Blood supply of colon and rectum.
•Vancomycin enemas can also be used if the patient has an ileus
•Fecal enemas from a donor (fecal transplant) for patients with recurrent or drug-resistant C. difficile
•High relapse rate (15%) after adequate therapy
•Consider a subtotal colectomy if the patient has worsening sepsis despite adequate medical treatment
•Other surgical indications include toxic megacolon, peritonitis, and organ failure
•High surgical mortality rate
Clostridium difficile colitis is associated with the use of all antibiotics including metronidazole, clindamycin (most common), penicillins, and cephalosporins.
A 38-year-old male with AIDS presents with lower Gastrointestinal (GI) bleeding. What is the most common cause for this bleeding?
Immunocompromised patients such as HIV and transplant patients are at risk for opportunistic infections. In the GI system, the most common opportunist is cytomegalovirus (CMV), causing colitis.
Lower GI Bleeding
•Etiologies include:
•Anatomic: Diverticulosis, Meckel diverticulum, hemorrhoids
•Vascular: Angiodysplasia, ischemia, radiation-induced
•Inflammatory: Inflammatory bowel disease (IBD), idiopathic
•Infections: C. difficile colitis, hemorrhagic E. coli
•Neoplastic
•Most common cause is diverticular disease (30% to 50%), yet only 15% of patients with diverticulosis will have bleeding
•Most diverticular bleeds occur in the absence of diverticulitis and resolve spontaneously
•Caused by disrupted vasa recta  arterial bleeding
arterial bleeding
•The most common cause of massive LGI bleeding is diverticulosis
•50% to 90% of diverticular bleeds occur on the right side while most diverticular disease is on the left side
•Angiodysplasia (Arteriovenous malformation, or AVM) is the most common cause of bleeding in elderly patients
•Most common in cecum or ascending colon
•Usually venous source
•Bleeding usually self-limited
•80% re-bleed if untreated
•20% to 30% patients also have aortic stenosis (Heyde syndrome).
•Treatment of bleeding includes argon plasma coagulation, endoscopic coagulation, injection sclerotherapy, or definitive surgical resection
•While treatment should be individualized, broad indications for surgery include:
•Transfusion of 4U PRBC within a 24-hour period
•Persistent bleeding after 72 hours
•Re-bleeding within 1 week of an initial episode
Remember that upper GI bleeding can cause lower GI bleeding. In fact, up to 15% of patients with lower GI bleeding have an upper GI source.
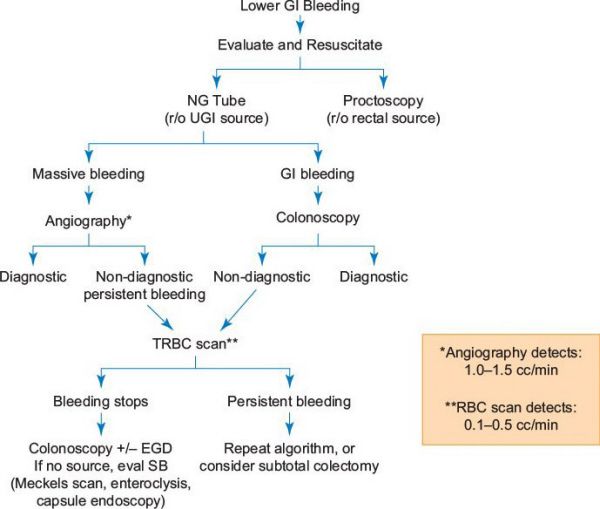
Workup of lower gastrointestinal (GI) bleeding.
An 82-year-old man underwent a hip replacement 8 days ago and now has a massively distended, non-tender abdomen. An abdominal X-ray (AXR) confirms marked colonic distension with a cecum measuring 9 cm and no obstruction seen on a gastrografin enema imaging study. What is the most likely diagnosis?
While identifying a possible source of obstruction is the first thought in any patient with a massively dilated colon, elderly patients without an obstruction are known to develop colonic pseudoobstruction, also known as Ogilvie syndrome.
Ogilvie Syndrome
•Massive dilation of colon without mechanical obstruction
•Common in elderly patients who are debilitated or have had recent surgery or trauma
•Must rule out mechanical obstruction with a water-soluble contrast enema or CT with rectal contrast
•Treatment
•Most (85%) resolve with conservative treatment
•Bowel rest
•Correct fluid-electrolyte imbalances
•Avoid narcotics and anticholinergics
•Rectal tube decompression
•If above measures fail or cecum is >10 to 12 cm:
•Consider a cholinesterase inhibitor (IV neostigmine)
•Neostigmine increases acetylcholine activity to induce coordinated colon propulsion
•90% success rate but 25% will recur
•Neostigmine is contraindicated in patients with cardiovascular disease, asthma, or on beta-blockers
•Must administer in a monitored setting with atropine available, as patients can become profoundly bradycardiac
•Consider colonoscopic decompression in patients who fail or have contraindications to neostigmine
•Cecostomy is an option if the patient fails the above measures
•Surgery is generally reserved for perforation or ischemia (rare)
•Procedure of choice is subtotal colectomy with end ileostomy
A 90-year-old female from a nursing home was noted to have obstipation and a significant increase in her abdominal girth. She is brought to the hospital where an AXR demonstrated large loops of redundant colon in the left lower quadrant. She has no peritoneal signs. What is the next step in management?
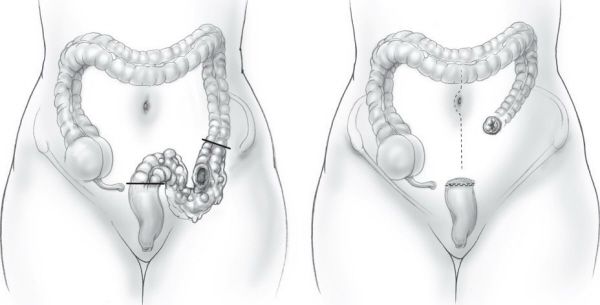
Unless the patient already meets criteria for a surgical resection (worsening sepsis, perforation, etc.), a rigid or flexible sigmoidoscopy should be performed for immediate decompression of a sigmoid volvulus.

Sigmoid volvulus. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Sigmoid Volvulus
•Sigmoid colon is the most common site for colonic volvulus
•Notorious in bedridden, institutionalized patients with neurologic or psychiatric conditions
•Risk factors: Redundant sigmoid colon, bedridden patients, chronic constipation
•Differential diagnosis includes obstructing colorectal cancer, cecal volvulus, and Ogilvie syndrome
•AXR shows dilated redundant colon and “bent inner tube” sign, which can extend anywhere from the pelvis to the RUQ
•Obtain a barium enema if AXR is equivocal
•A classic “bird’s beak” points to the site of obstruction
•Treatment is sigmoidoscopy to decompress and detorse the volvulus
•Success rate 85%
•Patients with perforation, peritonitis, hematochezia, gangrene or those who fail detorsion or fail to improve should undergo rapid resuscitation and surgical resection
60% of patients will have a recurrence after endoscopic detorsion and patients should undergo elective resection (sigmoid colectomy) during the same hospitalization. These patients should be nutritionally optimized and undergo full colonoscopy in the interim.
A 55-year-old woman presents with severe abdominal pain. Physical exam reveals a distended abdomen that is tympanitic and diffusely tender. She has a marked leukocytosis. AXR shows a dilated cecum extending to the left upper quadrant. A gastrografin enema confirms the diagnosis of cecal volvulus. What is the next step?
An ileocecectomy or right colectomy to include the involved area is indicated.
Cecal Volvulus
•Less common than sigmoid volvulus
•Differential diagnosis is the same as that for sigmoid volvulus
•Treatment is resection with right hemicolectomy
•Despite higher risk of recurrence, cecopexy can be considered in:
•Poor medical candidates with a short life expectancy, with viable bowel
•Patients with mild symptoms caused by cecal bascule (chronic intermittent obstruction caused by a floppy cecum that folds on itself leading to obstruction)
There is no role for neostigmine in the management of volvulus.
A 78-year-old man is found to have a stricture in the sigmoid colon on contrast studies. He has a history of multiple attacks of diverticulitis. What is the next step in his management?
A stricture often recurs following endoscopic dilatation. Surgical resection of the stricture with primary colon anastomosis is the definitive treatment and will rule out neoplasia.
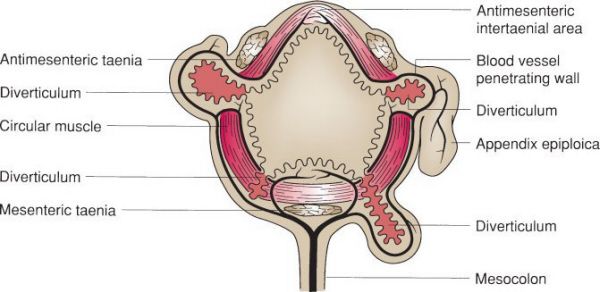
Relation of diverticula to blood vessels. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Diverticular Disease
•“False” diverticula—involve herniation of the mucosa through the muscularispropria
•90% of diverticular disease involves the sigmoid
•35% of patients have disease outside the sigmoid
•Incidence rises with age; 30% to 50% by age 60, 80% by age 85
•Most patients are asymptomatic
•One-third of patients present with complications (bleeding, abscess, stricture, or acute perforation)
•Surgery is only indicated for patients with diverticular complications, recurrent bleeding, or multiple hospitalizations
•One-third of patients require an operation
A 67-year-old woman presents with a 1-day history of fever, left lower quadrant pain, and leukocytosis. AXR shows significant free air. What is the most likely diagnosis?
Perforated diverticulitis is a common cause of sudden left lower quadrant pain and free air.
•A CT scan with oral and IV contrast helps establish the diagnosis
•Right-sided (atypical) diverticulitis is more common in younger and Asian patients
•Hinchey classification
•Stage I: Confined pericolic abscess
•Stage II: Distant abscess (retroperitoneal or pelvic)
•Stage III: Purulent peritonitis due to rupture of pericolonic/pelvic abscess but without communication with bowel
•Stage IV: Fecal peritonitis due to free perforation of diverticulum with communication with bowel
•Treatment
•Mild diverticulitis: A course of oral broad-spectrum antibiotics and a low-residue diet
•Must cover E. coli and Bacteroides fragilis
•Severe diverticulitis: IV antibiotics, IV fluids, bowel rest and analgesics
•If an abscess is seen, percutaneous drainage followed by elective resection in 6 to 12 weeks
•Patients with generalized peritonitis and fecal contamination or worsening sepsis (Stage III or IV) require immediate surgery
•All patients should undergo colonoscopy 6 weeks after episode of diverticulitis to rule out neoplasia
•High recurrence rate
•30% recur after first episode and 30% recur after second episode, however complications are most likely to occur with first episode
•Elective resection recommended for patients with uncomplicated diverticulitis when the frequency and severity of episodes impact quality of life
•Elective resection recommended after the first episode in immunosuppressed due to higher recurrence and complication rates
•Elective operation is a simple resection with primary anastomosis
•Choice of operation in an emergent situation depends on degree of inflammation and contamination
•Anastomosis of severely inflamed/contaminated ends of bowel should be avoided given the risk of non-healing and subsequent leakage
•Emergency operation choices include:
•Hartmann procedure (resection of involved colon with the proximal end brought out as an end colostomy)
•Resection with primary anastomosis ± proximal diversion with a “protective” diverting loop ileostomy
•Placement of large external drains at the site of perforation ± proximal diversion with an ostomy (useful choice when dissection is very dangerous)
•4% to 10% can recur even after surgical resection, especially when a portion of sigmoid colon is left in place
The choice to perform a diverting ostomy depends on the bowel tissue integrity and the degree of inflammation and contamination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


