http://evolve.elsevier.com/McCuistion/pharmacology
Numerous skin lesions and eruptions require mild to aggressive drug therapy. Skin disorders include acne vulgaris, psoriasis, eczema dermatitis, contact dermatitis, drug-induced dermatitis, and burn infection. Skin eruptions may result from viruses, such as herpes simplex and zoster; fungi (e.g., tinea pedis [athlete’s foot], tinea capitis [ringworm]); and bacteria.
Skin lesions may appear as macules (flat and nonpalpable, usually less than 10 mm in diameter with varying colors), papules (raised and palpable, less than 10 mm in diameter), vesicles (clear, fluid-filled blisters smaller than 10 mm in diameter), or plaques (palpable lesions that are depressed or elevated when compared with the skin surface and greater than 10 mm in diameter). Treatments for skin eruptions include topical creams, ointments, pastes, gels, lotions, and solutions. Selected skin disorders and their drug therapy regimens are discussed separately. Treatment information can be found at the American Academy of Dermatology (AAD) website: https://www.aad.org.
Acne Vulgaris
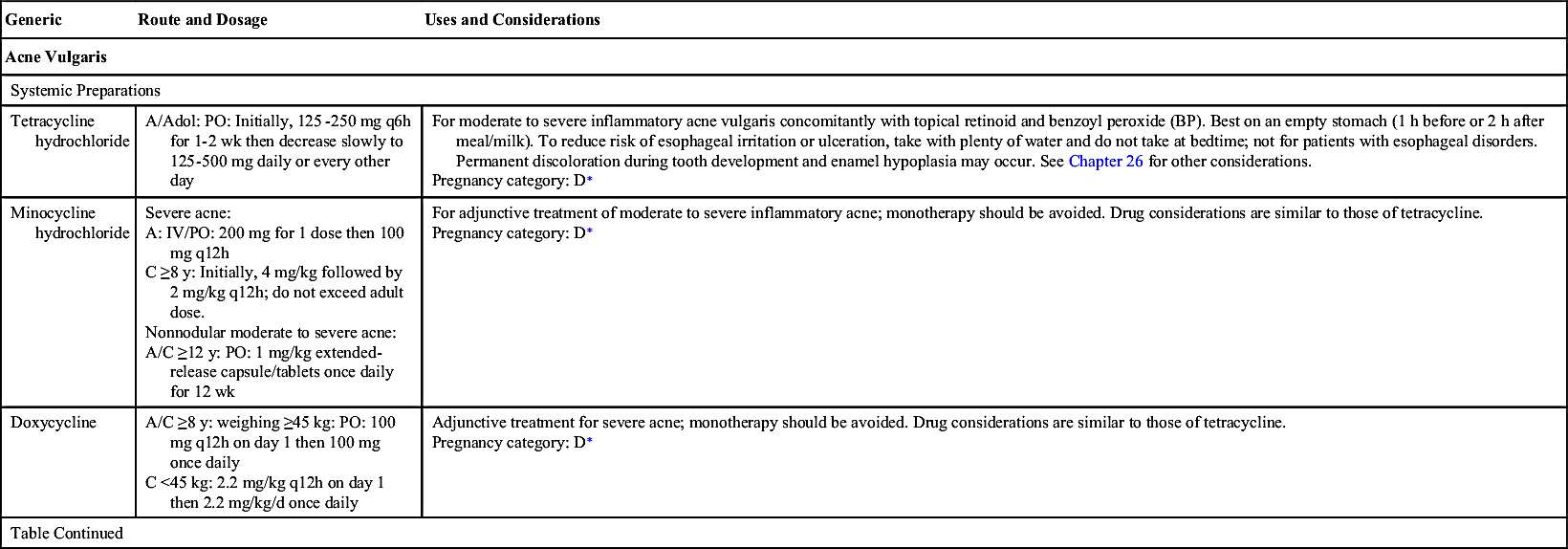
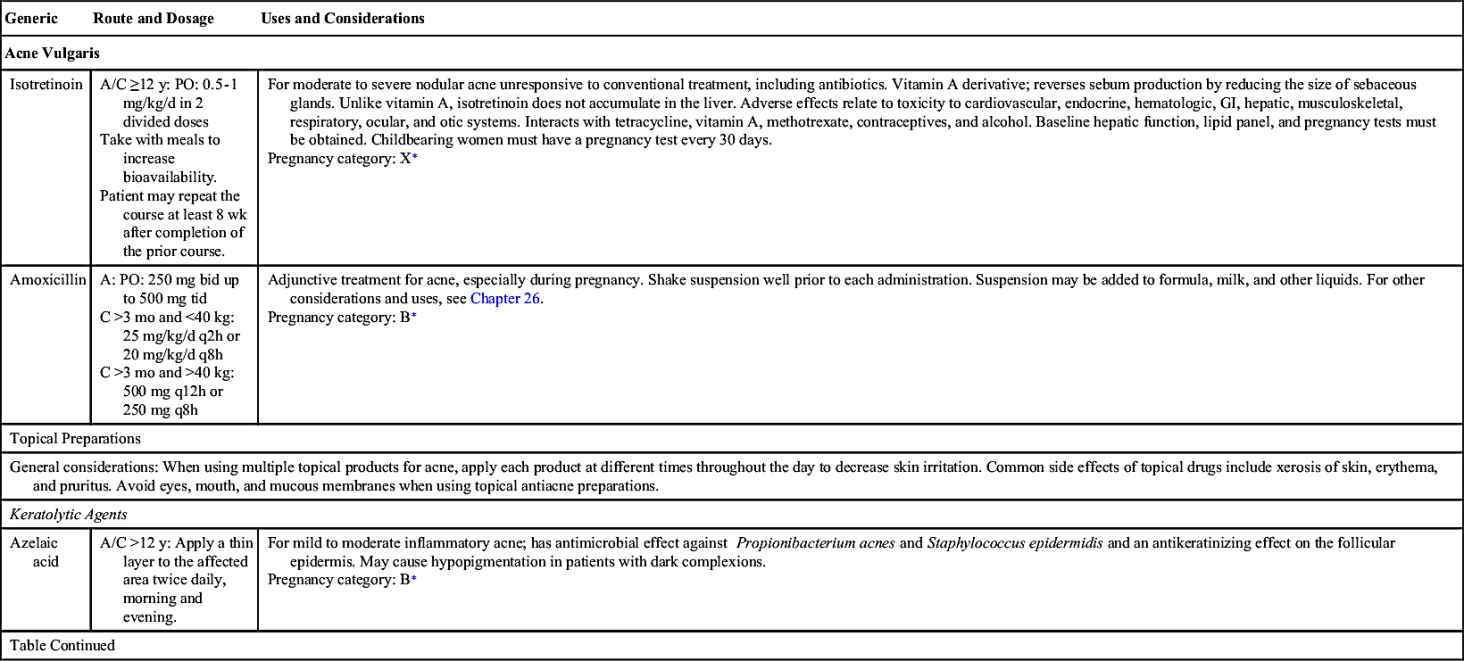
Acne is the most common skin disorder in the United States. Acne is more prevalent among adolescents, but adults and children can also develop acne. Acne vulgaris is the formation of papules, nodules, and cysts on the face, neck, shoulders, and back that results not from dirt but from keratin plugs at the base of the pilosebaceous oil glands near the hair follicles. The keratin plugs trap normal skin flora, including bacteria commonly found on the skin; the primary bacterium is Propionibacterium acnes. Bacteria start proliferating, which causes inflammation and irritation. During adolescence, production of androgens and sebum—an oily skin lubricant—are increased. The sebum combines with keratin, a protein that is part of the skin, to form a plug that results in acne. Comedones are types of noninflammatory acne lesions that may be open (blackheads) or closed (whiteheads). Open comedones are dilated hair follicle openings that allow oxidation of the debris within the follicle; closed comedones are small, plugged hair follicles. As with other forms of acne, comedones are not a result of poor hygiene. All forms of acne should be treated to prevent lifelong scars. Acne can be treated nonpharmacologically and pharmacologically. Table 45.1 lists the drugs commonly used to control acne vulgaris along with their dosages, uses, and considerations.
Nonpharmacologic Approach
Nonpharmacologic measures should be tried before drug therapy is initiated. A prescribed or suggested cleansing agent, such as antibacterial soap, is necessary for all types of acne. The skin should be gently cleansed twice daily, but vigorous scrubbing should be avoided. Overscrubbing and overwashing can irritate the skin, worsening the acne and possibly causing an infection. The American Osteopathic College of Dermatology recommends not using abrasive cleaners. In addition to facial hygiene, shampooing hair to decrease the oiliness may help with acne. Keeping hair away from the face has also been shown to decrease acne. Cosmetics should be water based because oil-based products can increase the clogging of skin pores. A well-balanced diet that is low in fat and sugar is recommended, and excessive carbohydrates should be avoided. Decreasing emotional stress and increasing emotional support are also suggested. If drug therapy is necessary, nonpharmacologic measures should be maintained as well.
Pharmacologic Treatment
Acne is not curable, but it is manageable. Acne medications may help decrease scar formation related to acne. The best course for patients with acne is to see a dermatologist who can prescribe treatment specific to the individual, therefore the course of therapy will vary according to the severity and extent of the acne.
Topical Antiacne Drugs
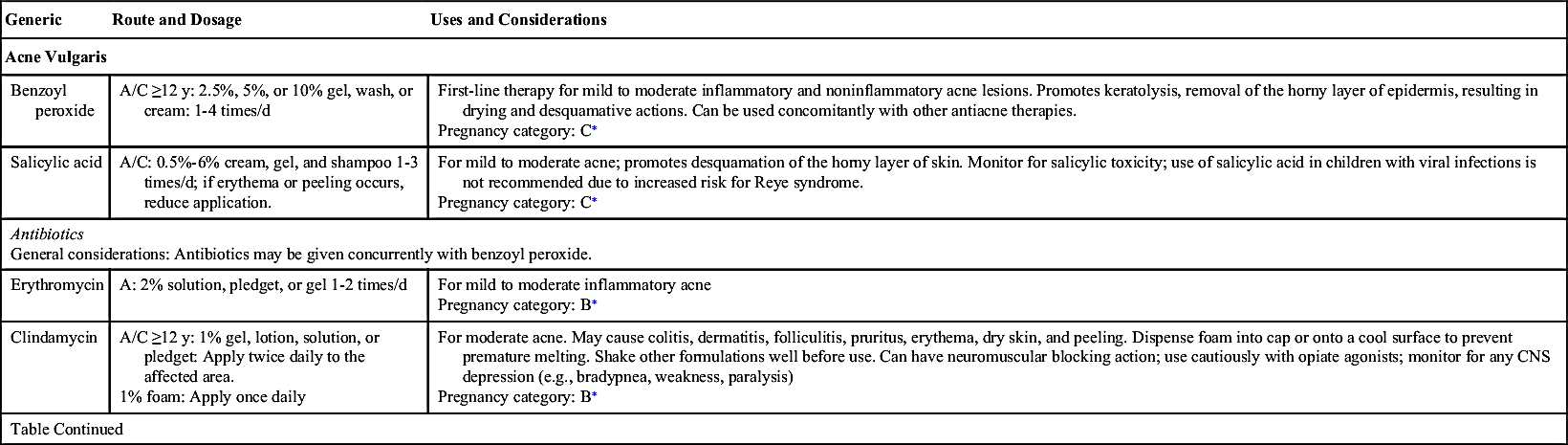
Mild acne is generally treated with topical drugs that treat existing acne and prevent new eruptions. Commonly used topical therapies for mild acne include benzoyl peroxide, retinoids, salicylic acid, antibiotics, or combinations of these in addition to gentle cleansing.
Benzoyl peroxide (BP) is an antibacterial agent that kills P. acnes, the predominant organism in sebaceous follicles and comedones. BP releases free radical oxygen species that oxidize bacterial proteins. When included as an adjunct to an antibiotic regimen, control of acne is enhanced. Resolution of acne usually occurs within 4 to 6 weeks. BP is applied as a cream, lotion, or gel once or twice a day and can be left on or washed off. Washing BP off may be better tolerated in patients with sensitive skin.
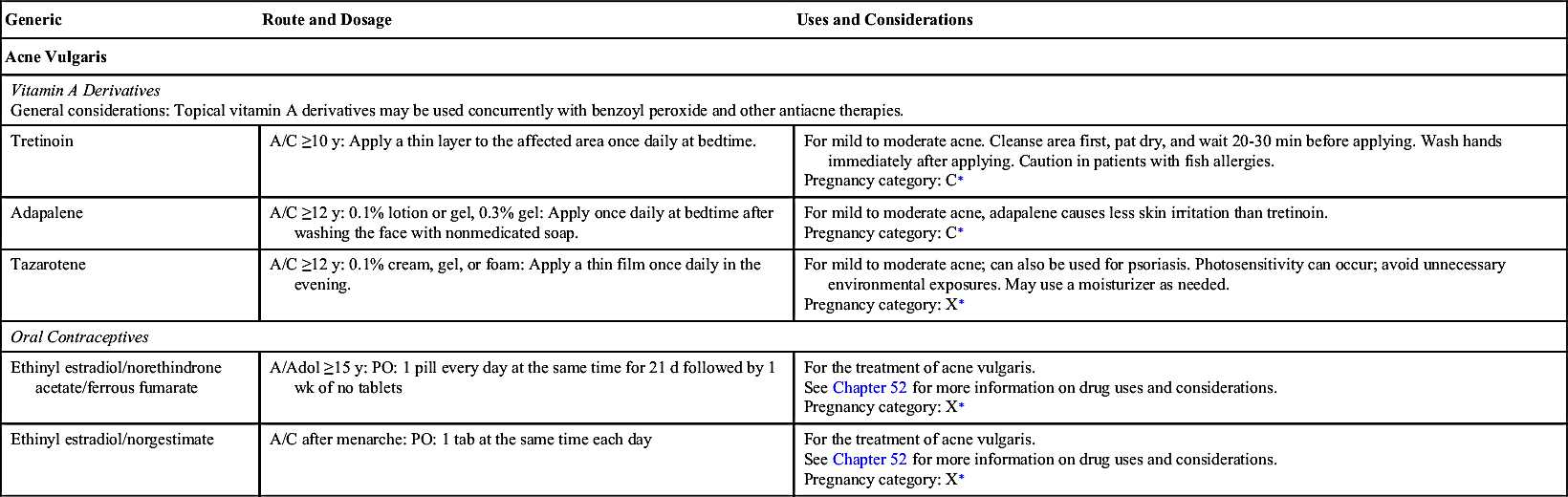
Topical retinoids such as tretinoin, adapalene, and tazarotene are derivatives of vitamin A and are used for mild to moderate acne that alters keratinization. They are the mainstay of topical therapy because of their comedolytic activities, and they also have antiinflammatory actions. Retinoids alter the intracrine and paracrine mediators of cell differentiation and proliferation, apoptosis, and reproduction, thereby modifying gene expression, subsequent protein synthesis, and epithelial cell growth. Retinoids prevent horny cell cohesion, or keratolysis, and increase epithelial cell turnover. They do not affect microorganisms in acne and sebum production. Topical retinoids are appropriate for all types of acne when used in combination with other antiacne therapy. They also allow maintenance of acne clearance after discontinuing oral antibiotics. Of the retinoids, tazarotene is contraindicated with pregnancy. Retinoids should not be used before or after extended sun exposure or sunburn because they can increase the risk of sunburn and intensify existing sunburn.
Another antiacne topical agent, azelaic acid, has antibacterial, antiinflammatory, and mild comedolytic actions. Azelaic acid is as effective as BP and tretinoin combined. Salicylic acid is also a comedolytic treatment that is available over the counter in various strengths. However, the efficacy of salicylic acid is still unknown. Topical treatments with retinoids, azelaic acid, and salicylic acid can cause burning, pruritus, and erythema after several applications; however, they are less common with azelaic acid.
Moderate to severe acne may require a stronger concentration of BP, and topical antibiotics, such as tetracycline, erythromycin, and clindamycin, may be added to the treatment regimen. Erythromycin and clindamycin are the recommended topical antibiotics for acne therapy; however, erythromycin has reduced efficacy when compared with clindamycin. Topical antibiotics accumulate in the hair follicle and have both antiinflammatory and antibacterial effects. Topical antibiotics as monotherapy are not recommended due to the development of antibiotic resistance. Severe painful acne may be treated with steroid injection.
Systemic Antiacne Drugs
For severe acne, adjunctive treatment is usually warranted with oral antibiotics (e.g., doxycycline and minocycline [drugs of choice], tetracycline, amoxicillin) in addition to topical corticosteroids (Box 45.1).  Tetracycline antibiotics, however, should not be used among the very young and among pregnant patients; drugs of the tetracycline class may cause dental discoloration to the developing teeth and have teratogenic effects on the fetus. Instead, amoxicillin or another non-tetracycline drug may be given for severe acne. See Chapter 26 for more information on antibacterials.
Tetracycline antibiotics, however, should not be used among the very young and among pregnant patients; drugs of the tetracycline class may cause dental discoloration to the developing teeth and have teratogenic effects on the fetus. Instead, amoxicillin or another non-tetracycline drug may be given for severe acne. See Chapter 26 for more information on antibacterials.
 Tetracycline antibiotics, however, should not be used among the very young and among pregnant patients; drugs of the tetracycline class may cause dental discoloration to the developing teeth and have teratogenic effects on the fetus. Instead, amoxicillin or another non-tetracycline drug may be given for severe acne. See Chapter 26 for more information on antibacterials.
Tetracycline antibiotics, however, should not be used among the very young and among pregnant patients; drugs of the tetracycline class may cause dental discoloration to the developing teeth and have teratogenic effects on the fetus. Instead, amoxicillin or another non-tetracycline drug may be given for severe acne. See Chapter 26 for more information on antibacterials.Isotretinoin, a derivative of vitamin A taken orally, is used for treatment of severe cystic acne that is not responsive to conventional therapy. It decreases sebum formation and secretion and has antiinflammatory and antikeratinizing (keratolytic) effects, decreasing lesions and scars due to acne. Additional benefits of isotretinoin include a decrease in anxiety and depression. The typical patient takes this drug for 4 to 6 months. Adverse reactions may occur that are dose dependent; these include chelitis, dizziness, cephalgia, conjunctivitis, skin irritation, pruritus, epistaxis, myalgia, arthralgia, temporary hair thinning, photosensitivity, depression, and suicidal thoughts. Usually, one course of treatment with isotretinoin is curative of severe acne. Because isotretinoin is a derivative of vitamin A, patients should not take vitamin A concomitantly. Using vitamin A or tetracycline with isotretinoin may increase its adverse effects. Baseline blood tests—liver function tests (LFTs), serum lipid panel, and pregnancy tests among female patients of childbearing age—are required before initiating isotretinoin therapy and at intervals throughout therapy.  Isotretinoin must not be used during pregnancy; it is a known teratogen. Additional cautions associated with isotretinoin are to not breastfeed or to give blood during or for 1 month after therapy; patients should not take other medications or herbal products without first consulting their health care provider, drive at night without knowing the effect of isotretinoin on night vision, or have cosmetic procedures to smooth skin. Patient should be instructed to avoid excessively vigorous activity and to contact the health care provider and stop taking isotretinoin if they experience muscle weakness, which may be an indication of serious muscle damage.
Isotretinoin must not be used during pregnancy; it is a known teratogen. Additional cautions associated with isotretinoin are to not breastfeed or to give blood during or for 1 month after therapy; patients should not take other medications or herbal products without first consulting their health care provider, drive at night without knowing the effect of isotretinoin on night vision, or have cosmetic procedures to smooth skin. Patient should be instructed to avoid excessively vigorous activity and to contact the health care provider and stop taking isotretinoin if they experience muscle weakness, which may be an indication of serious muscle damage.
 Isotretinoin must not be used during pregnancy; it is a known teratogen. Additional cautions associated with isotretinoin are to not breastfeed or to give blood during or for 1 month after therapy; patients should not take other medications or herbal products without first consulting their health care provider, drive at night without knowing the effect of isotretinoin on night vision, or have cosmetic procedures to smooth skin. Patient should be instructed to avoid excessively vigorous activity and to contact the health care provider and stop taking isotretinoin if they experience muscle weakness, which may be an indication of serious muscle damage.
Isotretinoin must not be used during pregnancy; it is a known teratogen. Additional cautions associated with isotretinoin are to not breastfeed or to give blood during or for 1 month after therapy; patients should not take other medications or herbal products without first consulting their health care provider, drive at night without knowing the effect of isotretinoin on night vision, or have cosmetic procedures to smooth skin. Patient should be instructed to avoid excessively vigorous activity and to contact the health care provider and stop taking isotretinoin if they experience muscle weakness, which may be an indication of serious muscle damage. Because of isotretinoin’s powerful teratogenicity, a risk-management system to prevent isotretinoin-related teratogenicity was implemented. iPLEDGE is the third risk-management program to prevent exposure to isotretinoin during pregnancy. Prior to starting isotretinoin therapy, both males and females must enroll in the iPLEDGE risk-management program and adhere to it. The program was created to ensure patients who receive isotretinoin use two forms of contraception, that no patient is pregnant when treatment is initiated, and that no patient becomes pregnant while taking the drug or for at least 1 month after completing a course of isotretinoin. This comprehensive program also has rules for the health care provider, patient, pharmacist, and wholesaler. Further information can be found at https://www.ipledgeprogram.com.
Because of isotretinoin’s powerful teratogenicity, a risk-management system to prevent isotretinoin-related teratogenicity was implemented. iPLEDGE is the third risk-management program to prevent exposure to isotretinoin during pregnancy. Prior to starting isotretinoin therapy, both males and females must enroll in the iPLEDGE risk-management program and adhere to it. The program was created to ensure patients who receive isotretinoin use two forms of contraception, that no patient is pregnant when treatment is initiated, and that no patient becomes pregnant while taking the drug or for at least 1 month after completing a course of isotretinoin. This comprehensive program also has rules for the health care provider, patient, pharmacist, and wholesaler. Further information can be found at https://www.ipledgeprogram.com.Psoriasis
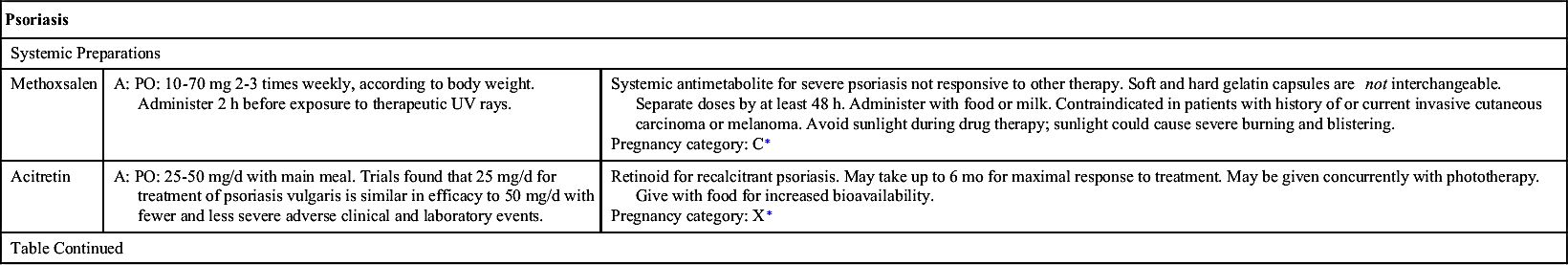
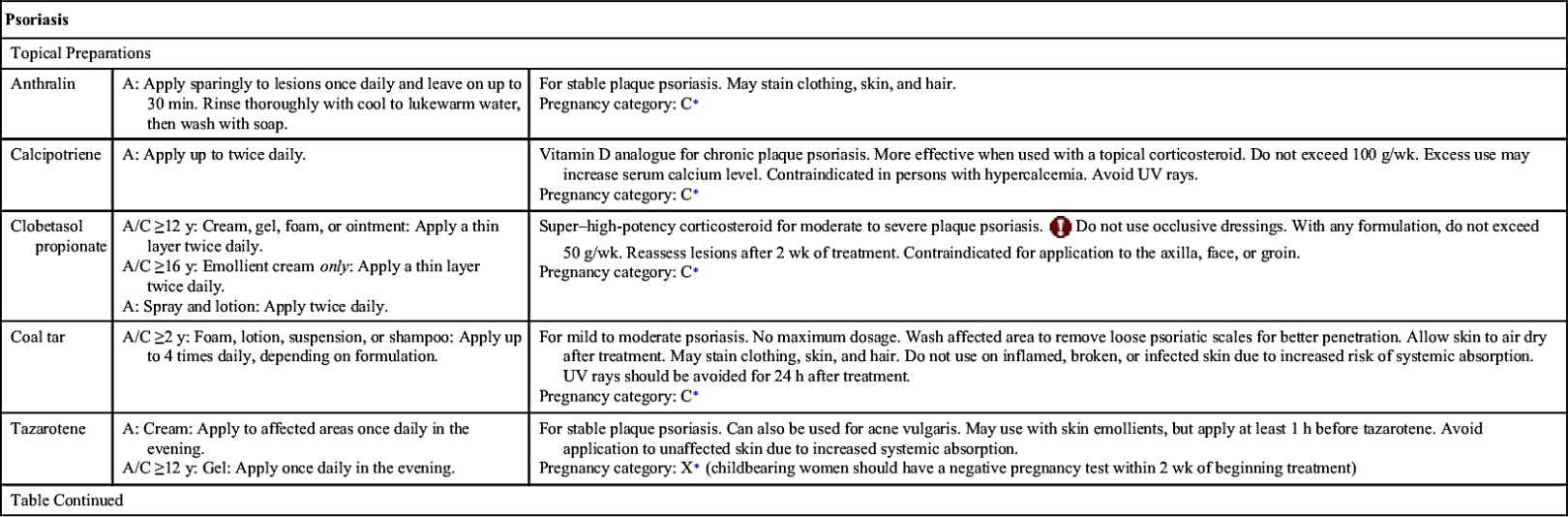
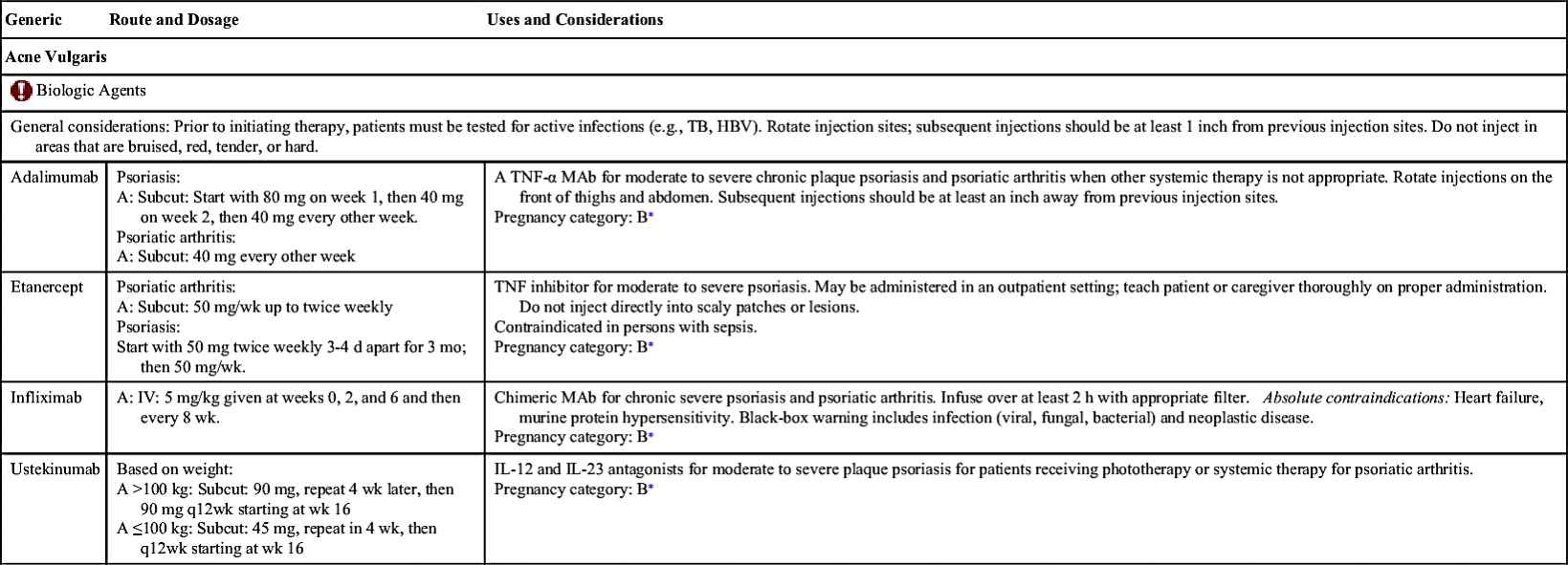
Psoriasis is a multisystem disease with predominant skin and joint disorders. According to the AAD, it affects nearly 2% of the population; of those affected, 80% have mild to moderate disease. A majority of the manifestations are exhibited as chronic skin inflammation that is characterized by scaly, erythematous plaques or scales. These plaques may be painful and are often pruritic, at times causing significant quality-of-life issues. They can appear on the scalp, elbows, palms, knees, and soles of the feet. Psoriasis is a chronic disease, and the manifestations wax and wane. Of the different forms of psoriasis, plaque psoriasis is the most common form. Depending on the severity of the disease, recommendations for the treatment of psoriasis include topical and systemic treatments and/or phototherapy. Table 45.1 lists some drugs, dosages, uses, and considerations for psoriasis. Table 45.2 lists current treatment modalities for psoriasis and psoriatic arthritis.
Topical Drugs
Vehicles for topical preparations are many and may include ointments, creams, lotions, solutions, gels, foams, and tape, among others. More than one topical medication may be used concomitantly to increase the effectiveness of each drug. If more than one topical drug is used, patients need to be instructed to apply each drug at separate times throughout the day. Topical drugs for psoriasis include corticosteroids, vitamin D analogues, tazarotene, calcineurin inhibitors (e.g., tacrolimus and pimecrolimus), salicylic acid, anthralin, and coal tar.
Topical corticosteroids are the principal treatment for the majority of patients. Corticosteroids are available in variety of vehicles that are sold over the counter (OTC) or by prescription; differing levels of potency are also available such that the weakest formula (e.g., 1% hydrocortisone) is available OTC, and the strongest (e.g., clobetasol propionate) is by prescription (see Box 45.1). Corticosteroids are classified according to their potency, class 1 to class 7, in which class 1 is the strongest (superpotent). The lower-potency topical steroids are reserved for sensitive skin (e.g., face, intertriginous areas, thin skin areas, in infants and older adults). Patients with thick skin and those with scales or plaques often require the highest-potency steroids.  The usual length of treatment for most topical steroids is 4 weeks; otherwise, adverse effects that include cutaneous side effects and systemic absorption may occur. Tapering topical steroids after clinical response is recommended by the AAD. Cutaneous side effects include skin atrophy, telangiectasia, striae distensae, acne, folliculitis, and purpura. Other effects include worsening of existing or preexisting skin conditions (dermatoses) and fungal infections (tineas). Worsening of psoriasis can also occur (rebound effect) with the use of topical corticosteroids. Even though systemic side effects are fewer than cutaneous side effects with topical steroids, these can still occur. Systemic effects usually occur with the highest-potency preparation used over a large surface for a prolonged period. Examples of systemic side effects include Cushing syndrome, cataracts, glaucoma, and suppression of the hypothalamic-pituitary-adrenal (HPA) axis, which can cause growth retardation.
The usual length of treatment for most topical steroids is 4 weeks; otherwise, adverse effects that include cutaneous side effects and systemic absorption may occur. Tapering topical steroids after clinical response is recommended by the AAD. Cutaneous side effects include skin atrophy, telangiectasia, striae distensae, acne, folliculitis, and purpura. Other effects include worsening of existing or preexisting skin conditions (dermatoses) and fungal infections (tineas). Worsening of psoriasis can also occur (rebound effect) with the use of topical corticosteroids. Even though systemic side effects are fewer than cutaneous side effects with topical steroids, these can still occur. Systemic effects usually occur with the highest-potency preparation used over a large surface for a prolonged period. Examples of systemic side effects include Cushing syndrome, cataracts, glaucoma, and suppression of the hypothalamic-pituitary-adrenal (HPA) axis, which can cause growth retardation.
 The usual length of treatment for most topical steroids is 4 weeks; otherwise, adverse effects that include cutaneous side effects and systemic absorption may occur. Tapering topical steroids after clinical response is recommended by the AAD. Cutaneous side effects include skin atrophy, telangiectasia, striae distensae, acne, folliculitis, and purpura. Other effects include worsening of existing or preexisting skin conditions (dermatoses) and fungal infections (tineas). Worsening of psoriasis can also occur (rebound effect) with the use of topical corticosteroids. Even though systemic side effects are fewer than cutaneous side effects with topical steroids, these can still occur. Systemic effects usually occur with the highest-potency preparation used over a large surface for a prolonged period. Examples of systemic side effects include Cushing syndrome, cataracts, glaucoma, and suppression of the hypothalamic-pituitary-adrenal (HPA) axis, which can cause growth retardation.
The usual length of treatment for most topical steroids is 4 weeks; otherwise, adverse effects that include cutaneous side effects and systemic absorption may occur. Tapering topical steroids after clinical response is recommended by the AAD. Cutaneous side effects include skin atrophy, telangiectasia, striae distensae, acne, folliculitis, and purpura. Other effects include worsening of existing or preexisting skin conditions (dermatoses) and fungal infections (tineas). Worsening of psoriasis can also occur (rebound effect) with the use of topical corticosteroids. Even though systemic side effects are fewer than cutaneous side effects with topical steroids, these can still occur. Systemic effects usually occur with the highest-potency preparation used over a large surface for a prolonged period. Examples of systemic side effects include Cushing syndrome, cataracts, glaucoma, and suppression of the hypothalamic-pituitary-adrenal (HPA) axis, which can cause growth retardation.Synthetic vitamin D analogues (e.g., calcipotriene) bind to vitamin D receptors, enhancing the differentiation of keratinocytes while inhibiting their proliferation. Calcipotriene is available in solution, foam, and cream and is usually combined with topical corticosteroids to increase clinical response. Local side effects include burning, pruritus, edema, peeling, dryness, and erythema. Systemic side effects usually occur due to overapplication and include hypercalcemia and suppression of parathyroid hormone. Patients need to be instructed to avoid ultraviolet (UV) light because UVA inactivates calcipotriene.
Topical tazarotene, a retinoid, normalizes abnormal keratinocyte differentiation and decreases hyperproliferation and inflammation. Tazarotene may be used concurrently with moisturizers and topical corticosteroids. Common side effects include local irritation, although tazarotene is a teratogen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree