Core Needle Biopsies
CORE NEEDLE BIOPSIES
Introduction
Core needle biopsy (CNB) can be used for initial evaluation of many types of breast lesions
Patients with benign findings can be spared surgical excision
Usually no cosmetic sequelae of breast deformity or skin scarring
No tissue scarring that could complicate mammographic interpretation
Patients with malignant findings also benefit
Multiple lesions can be sampled; helpful in determining number of cancers and extent
Widely spaced or very extensive cancers may require mastectomy
Generally require only 1 subsequent surgical procedure to remove cancer and sample lymph nodes if necessary
Information can be used to guide neoadjuvant therapy for eligible patients
Severe complications after CNB are very rare (< 1% of procedures)
CNB has advantages and disadvantages in comparison to fine needle aspiration (FNA) biopsy
FNA uses smaller needles: 18-, 20-, or 22-gauge
Can be performed on palpable masses or under image guidance
Slides can be interpreted immediately
Single cells rather than tissue are removed
Therefore, invasive carcinoma and carcinoma in situ cannot be distinguished with certainty
This information is important in deciding whether to sample nodes in subsequent procedure
Formalin-fixed, paraffin-embedded tissue sections are preferred specimen to perform special studies for ER, PR, and HER2
FNA is very useful for sampling palpable or enlarged nodes detected by ultrasound prior to planned neoadjuvant therapy
Documents presence of positive node but leaves metastasis in place to be evaluated for treatment response
Response in nodal metastases has more prognostic importance than response in breast
FNA is also useful for distinguishing solid from cystic lesions
Masses that can be aspirated to completion and need no further evaluation
If fluid is is not bloody, cytologic examination generally not performed
Types of CNB
Variety of needle sizes are used
16-g: Small size; use generally limited to very dense breast tissue that is difficult to penetrate
14-g: Standard size
11-g: Larger bore needle
2 main types of devices
Automated, spring-loaded biopsy gun with cutting needle
Multiple cores are required to sample lesion; may be obtained through single puncture site using a co-axial needle system
May be designated as clock face locations (12:00, 3:00, 6:00, 9:00) and central
Used ± imaging guidance
Vacuum-assisted devices
Employ a vacuum to draw tissue into needle
Remove multiple contiguous cores of tissue with 1 insertion
Permits use of larger diameter needles yielding larger specimens
Can be used under stereotactic, ultrasound, or MR guidance
14-g vacuum-assisted core biopsy is approximately 2x size of 14-g non-vacuum-assisted core
May remove entire lesion if numerous cores are taken
Clips
Generally deployed to mark site of biopsy in case excision is later required
Clips marketed by different manufacturers have different shapes
If > 1 lesion is biopsied, it is preferable to use clips of different shapes to ensure that each site can be identified
Clips are often deployed with gel pledgets
Pledgets fill cavity left by needle biopsy
Many are small, ovoid, rice-shaped particles; associated with chronic inflammatory reaction with giant cells
Larger rectangular gel pledgets are less resorbable and may be surrounded by pseudosynovial lining
Pledgets facilitate identification of core site in excisional specimen
In ˜ 20% of cases, clip is displaced from actual biopsy site; post-procedure radiograph should document location of clip
Identification of Targeted Lesion
Palpable lesions
May be sampled by freehand (TrucutTM) core needle biopsies
Needle biopsies without imaging tend to push lesions away rather than piercing them
If biopsy does not show definite mass-forming lesion (e.g., fibroadenoma or carcinoma), possibility of biopsy not sampling lesion must be considered
Stereotactic-guided biopsies
Can identify masses and calcifications
Masses also identified by ultrasound are more easily sampled using this technique
Ultrasound-guided biopsies
Can be used for visible lesions of any size if sufficiently suspicious
May be difficult to see masses < 1 cm
MR-guided biopsies
Require open coil and needles compatible with special techniques
Only performed for lesions that cannot be identified by other methods
SPECIMEN PROCESSING
Radiologist Handling
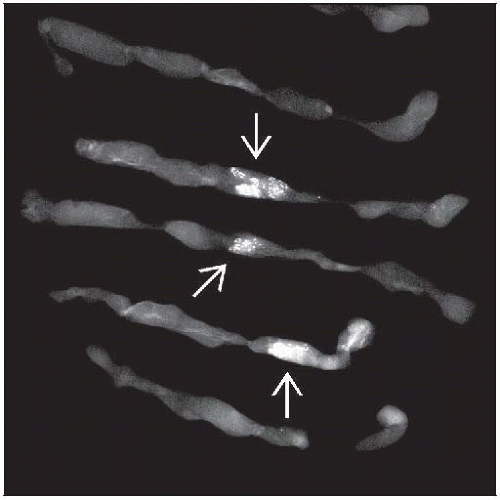
Biopsies for calcifications should be radiographed to ensure that calcifications have been sampled
Cores may be separated into those containing and not containing calcifications
Cores with calcifications may have more superficial sections taken during slide preparation to ensure they are not missed
If calcifications are not seen on initial H&E slides, additional levels can be obtained only on cores with radiologic calcifications
It is helpful for radiologist to wrap cores in thin paper and submit in tissue cassette in larger container of formalin
Ensures all tissue fragments are removed from formalin container
More likely to keep cores intact
More likely to preserve calcifications in tissue
As many cassettes as necessary for multiple cores can be used to ensure adequate formalin penetration and fixation
The time the cores are placed in formalin should be recorded to ensure they are fixed for sufficient amount of time prior to processing
Radiologist should provide information about targeted lesion(s)
Mode of detection (mammography, ultrasound, MR)
Type of lesion (mass, calcifications, architectural distortion, type of enhancement on MR)
For masses, provide shape (irregular, circumscribed/lobulated, ill defined)
Palpable or nonpalpable
Size of lesion
Distance between lesions if multiple lesions are present
Distance from prior excisional sites, if present
Specialized requisition forms for CNB can be utilized with relevant information in menu form
Pathology Processing
Cores wrapped in paper can be transferred to labeled cassette for processing
If there is too much tissue in cassette for adequate fixation, cores can be distributed into more cassettes
Histology Processing
Multiple levels are usually obtained on each biopsy
3 levels are generally adequate for diagnosis
3rd level should be approximately halfway through thickness of tissue
Allows for additional sections should additional studies be necessary
For MR biopsies with carcinoma, diagnosis is usually apparent on 1st level
Very small cancers are less likely to be detected by MR
Cores known to have calcifications may have superficial levels taken to make sure calcifications are not missed
REPORTING
General Considerations
Correlation with imaging findings is essential to ensure lesions are not missed
Requires adequate information about lesion from radiologist
Pathologist can document correlation with radiologic finding in some cases
Majority of carcinomas will be source of imaging lesion
Majority of fibroadenomas will be source of imaging lesion
In some cases there may be correlation, but pathologist cannot determine this with certainty
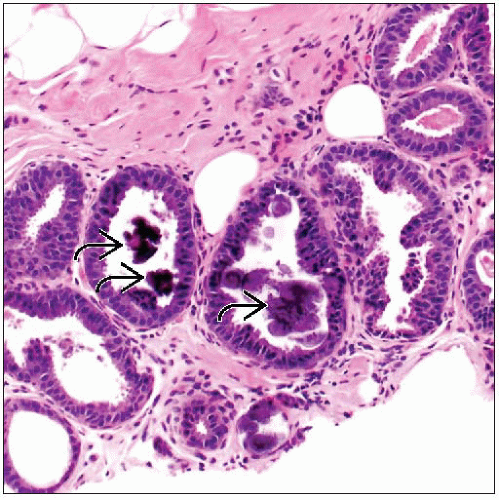
Cores for radiologic calcifications with only rare pathologic calcifications seen
Cores for masses with findings that do not have specific findings on core
e.g., lipoma, pseudoangiomatous stromal hyperplasia, hamartoma
In some cases, there clearly is not a correlation
Cores for calcifications without calcifications
Radiologic examination of block (direct and lateral views) may be considered to locate them in block
Additional deeper levels should be performed
Less common reasons for “calcifications” should be considered: Calcium oxalate, metallic debris from prior biopsies, gold from treatment for rheumatoid arthritis
Calcium oxalate is best seen using polarized light
Cores for mass lesions with only normal tissue identified
Radiology/pathology correlation conferences are useful for discussing difficult cases
Reporting Cancers
Ductal carcinoma in situ (DCIS)
Sometimes difficult to distinguish from atypical ductal hyperplasia (ADH) on CNB
Diagnosis may be deferred to excision for borderline lesions
Invasive carcinoma will be present on excision in some cases
More likely if targeted lesion is a mass
Correlation is better for vacuum-assisted biopsies that sample more tissue
Reduce number of cases with invasive carcinoma at surgical excision by at least 50%
ER may be performed on CNB
If results are negative, may be repeated on larger area in excision as there is often marked heterogeneity in DCIS
Lobular carcinoma in situ (LCIS)
LCIS may be present as incidental finding
If LCIS has atypical features, these should be clearly described
High nuclear grade
Necrosis
Association with calcifications
Excision is recommended for LCIS with atypical features due to higher risk of finding invasive carcinoma or DCIS
Invasive carcinoma
Useful to report maximum size as seen on CNB
Generally smaller than actual size
However, size on excision may be smaller than on core for small cancers
Helpful to judge reliability of special studies: If only small area of cancer is present on CNB and results are negative, repeat studies on excision may be warranted
Clinicians must understand that size on core should not be added to size on excision
Histologic type and grade are helpful for counseling patients about likely prognosis and treatment
Grade may be underscored in ˜ 1/3 of cases compared to excisions; rarely overscored
Special histologic types need to be reevaluated on excisional specimen
ER, PR, and HER2 may be evaluated
CNBs usually have minimal ischemic time and optimal formalin fixation
Minimum time for fixation is 6 hours for adequate antigen preservation; shorter times may result in false-negative results
However, amount of tumor available may be limited
In other cases, tissue disruption and crushing may make evaluation difficult or impossible
Repeat of negative results on larger areas of carcinoma on excision should be considered
Studies on larger areas of carcinoma may also be better for detecting cases of heterogeneous expression
For patients undergoing neoadjuvant treatment, results on CNB may be only documentation of their carcinoma
Tumor necrosis is predictive of response to therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree