the thick segment of the ascending limb of the loop of Henle to block reabsorption of sodium and chloride (see Fig. 35.2). By blocking solute reabsorption, furosemide prevents passive reabsorption of water. Because a substantial amount (20%) of filtered NaCl is normally reabsorbed in the loop of Henle, interference with reabsorption here can produce profound diuresis.
Pharmacokinetics
With oral administration, diuresis begins in 60 minutes and persists for 8 hours. Oral therapy is used when rapid onset is not required. Furosemide undergoes hepatic metabolism followed by renal excretion.
Therapeutic Uses
Furosemide is a powerful drug that is generally reserved for situations that require rapid or massive mobilization of fluid. This drug should be avoided when less efficacious diuretics (thiazides) will suffice. Conditions that justify use of furosemide include (1) pulmonary edema associated with congestive heart failure (CHF); (2) edema of hepatic, cardiac, or renal origin that has been unresponsive to less efficacious diuretics; and (3) hypertension that cannot be controlled with other diuretics. Furosemide is especially useful in patients with severe renal impairment because, unlike the thiazides (see later), the drug can promote diuresis even when renal blood flow and glomerular filtration rate (GFR) are low. If treatment with furosemide alone is insufficient, a thiazide diuretic may be added to the regimen. There is no benefit to combining furosemide with another loop diuretic.
Adverse Effects
Hyponatremia, Hypochloremia, and Dehydration
Furosemide can produce excessive loss of sodium, chloride, and water. Severe dehydration can result. Signs of evolving dehydration include dry mouth, unusual thirst, and oliguria. Impending dehydration can also be anticipated from excessive loss of weight. If dehydration occurs, furosemide should be withheld.
The risk for dehydration and its sequelae can be minimized by initiating therapy with low doses, adjusting the dosage carefully, and monitoring weight loss every day.
Hypotension
Furosemide can cause a substantial drop in blood pressure. At least two mechanisms are involved: (1) loss of volume and (2) relaxation of venous smooth muscle, which reduces venous return to the heart. Signs of hypotension include dizziness, lightheadedness, and fainting. If blood pressure falls precipitously, furosemide should be discontinued. Because of the risk for hypotension, blood pressure should be monitored routinely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


