Fig. 12.1
Silver alloy tarnishing (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
Mastication applies periodic stress to dental devices and causes friction between devices. As maximum biting force in the molar region is generally known to be equivalent to the static load of one’s body weight, dental devices may be damaged by stress corrosion and/or fretting corrosion (Fig. 12.2).
Fig. 12.2
Fretting corrosion (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
Therefore, when dental alloys are worn intraorally for long periods of time as dental devices, multiple factors that deteriorate corrosion resistance accumulate in addition to the formation of a corrosive intraoral environment. Thus, when considering the corrosion resistance of dental metallic materials to be used intraorally, it is important to consider the corrosion resistance of dental devices as a whole rather than the corrosion resistance properties of each individual material.
12.3 Treatment Methods [1]
12.3.1 Crown Restorations
When the shape or function of a tooth crown (part of the tooth exposed within the oral cavity) is partially lost due to dental caries (tooth decay) or external trauma, restoration with artificial materials is conducted.
When the range of damage is restricted to a relatively small area such as the molar occlusal surface (surface on which the back teeth clench) or the adjacent surface to the anterior teeth, restoration is performed by filling the cavity (missing portion left over after the lesion has been removed and the area has been appropriately shaped) with plastic materials that are hardened after they have been shaped. Although gold foil has been used as a filling material, the most common type of metallic plastic filling material is dental amalgam. Restorations using dental amalgam involve filling the cavity with plastic wet amalgam that is a mixture of mercury and amalgam alloy powder containing the main components of silver, tin, and copper. After the amalgam hardens, the filling is polished. Because amalgam filling restorations offer excellent treatment outcomes and operability, they have long been widely clinically applied. However, there are concerns that amalgam is harmful to the human body, and it also has the disadvantages of tarnishing and tooth fractures. Thus, the development of composite resin (composite materials containing ceramic particles as a filler in a high polymer matrix), which adheres to the tooth and offers excellent esthetic properties, has meant that composite resin is now becoming more widely used.
Crown restorations performed by luting dental cement onto a metal casting manufactured outside of the oral cavity are called cast restorations. Inlays (Fig. 12.3) refer to restorations that are shaped to the tooth and fitted to the inside (surrounded by dentin) of the cavity, and crowns (Fig. 12.4) refer to restorations used to cover the cusp when the cavity area is relatively large. Abutment construction to compensate for the area of missing tooth is also frequently used to make crown restorations possible. When the missing area is relatively small, plastic filling materials are used, but when the missing area extends to the root canal, prefabricated posts or a metal core comprising a metal casting is used.



Fig. 12.3
Inlay (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)

Fig. 12.4
Crown (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
Cast restorations involve first removing the caries and then filing down (shaping) and filling in (cavity base, construction) the remaining tooth to make it into a suitable shape for the restoration. Next, dies (impressions) of the row of teeth that will hold the restoration and opposing teeth are taken, and the occlusal relationship is registered (interocclusal registration). The impressions and interocclusal registration results are then used to create a plaster cast, upon which a wax pattern is fabricated. This wax pattern is embedded in heat-resistant investment materials and fired to create a mold. Molten aluminum alloy is then cast in the mold. Dental casting is a type of lost wax process that has been industrialized for precision casting. Finally, the casting is adjusted on the die and in the patient’s mouth, before being polished and luted with dental cement. When luting crown restorations onto teeth, dental castings must be extremely precise, and cement layer thickness is ordered per 10 μm. If the cement is too thick, the structure may start to collapse from the exposed cement layer, and the entry of bacteria from food, drink, and saliva may lead to secondary caries, which can cause the casting to fall out. Quartz and silica (SiO2) cristobalite are used as base investing materials to achieve high casting precision. The setting expansion and thermal expansion of the die materials compensate for alloy casting shrinkage.
Rather than being completely made of metal, crowns are often partially made from hard resin or porcelain the same color as the tooth crown (facing crowns) to enhance esthetics. Strength of adhesive bonding is an important factor for both of the above types of facing crowns, which have complex structures. For the former type, hard resin facing crowns (Fig. 12.5), adhesive primers (pretreatment agents), have been developed for each type of alloy. The latter, porcelain fused to metal (PFM) crowns, is formed by fusing porcelain onto the alloy surface, as the name suggests. Elements are added to the alloy so that it forms an oxide film that increases the strength of porcelain fusion to metal while also increasing the melting point. Firing temperature is lowered on the porcelain side as well so that the alloy does not change shape and the thermal expansion coefficient of the porcelain is set slightly higher than that of the alloy so that contraction due to cooling after firing does not cause cracks on the interface. Recently, porcelain inlays and crowns (all-ceramic crowns) that use no metal at all are also becoming more commonly used.


Fig. 12.5
Hard resin facing crown (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
12.3.2 Prosthodontic Treatments for Missing Teeth
When teeth are lost due to periodontal disease, caries, or external trauma, prosthodontic treatments using artificial materials to recover form and function are performed.
When one or multiple teeth are missing, two or more teeth are joined as abutment teeth (teeth used to support and maintain dentures), and a bridge (Fig. 12.6) is constructed to recover the lost shape and function of missing teeth. When the bridge is relatively small, a one-piece cast may be used. However, when multiple teeth are missing, parts of the bridge may be cast separately before being joined with a soldering alloy or welded with a laser. The area of the missing tooth is covered with an artificial tooth called a pontic, which is shaped taking hygiene, functionality, and esthetics into consideration, depending on its location. Hard resin facing crowns and PFM crowns are used for anterior teeth because esthetic properties are important elements in this area. Furthermore, because the use of adhesive resin increases the bonding strength of luting cement, bridges that require little filing down of the remaining tooth are now a possibility.


Fig. 12.6
Bridge (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
Another treatment option is dentures, which morphologically compensate for the missing tooth and accompanying retraction of surrounding tissue and aim for functional and esthetic recovery. Types of dentures include removable dentures, partial dentures (Fig. 12.7) for use with remaining teeth, and full dentures. Partial denture design is diverse, taking into account the number and position of remaining teeth and type of retainer. Metal base dentures contain metal in the frame of the base, which constitutes the body of plate dentures, with the aim of increasing strength and sense of fit. In general, metal base dentures are fabricated via precision casting. Types of retainers used to prevent dentures from falling out include clasps that comprise wires wrapping around the abutment teeth and attachments that exhibit retentive force by joining parts attached to the abutment teeth to parts in the denture. Wire clasps made by bending alloy wires or cast clasps fabricated by casting may be used. Recently, magnetic attachments that utilize the suction force of magnets for retentive force have been developed. Magnets used include samarium-cobalt alloy and neodymium-iron-boron alloy. Ferrite magnetic stainless steel (SUS444, SUSXM27, SUS47J1), which has excellent corrosion resistance, is used for the keeper (side pulled by magnetic force within the dentures) and yoke (magnet cover).
Fig. 12.7
Partial denture (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
12.3.3 Dental Implants
Dental implants are artificial objects embedded into intraoral tissue to compensate for missing teeth. Implants are classified according to the site of insertion into intramucosal, sub-membrane, endodontic, and endosseous implants. Currently, endosseous implants (Fig. 12.8) inserted into the jawbone are the most common and are widely applied clinically. Materials implanted in the root portion in alveolar bone (fixtures) are mainly made of titanium, which has excellent biocompatibility. Good clinical outcomes are achieved with fixtures, as they offer osseointegration with no soft tissue separating them from bony tissue. Furthermore, some have a shape that promotes invasion of bony tissue or are coated with bioceramics such as hydroxyapatite, which offers osseoinduction and osseoconduction. In dental implant treatments, a fixture implanted within the bone is used as the foundation, and the abutment is placed. Then, the “superstructure” comprising a crown, bridge, or prosthesis with base is fixated.
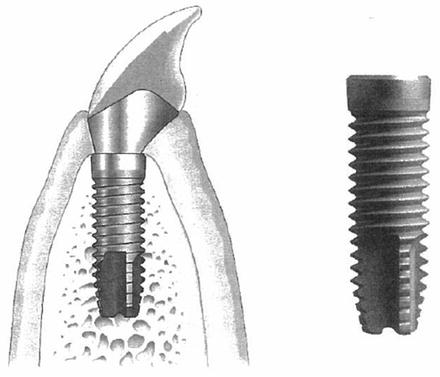
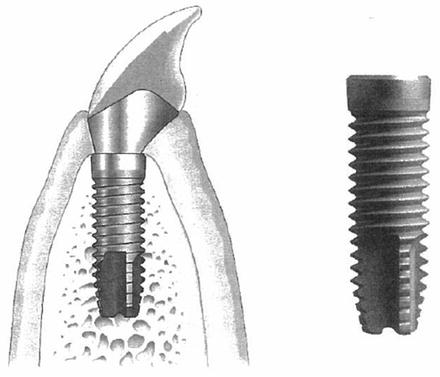
Fig. 12.8
Dental implant (Reprinted from Ref. [1], Copyright 2010, with permission from the Japan Institute of Metals)
12.3.4 Orthodontic Treatments
Orthodontic treatments use mainly metal wire elasticity or superelasticity as orthodontic force to move teeth into target positions. Orthodontic wires may be made of materials such as stainless steel, cobalt-chromium (Co-Cr) alloy, titanium-nickel (Ti-Ni) alloy, or titanium-molybdenum alloy. Ti-Ni alloy wires that apply superelasticity in particular are widely used clinically due to their persistent exertion of orthodontic force appropriate for moving teeth. Arch fixtures suited to the tooth dentition may be twisted into circular, square cross-sectional shapes or bundle shapes and are fixated in brackets fitted to the labial buccal surfaces of teeth. Various other types of devices are also used in orthodontic treatments to move individual teeth and rows of teeth. These include, for example, expansion appliances for widening narrowed maxillary dentition with screws and thick wires, arch appliances composed of a main wire fixated to the dentition and springs and hooks soldered to this, and orthodontic plates combining labial side guide wires, clasps, and springs with a resin base. Retainers used to prevent recurrence after teeth have been moved to the correct position also come in various shapes. In general, all types of orthodontic devices use Co-Cr alloy or stainless steel wires that have been bent.
12.3.5 Other Treatments
As the extent of dental caries progresses and bacteria reach the dental pulp (soft tissue containing nerves and blood vessels) inside the tooth, the infected pulp must be removed, and the walls of the root canal that held the pulp must be mechanically and chemically expanded and cleaned to make it possible to conserve the tooth. In this type of endodontic procedure, a stainless steel dental reamer and file are usually used manually for mechanical root canal enlargement. In recent years, motorized root canal preparation using a superelastic Ti-Ni alloy file required for good results even in the case of bent root canals is being clinically applied and is garnering attention.
Because jaw fracture and orthognathic surgery involve fixation of bone fragments, the same osteosynthesis plates used for orthopedic surgery are employed. The plates used in oral surgery, however, are often smaller “mini-plates.” Previously, stainless steel plates had been used, but titanium plates have now become mainstream. The plate is bent to follow the bone surface and fixated to the bone fragment with screws. For reconstructive maxillofacial surgery, dental implants and different types of reconstructive plates are used.
12.4 Types and Features of Dental Metallic Materials
12.4.1 Dental Casting Alloys
Dental casting alloys are commonly used in dental treatments such as crown restorations and prosthodontic treatments for missing teeth. These alloys must have sufficient mechanical properties (strength, ductility, etc.) that suit the purpose of their use, offer excellent corrosion resistance, cause no toxicity or irritation, and have superior casting performance. Previously, there were separate standards for each type of alloy, but in 2006, internationally unified standards, “ISO22674: Dentistry―Metallic materials for fixed and removable restorations and appliances” [2], were determined by the International Organization for Standardization (ISO). These standards divide dental metallic materials into six types depending on their mechanical properties and specify the uses for each type (Table 12.1).
Table 12.1
Mechanical properties and uses of dental restorations and metallic materials for prostheses by type
Type | 0.2 % proof stress (MPa) minimum | Elongation (%) minimum | Elastic modulus (GPa) minimum | Uses |
|---|---|---|---|---|
0 | – | – | – | Fixed restorations with low stress loading (e.g., small, one-sided veneer inlays and veneer crowns, metal frames for porcelain bonding made via electroforming or sintering) |
1 | 80 | 18 | – | Fixed restorations with low stress loading (e.g., one-sided inlays, veneer crowns) |
2 | 180 | 10 | – | Fixed restorations (e.g., inlays, crowns) |
3 | 270 | 5 | – | Fixed restorations and prostheses for multiple teeth (e.g., bridges) |
4 | 360 | 2 | – | Devices with high stress loading (e.g., removable partial dentures, clasps, thin crowns, long span bridges, bridges with small section surfaces, burrs, attachments, implant superstructures) |
5 | 500 | 2 | 150 | Devices that require high rigidity and strength (e.g., thin removable partial dentures, parts with thin section surfaces, clasps) |
12.4.1.1 Dental Casting Gold Alloys
Dental casting gold alloys must offer mechanical properties suitable for their use and superior casting performance while still maintaining the excellent corrosion resistance and chemical stability of gold. The additional elements mainly used to create gold alloys are selected for their ability to improve mechanical properties and lower the melting point. Table 12.2 shows typical elements and their effects [1]. Silver and copper are the main elements that constitute the elemental composition of gold alloys. The hardness and strength are improved by making the copper into a proportional solid solution with gold. When more than approximately 10mass% of copper is added, it undergoes solid phase transformation to Au3Cu or AuCu superlattice below 680 K; thus, improved mechanical properties due to age hardening can also be anticipated. Copper is also greatly involved in lowering melting point, but when it is added in large amounts, it leads to reddening and decreased corrosion resistance of the alloy. Silver becomes a proportional solid solution with gold but can form an alloy without changing any mechanical properties. Decreasing the amount of gold contained in the alloy and adding copper can prevent reddening. Platinum and palladium are harder than gold and have a higher elastic modulus. They increase the elastic modulus and strength of gold alloys. Therefore, they are added to gold alloys used in large prosthodontic appliances. Like silver, platinum and palladium prevent the reddening effects of adding copper, but, because they markedly increase the melting point, they cannot be added in large amounts to dental casting gold alloys. Although these elements exhibit the same effects on gold alloys, platinum is used with palladium because platinum is prone to segregation. Small amounts of zinc and iridium are also sometimes used as additional elements. Zinc is added to precious alloys for casting as a deoxidizing agent. Iridium cannot be melted easily as it has an extremely high melting point. When a small amount of fine powder iridium is added to a gold alloy, the iridium becomes a crystalline nucleus, promoting the refinement of crystal grains, inhibiting segregation, and improving corrosion resistance and mechanical properties. Dental casting gold alloys (gold-silver-copper alloys) contain at least 60 % gold, and gold + platinum group metals (Pt, Pd) contain at least 75 %. They are classified according to the amount of precious metals contained and their mechanical properties. Figure 12.9 shows the main types of dental casting gold alloys. The American Dental Association Standards (ADAS) and Japanese Industrial Standards (JIS) classify gold alloys into four types based on strength and elongation and define each gold alloy according to type. Standards for dental alloys have also been compiled in “ISO22674: Dentistry―Metallic materials for fixed and removable restorations and appliances.” For each of these types, there are gold-silver-copper alloys and gold-platinum alloys with the gold content shown in carats (K). For each composition or use, 22 to 18 K gold alloys are classified into gold alloy types 1, 2, or 3, and gold-platinum alloys for casting are classified as a type 4 gold alloy. All of these alloys are high-carat gold alloys for dental treatment. Some gold-platinum alloys are used for purposes other than casting.
Table 12.2
The effects of additional elements in gold alloys
Additional elements | Effects | |
|---|---|---|
Advantages | Disadvantages | |
Ag | Reduces redness | Decreases resistance to corrosion |
Cu | Lowers melting point, improves mechanical properties | Decreases resistance to corrosion, causes redness |
Pt | Improves strength and elasticity | Raises melting point, segregation |
Pd | Same as Pt | Raises melting point, decreases resistance to corrosion |
Zn | Prevents oxidation | Decreases resistance to corrosion |
Ir | Crystal grain refinement | – |
Fig. 12.9
Types of dental casting gold alloys
Within Japan, dental treatment is covered by health insurance. JIS T6113 [3] defines dental casting 14 K gold alloys as being suitable for coverage by health insurance. Under JIS, excluding types 1 to 4 and 14 K gold alloys, these are defined as medium-carat dental casting gold alloys with a gold content of 55mass% or greater and low-carat dental casting gold alloys containing a total amount of precious metals (gold and platinum group metals as additional elements) of 35mass% or greater.
Gold alloys separated according to type include gold-silver-copper-platinum-palladium-zinc-type alloys that contain gold, silver, and copper as the main components. As you can see in Table 12.3, which shows the composition of each type of gold alloy, the amount of copper increases from type 1 to type 4, whereas the amount of gold decreases. Platinum and palladium are mainly added to types 3 and 4. Copper lowers the melting point and improves hardness and strength. Platinum and palladium are mainly added to improve strength and elastic modulus. These alloys exhibit mechanical properties appropriate for the intended use. The more copper contained, the lower the melting point; however, the melting point rises when more platinum and palladium are added. Thus, JIS T6116 [4] dictates that the sum of these added elements cannot exceed 10mass% and the liquid phase points of gold alloy types 1 through 4 are each below 1,323 K.
Table 12.3
Composition of gold alloys by type
Gold alloy | Composition range (mass%) | |||||
|---|---|---|---|---|---|---|
Au | Ag | Cu | Pt | Pd | Zn | |
Type 1 | 80.2–95.8 | 2.4–12.0 | 1.6–6.2 | 0–1.0 | 0–3.6 | 0–1.2 |
Type 2 | 73.0–83.0 | 6.9–14.5 | 5.8–10.5 | 0–4.2 | 0–5.6 | 0–1.4 |
Type 3 | 71.0–79.8 | 5.2–13.4 | 7.1–12.6 | 0–7.5 | 0–6.5 | 0–2.0 |
Type 4 | 62.4–71.9 | 8.0–17.4 | 8.6–15.4 | 0.2–8.2 | 0–10.1 | 0–2.7 |
Table 12.4 shows the mechanical properties and main uses of the gold alloys by type. Gold alloy types 1 through 4 are defined as soft, medium hard, hard, and super hard in that order. In accordance with an increasing amount of added copper, hardness and strength increase, but elongation decreases. There are no stipulations regarding heat treatment for gold alloys other than type 4. However, types 3 and 4 can undergo hardening heat treatment (regular age hardening) using Au3Cu or AuCu superlattice and be used in large prosthodontic appliances that require strength.
Table 12.4




Mechanical properties and uses of gold alloys by type
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


