CHAPTER 8
Colistin and Polymyxin B
LISA M. VOIGT, PharmD, BCPS
KIMBERLY T. ZAMMIT, PharmD, BCPS, FASHP
Antimicrobial resistance has become a worldwide health care crisis with many pathogens showing limited or no susceptibility to currently available antimicrobial treatments. Gram-negative infections are of even more concern because of the lack of currently effective treatments, as well as the lack of new antibiotics in development to treat these potentially lethal pathogens. It is currently estimated that no new antibiotics with activity against multiresistant gram-negative bacteria will be released within the next five years, emphasizing the need for last-line options, such as colistin, in cases where pathogens are resistant to all other antibiotics. In the last two decades, the paucity of novel antibiotics with which to treat drug-resistant infections, especially those caused by gram-negative pathogens, has led to their reconsideration as a therapeutic option.1
Polymyxins are a group of polypeptide antibiotics that consists of five chemically different compounds (polymyxins A–E) discovered in 1947. Only polymyxin B and polymyxin E (colistin) have been used in clinical practice. They differ by a single amino acid change (D-phenylalanine in polymixin B replaces D-leucine in colistin). Polymyxins have been used extensively worldwide in topical otic and ophthalmic solutions for decades.2 The mechanism behind colistin’s bactericidal ability is considered to be identical to that of polymyxin.1
Colistin was discovered in 1949 and was nonribosomally synthesized by Bacillus polymyxa subspecies colistinus Koyama.3-4 Colistin was initially used therapeutically in Japan and in Europe during the 1950s and in the United States in the form of colistimethate sodium in 1959.5 However, the intravenous formulations of colistin and polymyxin B were gradually abandoned in most parts of the world in the early 1980s because of the reported high incidence of nephrotoxicity.6-8
This chapter review focuses on colistin, rather than polymyxin B, because of its wider use in current clinical practice.
MECHANISM OF ACTION
The initial target of the antimicrobial activity of polymyxins is the lipopolysaccharide (LPS) component of the outer membrane. The polymyxins have a strong positive charge and a hydrophobic acyl chain that give them a high binding affinity for LPS molecules. They interact electrostatically with these molecules and competitively displace divalent cations (Mg2++ and Ca2++) from them, causing disruption of the membrane. The result of this process is an increase in the permeability of the cell envelope, leakage of cell contents, and, subsequently, cell death. The exact mechanism by which the polymyxins induce bacterial killing is still unknown, and multiple bacterial cell targets may be involved. Polymyxins also bind to the lipid A portion of LPS and, in animal studies, block many of the biological effects of endotoxin.9
FORMULATIONS, DOSAGE, AND ROUTE OF ADMINISTRATION
Colistin is composed of at least 30 different polymyxin compounds, mainly colistin A and B. Two forms of colistin are available: colistin sulfate and the commercially available parenteral formulation colistimethate sodium (CMS, also called sodium colistin methanesulphonate, colistin methanesulphonate, colistin sulfomethate, or colistimethate). It is extremely important to note that the two forms are not interchangeable. CMS is an inactive prodrug and in aqueous solution, CMS undergoes spontaneous hydrolysis to the active form colistin.10
As a prodrug, CMS is readily hydrolyzed to form partially sulfomethylated derivatives, as well as colistin sulfate, the active form of the drug. This hydrolysis of CMS to colistin is an important step in providing the drug’s antimicrobial activity. Up until colistin is formed, CMS by itself has been shown to display little to no antibacterial activity, and is therefore considered an inactive prodrug of colistin.11 CMS is eliminated mainly by the renal route, with a fraction of the dose being converted to active colistin in vivo. Colistin undergoes extensive renal tubular reabsorption and therefore is mainly cleared by nonrenal mechanisms. CMS is administered intravenously or intramuscularly, because it is less toxic than colistin sulfate. The intramuscular injection, which is rarely used in clinical practice, may cause severe local pain, and absorption is variable.9 Solutions of colistimethate sodium for IM injection, IV injection, or continuous IV infusion should be freshly prepared and used within 24 hours.9
Colistin sulfate is administered either orally (for bowel decontamination, without absorption) or topically (for the treatment of bacterial skin infections). Both colistimethate sodium and colistin can be given via inhalation, but colistin may result in a higher frequency of bronchoconstriction than colistimethate sodium. Colistimethate sodium can also be administered by the intrathecal or intraventricular routes.9
LACK OF A UNIVERSAL DOSAGE UNIT FOR COLISTIN
Coly-Mycin M Parenteral, which is manufactured and used in the United States, contains 150 mg of colistin base activity (CBA) per vial, equivalent to 400 mg of colistimethate sodium per vial and to 5 × 106 international units (IU) of colistimethate sodium. Colomycin injection, which is manufactured and used in Europe, is provided in vials containing 5 × 106 or 2 × 106 IU of colistimethate sodium. An IU is defined as the minimal concentration that inhibits the growth of Escherichia coli 95 I.S.M in 1 mL broth at pH 7.2 and 106 IU is considered to be equivalent to 80 mg of colistimethate sodium.9
The complexity of the nomenclature used to define colistin dosing has resulted in much confusion, increasing the potential for drug errors. The need for utilization of a uniform dosing unit to avoid such confusion is obvious.12,13 In June 2011, a National Alert for Serious Medication Errors was issued by the American Society of Health-System Pharmacists (ASHP) and the Institute for Safe Medication Practices (ISMP), warning that potentially fatal errors may occur with dosing for colistimethate for injection.13 Particular attention must be paid to the dosing units used in various drug information sources and scientific literature to avoid utilization of incorrect doses.
ASHP/ISMP Recommendations for Safe CMS Use13
• In the United States, colistimethate for injection must ONLY be prescribed as colistin in terms of base activity with dose range of 2.5–5 mg/kg/day in patients with normal renal function. As per package insert, use ideal body weight for obese patients. This total daily dose should be given in 2 to 4 divided doses.
• Dosage reduction in the setting of renal insufficiency is recommended (see product labeling for suggested modification of dosage schedules).
• If the drug is ordered as “colistimethate” or “colistimethate sodium,” the prescriber should be contacted to verify the dose in terms of colistin base.
• Consider restricting ordering to infectious disease specialists or intensivists.
• To prevent errors, preapproved printed guidelines or computer order sets should be made available with dosing only as colistin base. Include adjustments for renal dysfunction.
• Dose limits should be established with immediate investigation required for doses outside hospital guidelines. Guidelines should define any circumstances where dosing outside the 2.5–5 mg/kg/day range may be appropriate. Testing of CPOE and pharmacy computer systems should be accomplished to assure proper function of alerts.
• Monitoring of renal function while receiving colistin is important to detect signs of renal toxicity associated with colistin, and the appropriateness of dosage should be reevaluated periodically while on treatment.
The ASHP/ISMP recommendation for dosing unit convention will be followed in this chapter (see Table 8-1). Unless otherwise specified all dose recommendations are made in milligrams of colistin base activity (CBA).
| TABLE 8-1 | Comparison of Colistimethate Sodium Products |
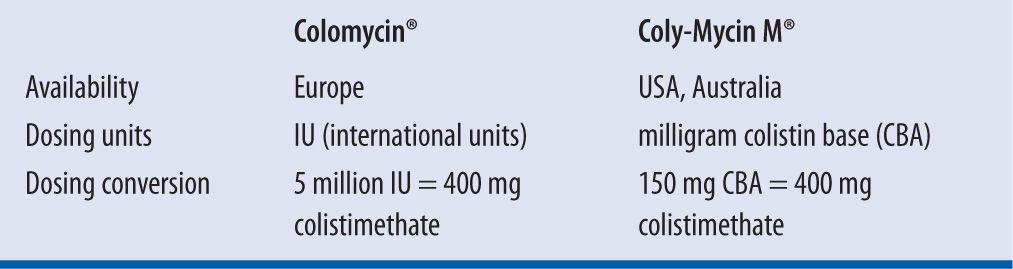
30 mg colistin base = 80 mg CMS = 1 MIU (European international units)
1 mg colistin base = 2.67 mg CMS = 33,333 IU; 1 mg CMS = 12,500 IU
Source: Adapted from van Duin D, Kaye KS, Neuner EA. Carbapenem-resistant Enterobacteriaceae: A review of treatment and outcomes. Diagn Microbiol Infect Dis. 2013;75(2):115–120.
NEPHROTOXICITY
One of the commonly observed adverse effects following intravenous administration of colistimethate sodium is nephrotoxicity, with incidences reported to be as high as 55 percent in the following studies. In studies comparing treatment with colistimethate sodium with or without other antibiotics versus other antibiotic regimens, nephrotoxicity was significantly higher with colistimethate sodium (or polymyxin B) in six studies, similar to that with comparators in five (two of which claimed no events), and lower in two that may actually be less nephrotoxic than aminoglycosides. Rates of nephrotoxicity in recent studies designed to assess this outcome have ranged from 6 percent to 14 percent in some20-24 and from 32 percent to 55 percent in others.25-30
The wide range of nephrotoxicity rates can be at least partly explained by different definitions of renal failure. Some studies used any of the RIFLE criteria (risk, injury, failure, loss, and end-stage kidney disease).31 Some used the threshold of failure or above, and others defined renal failure as creatinine >2 mg/dL. Risk factors for nephrotoxicity found in different studies included older age,26,29 preexisting renal insufficiency,32 hypoalbuminaemia,27 and concomitant use of nonsteroidal anti-inflammatory drugs27 or vancomycin.29 Higher dosing is associated with renal failure, with some studies identifying the total cumulative dose as predictive of renal failure,3,24,25 and others the daily dose.26,29-30 The time to nephrotoxicity was not reported in most studies. Four studies reported that most cases occurred within the first week of treatment.26,28-30 Studies monitoring patients for 1–3 months after treatment demonstrated reversibility of renal failure in at least 88 percent of patients.21,25,27 Overall, rates of nephrotoxicity are probably lower today than those observed in old studies.3 Explanations for the lower toxicity include fewer chemical impurities in colistimethate sodium, better intensive care unit (ICU) monitoring, and avoidance of coadministration of other nephrotoxic drugs.33,34 Recent observations have suggested that, at least in CF patients, colistimethate sodium may actually be less nephrotoxic than aminoglycosides.35
NEUROTOXICITY
Neurotoxicity is less common than nephrotoxicity. Clinical manifestations include dizziness, muscle weakness, paresthesias, partial deafness, visual disturbances, vertigo, confusion, hallucinations, seizures, ataxia, and neuromuscular blockade. Paresthesias constitute the most common clinical manifestation, being reported in approximately 27 percent of cases with the use of intravenous colistimethate sodium. Neurotoxic effects are usually mild and resolve after prompt discontinuation of the antibiotic.34 Apnea and respiratory failure, which are feared complications of neuromuscular blockade, have not been reported with intravenous colistimethate sodium in the recent literature.34
RESPIRATORY EFFECTS
Bronchoconstriction15-19 and hypersensitivity pneumonitis36 have been reported in adult and pediatric cystic fibrosis patients who received oral nebulized CMS. Bronchoconstriction occurs almost immediately after initiation of nebulization and may persist for more than 30 minutes.16 Administration of bronchodilators prior to colistin nebulization may reduce the potential for development of bronchoconstriction.15-19 Pre- and posttreatment pulmonary function tests may have clinical utility to identify individuals at risk for bronchoconstriction.16 In those individuals who are unable to perform pulmonary function tests (especially young children), bronchodilator premedication is recommended.19 It should also be noted that in critically ill patients without CF, these adverse events have not yet been demonstrated.37-45
Both CMS and colistin can be given via inhalation, but colistin may result in a higher frequency of pulmonary adverse effects than colistimethate sodium. A component of colistin (polymyxin E1) has been shown to cause pulmonary inflammatory reactions in animals and may contribute to such local toxicity in humans. Given the fact that colistmethate sodium is hydrolyzed to colistin in aqueous solutions and potentially serious pulmonary toxicity, including fatal respiratory failure, has been associated with the administration of premixed product, inhalation solutions should be prepared immediately prior to administration.15 The Food and Drug Administration and the Cystic Fibrosis Foundation underscored the importance of this practice by issuing an alert recommending that patients not use colistimethate for inhalation premixed by pharmacies and that patients should prepare their colistimethate nebulizer inhalation solutions immediately prior to use.15
SPECTRUM OF ACTIVITY AND RESISTANCE
Colistin is bactericidal against most strains of gram-negative bacilli, including Enterobacter aerogenes, Escherichia coli, Haemophilus influenza, Bordetella pertussis, Legionella pneumophilia, Salmonella species, Shigella species, Pasteurella species, Klebsiella pneumonia, Pseudomonas aeruginosa, and Stenotrophomonas maltophilia. However, some bacteria are resistant to colistin, including the gram-negative organisms of Proteus species, Burkholderia cepacia, Providencia species, Serratia marcescens, Moraxella catarrhalis, and Morganella morganii. Gram-positive bacteria, fungi, and gram-negative cocci (Neisseria gonorrhoeae and Neisseria meningitides) are inherently resistant to colistin.46-48
P. aeruginosa and A. baumannii susceptibility are defined as MICs of ≤4 and ≤2 mg/L colistin sulfate, respectively, according to the European Committee on Antimicrobial Susceptibility Testing,49 and as an MIC of ≤2 mg/L for both bacteria according to the Clinical and Laboratory Standards Institute (CLSI).50
Isolates with intrinsic resistance to polymixins have alterations in lipid A that account for reduced binding.47 But acquired resistance to colistin has been historically deemed to be infrequent, although this may simply be a function of the drug’s relatively limited use. Emergence of resistance has been increasingly reported and it is likely mediated by alteration in the negatively charged bacterial cell membrane, although additional mechanisms may also be involved. Inadequate dosing may also be a factor in the development of resistance due to preferential growth within heteroresistant subpopulations. As such, optimization of dosing is necessary to achieve desired therapeutic outcomes.51,52
DRUG INTERACTIONS53
Colistimethate may increase the levels/effects of neuromuscular-blocking agents. Case reports have described potentiation of neuromuscular blockade of pancuronium when concomitantly given polymyxin B. Antagonizing the block was not successful with pyridostigmine or calcium chloride.54 Neuromuscular blockade from Polymyxin B alone has been reported in both medical and surgical patients not receiving anesthetic or other neuromuscular blocking drugs. It also potentiates d-tubocurarine- and succinylcholine-induced blockades.55 The levels/effects of colistimethate may be increased by aminoglycosides, amphotericin B, and vancomycin. Concomitant use with BCG (M. tuberculosis vaccine) should be avoided.
PHARMACOKINETICS
The pharmacokinetics of colistimethate sodium and colistin are complex and incompletely characterized. The antimicrobial activity of colistimethate requires conversion to colistin, and thus its rate of conversion impacts peak concentrations.11 The overall disposition of colistin is rate limited by the elimination of the parent compound, because the colistin has a substantially longer terminal half-life than CMS.51 Complete understanding of the pharmacokinetics of colistimethate sodium and colistin continues to evolve, as studies using HPLC and not immunoassays allow better characterization of the disposition of each drug. It is important to note that the pharmacokinetic and prescribing information supplied with currently available parenteral products was obtained using microbiological assays.51
Palchouras and colleagues60 conducted a pharmacokinetic study of 18 critically ill patients administered CMS 3 million units (240 mg CMS) every 8 hours, with a reduction to 160 mg q8h for those whose creatinine clearance was less than 50 mL/min. Plasma samples for drug concentration analysis were obtained with the first and fourth dose. A nonlinear mixed-effects model analysis was performed in which all concentration-time data were modeled simultaneously. The predicted maximum concentrations of drug in plasma were 0.60 mg/liter and 2.3 mg/liter for the first dose and at steady state, respectively. Colistin displayed a half-life that was significantly long in relation to the dosing interval (14.6 hours). This study suggests that administration of a loading dose may be more beneficial in critically ill patients as plasma colistin concentrations are insufficient before steady state.
A subsequent study57 evaluated the disposition of the prodrug, CMS, and formed colistin in 105 critically ill patients, including 12 on intermittent hemodialysis and 4 on continuous renal replacement therapy. Of the 105 patients, 69 had creatinine clearances of less than 40 mL/min/1.73 m2. This study demonstrated important information concerning the disposition of CMS and colistin. First, it revealed the significant role of renal function as a determinant of the plasma concentrations of the active antibacterial, formed colistin. Second, it is apparent that in patients with moderate-to-good renal function, utilization of a daily dose of CBA at the high end of manufacturer recommended doses (300 mg CBA per day)53 was not able to generate plasma colistin concentrations that would be expected to be reliably efficacious.
It is also important to note that the disposition of the active component colistin is remarkably flat for >14 hours, which may limit the optimization of the dose without unacceptable toxicity. Therefore, based on our current understanding of colistin PK and pharmacodynamic relationships, colistin may best be used as part of a highly active combination, especially for patients with moderate-to-good renal function and/or for organisms with MICs of ≥1.0 mg/L.57
DISTRIBUTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


