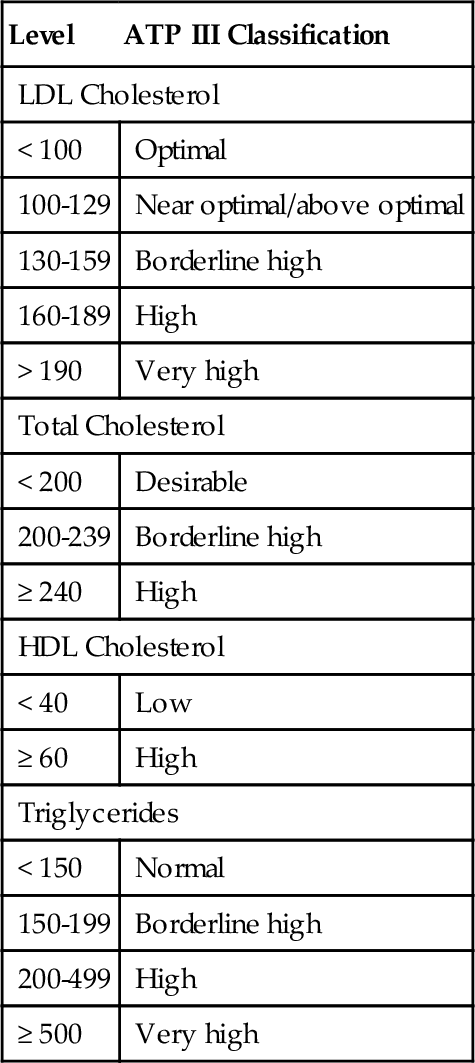
Chapter 7 Tilla S. Worgall; Steven L. Spitalnik; Jeffrey S. Jhang A. Free cholesterol and triglycerides (TGs). B. Cholesteryl esters and TGs. C. Free cholesterol and cholesteryl esters. D. Phospholipids and TGs. E. Free cholesterol and phospholipids. 2. The National Cholesterol Education Program Expert Panel (NCEP), Adult Treatment Panel III (ATP III), recommends that patients achieve which one of the following values for total cholesterol? B. < 150 mg/dL. C. < 200 mg/dL. D. < 239 mg/dL. E. < 240 mg/dL. 3. Plasma lipoproteins are divided into five major classes. These lipoprotein classes contain different concentrations of TGs, free cholesterol, esterified cholesterol, phospholipids, and apoproteins. Classification is based on their density, which ranges from less than 0.95 g/mL to about 1.20 g/mL. Which one of the following best describes the relationship between density and diameter? B. Density and diameter are inversely proportional: High-density particles are the smallest lipoproteins. C. There is no relationship between density and diameter. 4. Most plasma cholesterol is carried as cholesteryl esters in which one of the following types of lipoprotein particle? B. Very-low-density lipoprotein (VLDL). C. Low-density lipoprotein (LDL). D. Intermediate-density lipoprotein (IDL). E. High-density lipoprotein (HDL). 5. Which one of the following statements regarding genetically determined hyperlipidemias is true? A. Increased chylomicrons are characteristic of type I hyperlipidemia. B. Defective LDL receptor binding results in low plasma cholesterol levels and high TG levels. C. Type III hyperlipidemia is associated with homozygosity for the ApoE E4/E4 genotype and results in equally increased cholesterol and TG levels. D. Type IIb hyperlipidemia is associated with increased LDL and HDL levels. E. Type V hyperlipidemia, or mixed hyperlipidemia, is associated with increased VLDL and LDL levels. 6. Which one of the following correctly describes the origin of plasma LDL? A. LDL originates directly from dietary uptake of cholesterol. B. LDL is synthesized by intestinal epithelium. C. LDL is secreted by the liver. D. LDL originates from chylomicron hydrolysis. E. LDL originates from VLDL hydrolysis. 7. Based on the 2001 recommendations of the NCEP ATP III, patients should be tested initially for which one of the following groups of parameters? A. Total cholesterol and HDL cholesterol. B. Total cholesterol, LDL cholesterol, HDL cholesterol, and TGs. C. Total cholesterol, LDL cholesterol, HDL cholesterol, TGs, and chylomicrons. D. Total cholesterol, HDL cholesterol, and LDL subfractions (i.e., small dense LDL particles). E. Total cholesterol, LDL cholesterol, HDL cholesterol, and chylomicrons. 8. Statin (3-hydroxy-3-methyl-glutaryl-CoA [HMG-CoA] reductase inhibitor) therapy lowers plasma cholesterol levels by which one of the following mechanisms? A. Increased upregulation of liver LDL receptors. B. Decreased uptake of cholesterol by enterocytes. C. Increased synthesis of anticholesterol particles. D. Increased secretion of cholesterol into bile. E. Decreased synthesis of apoprotein B. 9. A 10-year-old girl presents to her pediatrician with elevated orange-yellow xanthomas present superficially over her knees, wrists, and interdigital webs. These physical findings are characteristic for which one of the following conditions? B. Hepatic lipase deficiency. C. Diabetic dyslipidemia. D. Familial hypercholesterolemia. E. Metachromatic leukodystrophy. 10. Cholesteryl ester transfer protein (CETP) is a potential therapeutic target to decrease atherosclerotic disease. Which one of the following statements best describes the effect of CETP? A. CETP transfers cholesteryl esters from chylomicrons to HDL, thereby producing VLDL particles. B. CETP transfers cholesteryl esters from LDL to HDL particles, which are then cleared by the HDL receptor. C. CETP increases cholesteryl ester content in VLDL particles. The cholesteryl esters in the circulation are then cleared by the liver through VLDL receptors. D. CETP increases cholesteryl ester content in HDL particles. The cholesteryl esters in the circulation are then cleared by the liver through HDL receptors. E. CETP transfers TGs from apolipoprotein B (ApoB)-containing lipoproteins to HDL in exchange for cholesteryl esters. The cholesteryl esters in the circulation are then cleared by the liver through LDL receptors. 11. Which one of the following statements best describes the finding(s) in a patient with ABCA1 deficiency (i.e., Tangier disease)? A. Increased ApoA1 on plasma LDL particles. B. Absence of LDL particles in plasma. C. Very low plasma HDL cholesterol levels accompanied by lipid accumulation in peripheral cells. D. Fasting TG levels of more than 100 mg/dL, which may rise to more than 10,000 mg/dL postprandially. E. Milky plasma characterized by increased circulating levels of chylomicrons. 12. Which one of the following findings best characterizes lecithin cholesterol acyltransferase (LCAT) deficiency? A. Large chylomicrons and VLDL with very high TG levels. B. Decreased HDL levels. C. Elevated LDL levels. D. Increased LDL receptors expressed on the cell surface. E. Increased lysolecithin. 13. Which one of the following best describes the changes associated with activation of the LDL receptor pathway? B. Increased HMG-CoA reductase activity, decreased ACAT activity, and decreased expression of LDL receptors. C. Decreased HMG-CoA reductase activity, decreased ACAT activity, and decreased expression of LDL receptors. D. Decreased HMG-CoA reductase activity, decreased ACAT activity, and increased expression of LDL receptors. E. Increased HMG-CoA reductase activity, increased ACAT activity, and increased expression of LDL receptors. 14. Which one of the following is the intraindividual physiologic variation in serum cholesterol? B. 6.5%. C. 8%. D. 20%. E. 50%. 15a. Which one of the following is the goal value for LDL cholesterol in patients with coronary heart disease (CHD) or CHD risk equivalent according to the recommendations made by the NCEP ATP guidelines? B. < 65 mg/dL. C. < 100 mg/dL. D. < 160 mg/dL. E. < 200 mg/dL. 15b. Which one of the following is the cutoff value for a “high” HDL cholesterol according to the recommendations made by the NCEP ATP? B. > 40 mg/dL. C. < 60 mg/dL. D. > 60 mg/dL. E. < 100 mg/dL. Major points of discussion ■ Free cholesterol is a component of phospholipid membranes. ■ Cholesteryl esters are the storage form of cholesterol. The ester bond between the carboxylate group of a fatty acid (primarily linoleic acid or oleic acid) and the hydroxyl group of cholesterol is formed by the enzyme acyl-CoA cholesteryl acyltransferase (ACAT). Cholesteryl esters are more hydrophobic than cholesterol. ■ Phospholipids are mainly found on the surface of the lipoprotein particle. ■ TGs are esters, each composed of glycerol and three fatty acids. These fatty acids can be saturated or unsaturated. The fatty acids of most naturally occurring TGs contain 16, 18, or 20 carbon chains. 2. A. < 100 mg/dL. Major points of discussion ■ The NCEP ATP III guidelines from 2002 identify major risk factors for CHD that modify the goal for LDL cholesterol. NCEP guidelines have shifted the focus from recognizing abnormal and normal cholesterol values to assessing overall cardiovascular risk based on cutoffs for cholesterol, TGs, HDL cholesterol, and LDL cholesterol (Table 7-1). ■ The ATP III guidelines introduced several new concepts for the evaluation of hyperlipidemia. Diabetes mellitus is now considered a risk equivalent because it confers a high risk for new CHD within 10 years. This means that for evaluation of elevated cholesterol levels, diabetic patients are treated like patients who already have CHD. Also, ATP III recognized patients with metabolic syndrome and patients with a high 10-year risk for CHD based on the Framingham risk projections as candidates for intensive intervention and therapy. ■ Risk status in persons without clinically manifested CHD or other clinical forms of atherosclerotic disease is determined by a two-step procedure. First, the number of risk factors is counted. Second, for persons with multiple (2 +) risk factors, 10-year risk assessment is carried out with Framingham scoring to identify individuals whose short-term (10-year) risk warrants consideration of intensive treatment. Estimation of the 10-year CHD risk adds a step to risk assessment beyond risk factor counting, but this step is warranted because it allows better targeting of intensive treatment to people who will benefit from it.3 3. A. Density and diameter are directly proportional: High-density particles are the largest lipoproteins. Major points of discussion ■ Density correlates inversely with diameter. HDL particles (density, 1.063 to 1.1210 g/mL) are the lipoprotein fraction with the smallest diameter (~ 6 to 12 nm). Chylomicrons (density, < 0.93 g/mL) are the lipoproteins with the highest diameter (80 to 1200 nm). The density is determined by the amount of lipid per particle. ■ Cholesterol accounts for almost all of the sterol in plasma. It exists as a mixture of unesterified (30% to 40%) and esterified (60% to 70%) forms; the proportion of the two forms is fairly constant among normal individuals. Enzymatic methods of cholesterol quantification have virtually replaced the chemical methods that were used for most clinical and research purposes. Enzymatic methods measure total cholesterol directly in plasma or serum through a series of reactions in which cholesteryl esters are hydrolyzed. The 3-OH group of free cholesterol is then oxidized, and hydrogen peroxide, one of the reaction products, is quantified enzymatically. ■ Currently, homogeneous assays are the most popular method for measuring HDL cholesterol. Unlike precipitation methods, these fully automated two-reagent procedures do not require off-line pretreatment and separation (hence the term homogeneous) and can be adapted to most chemistry analyzers. Thus, they reduce hands-on time and overall assay costs. Test kits distributed in the United States are based on various methods. Usually, the first reagent forms a stable complex with non-HDL lipoproteins, preventing them from participating in the reaction, and the second reagent releases HDL-cholesterol that is then measured enzymatically. According to surveys of the College of American Pathologists, the most common method uses a synthetic polymer together with a polyanion to block non-HDL lipoproteins, followed by a selective detergent to release HDL cholesterol (Genzyme Diagnostics, Cambridge, MA; Beckman Coulter, Inc Brea, CA). Other methods use polyethylene glycol–modified enzyme (Roche Diagnostics, Indianapolis), or immunoinhibition (Wako Chemicals USA, Inc., Richmond, VA) to block non-HDL lipoproteins. A fourth method (Polymedco Inc., Cortland Manor, NY) uses a special reagent to selectively eliminate cholesterol in non-HDL lipoproteins, followed by a second reagent that releases cholesterol from HDL (Denka Seiken Co., Niigata, Japan). These methods generally are not affected by high TGs, bilirubin, and globulins. ■ LDL cholesterol plays a causal role in the development of atherosclerosis. An LDL cholesterol level of more than 160 mg/dL with no other risk factors is an indication for therapy. With two or more CHD risk factors, the upper limit is lowered to 130 mg/dL for initiation of therapy. Several methods have been used to measure LDL cholesterol. The first, a reference laboratory procedure, involves ultracentrifugation to separate LDL from other lipoproteins, followed by analysis as described previously, to measure cholesterol. A much more common second method uses the Friedewald formula to calculate LDL cholesterol. Finally, more recently developed homogeneous methods for measuring LDL cholesterol are now available. ■ LDL cholesterol can be determined by using the Friedewald formula, originally described by Friedewald, Levy, and Fredrickson in 1972. Generally, in fasting plasma samples, LDL contains the cholesterol that is not present in HDL or VLDL. Thus, LDL cholesterol can be determined by the following equation:
Clinical Chemistry
Lipids and Glycoproteins
B. < 150 mg/dL.
C. < 200 mg/dL.
D. < 239 mg/dL.
E. < 240 mg/dL.
Rationale: The NCEP ATP III guidelines recommend a total cholesterol of less than 200 mg/dL.
Rationale: Density correlates inversely with diameter. (HDL particles are the lipoprotein fraction with the smallest approximately 6 to 12 nm in diameter. The density is determined by the amount of lipid per particle.
B. Density and diameter are inversely proportional: High-density particles are the smallest lipoproteins.
C. There is no relationship between density and diameter.
Rationale: Density correlates inversely with diameter. HDL particles (density, 1.063 to 1.1210 g/mL) are the lipoprotein fraction with the smallest diameter (~ 6 to 12 nm). Chylomicrons (density, < 0.93 g/mL) are the lipoproteins with the highest diameter (80 to 1200 nm). The density is determined by the amount of lipid per particle.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine