48
Cutaneous & Subcutaneous Mycoses
CHAPTER CONTENTS
INTRODUCTION
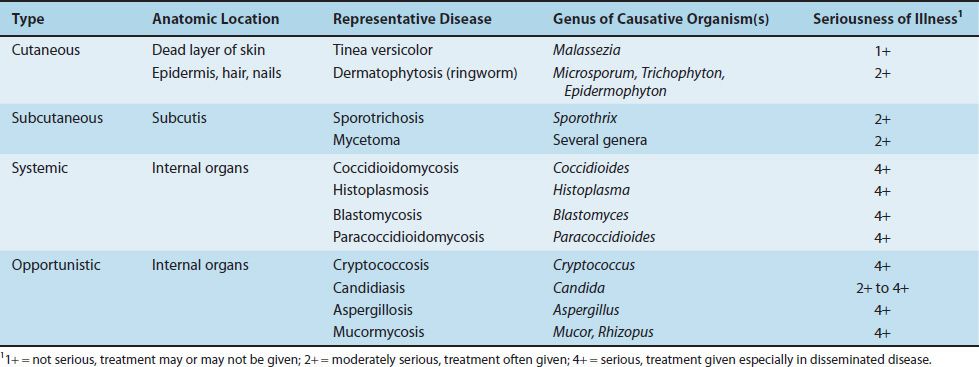
Medical mycoses can be divided into four categories: (1) cutaneous, (2) subcutaneous, (3) systemic, and (4) opportunistic. Some features of the important fungal diseases are described in Table 48–1. Cutaneous and subcutaneous mycoses are discussed in this chapter, and important features of the causative organisms are described in Table 48–2. The systemic and opportunistic mycoses are discussed in Chapters 49 and 50, respectively.
CUTANEOUS MYCOSES
Dermatophytoses
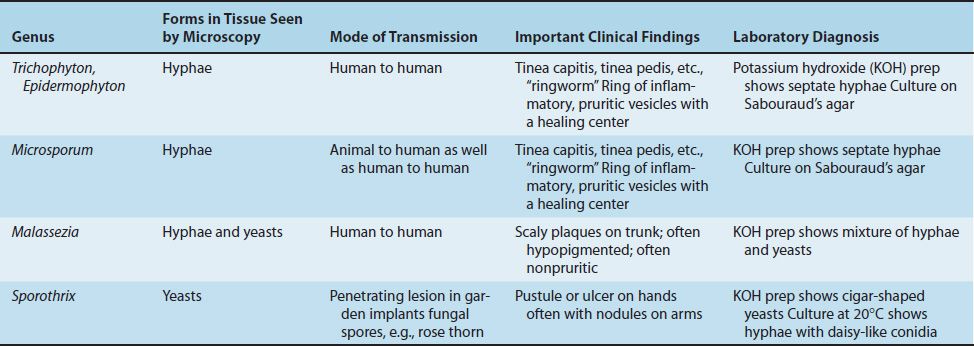
Dermatophytoses are caused by fungi (dermatophytes) that infect only superficial keratinized structures (skin, hair, and nails), not deeper tissues. The most important dermatophytes are classified in three genera: Trichophyton, Epidermophyton, and Microsporum. They are spread from infected persons by direct contact. Microsporum is also spread from animals such as dogs and cats. This indicates that to prevent reinfection, the animal must be treated also.
Dermatophytoses (tinea, ringworm) are chronic infections often located in the warm, humid areas of the body (e.g., athlete’s foot and jock itch).1 Typical ringworm lesions have an inflamed circular border containing papules and vesicles surrounding a clear area of relatively normal skin. The lesions are typically pruritic. Broken hairs and thickened broken nails are often seen. The disease is typically named for the affected body part (i.e., tinea capitis [head], tinea corporis [body], tinea cruris [groin], and tinea pedis [foot]) (Figure 48–1).
FIGURE 48–1 Tinea corporis (ringworm). Note oval, ring-shaped inflamed lesion with central clearing. Caused by dermatophytes such as Epidermophyton, Trichophyton, and Microsporum. (Reproduced with permission from Fauci AS, Braunwald E, Kasper DL et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill, 2008. Copyright © 2008 by The McGraw-Hill Companies, Inc.)
Trichophyton tonsurans is the most common cause of outbreaks of tinea capitis in children and is the main cause of endothrix (inside the hair) infections. Trichophyton rubrum is also a very common cause of tinea capitis. Trichophyton schoenleinii is the cause of favus, a form of tinea capitis in which crusts are seen on the scalp. Trichophyton species also cause an inflammatory pustular lesion on the scalp called a kerion. The marked inflammation is caused by an intense T-cell–mediated reaction to the presence of the fungus.
In some infected persons, hypersensitivity causes dermatophytid (“id”) reactions (e.g., vesicles on the fingers). Id lesions are a response to circulating fungal antigens; the lesions do not contain hyphae. Patients with tinea infections show positive skin tests with fungal extracts (e.g., trichophytin).
Scrapings of skin or nail placed in 10% potassium hydroxide (KOH) on a glass slide show septate hyphae under microscopy. Cultures on Sabouraud’s agar at room temperature develop typical hyphae and conidia. Tinea capitis lesions caused by Microsporum species can be detected by seeing fluorescence when the lesions are exposed to ultraviolet light from a Wood’s lamp.
Treatment involves local antifungal creams (terbinafine (Lamisil), undecylenic acid (Desenex), miconazole (Micatin), tolnaftate (Tinactin), etc.) or oral griseofulvin (Fulvicin). Prevention centers on keeping skin dry and cool.
Tinea Versicolor
Tinea versicolor (pityriasis versicolor), a superficial skin infection of cosmetic importance only, is caused by Malassezia furfur. The lesions are usually noticed as hypopigmented areas, especially on tanned skin in the summer. There may be slight scaling or itching, but usually the infection is asymptomatic. It occurs more frequently in hot, humid weather. The lesions contain both budding yeast cells and hyphae. Diagnosis is usually made by observing this mixture in KOH preparations of skin scrapings. Culture is not usually done. The treatment of choice is topical miconazole, but the lesions have a tendency to recur. Oral antifungal drugs, such as fluconazole or itraconazole, can be used to treat recurrences.
Tinea Nigra
Tinea nigra is an infection of the keratinized layers of the skin. It appears as a brownish spot caused by the melanin-like pigment in the hyphae. The causative organism, Cladosporium werneckii, is found in the soil and transmitted during injury. In the United States, the disease is seen in the southern states. Diagnosis is made by microscopic examination and culture of skin scrapings. The infection is treated with a topical keratolytic agent (e.g., salicylic acid).
SUBCUTANEOUS MYCOSES
These are caused by fungi that grow in soil and on vegetation and are introduced into subcutaneous tissue through trauma.
Sporotrichosis
Sporothrix schenckii is a dimorphic fungus. The mold form lives on plants, and the yeast form occurs in human tissue. When spores of the mold are introduced into the skin, typically by a thorn, it causes a local pustule or ulcer with nodules along the draining lymphatics (Figure 48–2). The lesions are typically painless, and there is little systemic illness. Untreated lesions may wax and wane for years. In human immunodeficiency virus (HIV)–infected patients with low CD4 counts, disseminated sporotrichosis can occur. Sporotrichosis occurs most often in gardeners, especially those who prune roses, because they may be stuck by a rose thorn.
FIGURE 48–2 Sporotrichosis. Note papular lesions on left hand and forearm. Caused by Sporothrix schenckii. (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree