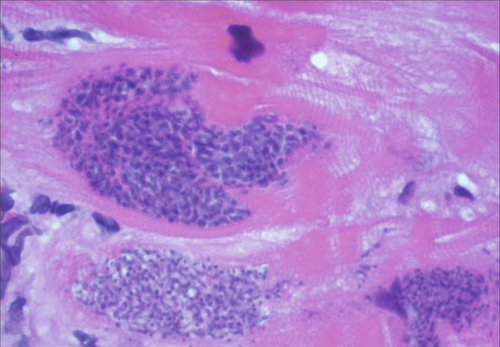
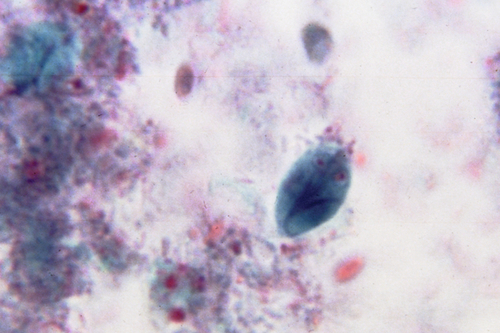
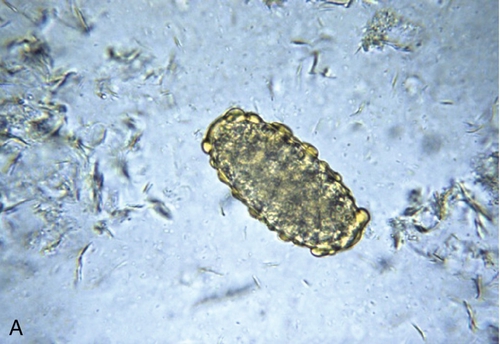
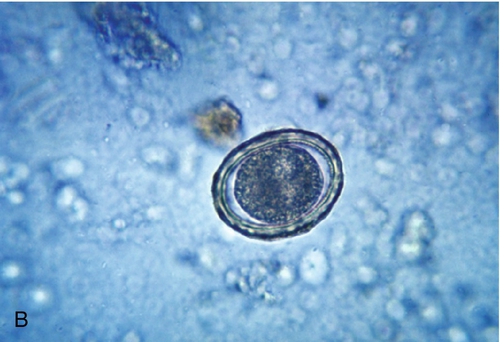
Chapter 18 1. A 56-year-old female patient presents complaining of fatigue 11 months after receiving a heart transplant. The organ donor emigrated from South America 15 years previously. An endomyocardial biopsy was performed, and the histologic results are shown in Figure 18-1. Which one of the following pathogens is shown? B. Listeria monocytogenes. C. Toxoplasma gondii. D. Trypanosoma cruzi. E. Cytomegalovirus (CMV). 2. A 14-year-old boy presents to his pediatrician with a 1-week history of abdominal pain, diarrhea, and foul-smelling flatulence. Two weeks before presentation, he was camping with his scout troop and may have ingested water from a nearby stream. Direct examination of a fresh stool sample is shown Figure 18-2. Which one of the following is the etiologic agent causing this patient’s illness? B. Trichomonas hominis. C. Cryptosporidium parvum. D. Chilomastix mesnili. E. Giardia intestinalis. 3. Which one of the following is the insect vector responsible for transmitting the organism seen in Figure 18-3? B. Anopheline mosquito. C. Reduviid bug. D. Ixodes scapularis. E. Black fly. 4. A 6-year-old boy presented with a 1-month history of decreased appetite and abdominal pain. He resides with his parents on a farm in rural South Carolina. No other family members are ill. Microscopic examination of a stool sample is illustrated in Figure 18-4. Which one of the following is the etiologic agent causing his infection? B. Necator americanus. C. Trichuris trichiura. D. Enterobius vermicularis. E. Ascaris lumbricoides. 5. A 12-year-old bone marrow transplant recipient presented to the emergency department with nonspecific influenza-like symptoms, including fever, chills, and myalgia. Initial laboratory test results were consistent with hemolytic anemia. The hematology technologist observed abnormal findings on the smear (Figure 18-5) and referred the slide to the microbiology laboratory. Relevant past medical history includes a blood transfusion 1 month before admission and no recent travel, although his parents confirmed a trip to the Ivory Coast 3 years ago. Which one of the following is the etiologic agent seen in the figure? B. Toxoplasma gondii. C. Plasmodium ovale. D. Ehrlichia chaffeensis. E. Babesia microti. 6. A 50-year-old pig farmer, a recent immigrant to the United States from Indonesia, presented to his local emergency department with a 3-week history of diarrhea. Examination of his stool demonstrated the ciliated pathogen shown in Figure 18-6. Which one of the following is the etiologic agent? B. Enterocytozoon species. C. Balantidium coli. D. Iodamoeba bütschlii. E. Leishmania species. 7. A 40-year-old man, recently returned from China, has experienced abdominal discomfort of 1 month’s duration. He was subsequently found to have biliary duct obstruction. Stool examination demonstrated the ovum shown in Figure 18-7. Which one of the following trematodes is the etiologic agent of his illness? B. Fasciola hepatica. C. Fasciolopsis buski. D. Clonorchis sinensis. E. Paragonimus westermani. 8. Which one of the following parasites is a liver fluke and infects the biliary ducts of humans? B. Paragonimus species. C. Diphyllobothrium latum. D. Strongyloides stercoralis. E. Wuchereria bancrofti. 9. A 7-year-old boy presents to his pediatrician with a 5-day history of watery diarrhea, nausea, vomiting, and a low-grade fever. There was no recent travel history, and his other family members were not symptomatic. He had attended a birthday party at an indoor water park 2 weeks before this presentation. Which one of the following is the etiologic agent (shown in Figure 18-8) causing this patient’s gastrointestinal disease? B. Isospora belli. C. Enterocytozoon bienusi. D. Cyclospora cayetanensis. E. Giardia intestinalis. 10. Which one of the following parasites cannot be classified as a helminth? B. Echinococcus granulosis. C. Taenia solium. D. Trichuris trichuria. E. Fasciola hepatica. 11. A 4-year-old girl presented to her pediatrician with a 1-week history of abdominal pain and increased bowel movements producing greenish-brown, watery diarrhea. Several children attending her day care center were experiencing similar symptoms. Which one of the following is the etiologic agent shown in Figure 18-9? B. Giardia intestinalis. C. Cyclospora cayetanensis. D. Entamoeba histolytica. E. Chilomastix mesnili. 12. Echinococcosis, or hydatid disease, is an infection by larval tapeworms of the genus Echinococcus. Which one of the following statements regarding this infection is correct? B. The large majority of hydatid cysts occur in the lung through blood dissemination from the intestine. C. Echinococcus species are classified as liver and lung trematodes. D. The genus Echinococcus contains four species for which humans are an accidental host. E. Immunodiagnostic tests are not useful in diagnosing hydatid disease because of poor sensitivity resulting from the inability of antigen to be released from the cysts. 13. A 4-year-old girl presented with complaints of severe perianal itching. Other children attending her day care setting had similar symptoms. The etiologic agent is shown in Figure 18-10. Which one of the following is the cause of this patient’s infection? B. Ascaris lumbricoides. C. Ancylostoma duodenale. D. Necator americanus. E. Trichuris trichiura. 14. A 21-year-old female college student presented to the student clinic complaining of a 1-week history of diarrhea and stomach cramps. She had traveled to rural Central America for humanitarian purposes 1 month before presentation. Direct examinations of stained fecal material are shown in Figure 18-11. Which one of the following is the etiologic agent responsible for this patient’s gastrointestinal disease? B. Blastocystis hominis. C. Iodamoeba bütschlii. D. Entamoeba histolytica. E. Endolimax nana. 15. A 40-year-old female patient presented to the emergency department of her local hospital with a 5-day history of watery diarrhea, abdominal cramps, and chills. She had been informed that several family members who also attended a wedding 2 weeks before had similar symptoms, which motivated her to seek medical attention. Stool specimens were collected for bacterial culture, viral studies, and parasitology examinations. A rapid antigen detection test was performed (Figure 18-12). Which one of the following statements provides the best interpretation of these results? A. The patient has cryptosporidiosis. B. The device indicates a false-positive reaction for Cryptosporidium. C. The patient may have a dual infection with Giardia and Cryptosporidium. D. The patient’s current diarrheal illness is not due to either Giardia or Cryptosporidium. E. The test results are inconclusive, and another sample should be tested. 16. Many blood-borne pathogens are transmitted by an insect (vector). Which of the following parasites is not vector transmitted? B. Plasmodium species. C. Leishmania species. D. Trypanosoma cruzi. E. Babesia microti. 17. A patient presented to his primary care physician with a rash consistent with erythema migrans. He had removed the ectoparasite, similar to the one shown in Figure 18-13, several days earlier. The patient was prescribed doxycycline and recovered uneventfully. Which one of the following is the most likely infectious disease for which the patient was successfully treated? B. Lyme disease. C. Anaplasmosis. D. Tularemia. E. Rocky Mountain spotted fever. 18. Which one of the following blood collection tubes is optimal for preparing blood smears for the diagnosis of malaria? A. Gold top (serum separator). B. Green top (sodium heparin). C. Gray top (fluoride/oxalate). D. Light blue top (citrate). E. Lavender top (ethylenediaminetetraacetic acid [EDTA]). 19. A 21-year-old college student presented to his physician with a 2-week history of flu-like symptoms, including fever, chills, and malaise. Two months before presentation, he spent 1 week in rural areas of the Dominican Republic as part of a school- based charitable mission. Laboratory tests were ordered, and the technologist reported an unusual observation, which is shown in Figure 18-14. Which one of the following is the best first-line therapy to recommend for this patient? B. Oral doxycycline. C. Intravenous artesunate. D. Oral chloroquine. E. Oral atovaquone-proguanil. 20. The size of the parasite is critical in distinguishing between parasites in stool that may be morphologically similar. Which one of the following best represents the standard of practice that must be followed to identify parasites accurately in stool specimens? A. Examine specimens in preservative only. B. Use a calibrated ocular micrometer. C. Use an antigen detection test. D. Observe the specimen under oil immersion. E. Determine the number of ova and cysts per field. 21. A 37-year-old woman presented to the emergency department with a 3-week history of severe headaches and two episodes of seizures. She is a recent immigrant from a rural area of Mexico and was in her usual state of good health until this presentation. Cultures and radiologic examinations were obtained. Computed tomography demonstrated several ring-enhancing cerebral calcifications. Subsequent serologic testing confirmed the diagnosis. Which one of the following is the most likely etiologic agent in this case? A. Nocardia asteroides complex. B. Mixed anaerobic bacterial infection. C. Streptococcus mitis. D. Taenia solium. E. Cryptococcus neoformans. 22. A 50-year-old woman presented to her primary care physician with complaints of a 2-week history of chronic cough and hemoptysis. She had traveled through rural parts of China during the previous month. Stool examinations demonstrated the ovum shown in Figure 18-15. Which one of the following parasites is the most likely etiologic agent of this patient’s illness? B. Fasciola hepatica. C. Paragonimus westermani. D. Diphyllobothrium latum. E. Clonorchis sinensis. 23. Which one of the following is not an acceptable practice to ensure stool integrity for morphologic identification of parasites? A. Preserve stool in polyvinyl alcohol (PVA). B. Refrigerate stool. C. Preserve stool in sodium acetate–acetic acid formalin (SAF). D. Examine stool immediately. E. Preserve stool in ethanol. 24. A 25-year-old woman presented to her physician with a 2-week history of fever, chills, and headache. Physical examination was significant for splenomegaly. She had recently returned from a 1-month trip to the Philippines where she was staying primarily with relatives in rural areas. Figure 18-16 demonstrates the positive findings of a blood smear preparation. Which one of the following is the most likely etiologic agent in this case? B. Plasmodium vivax. C. Plasmodium falciparum. D. Ehrlichia chaffeensis. E. Babesia microti. 25. An ovum of which one of the following trematodes is shown in Figure 18-17? B. Schistosoma mansoni. C. Fasciola hepatica. D. Paragonimus westermani. E. Schistosoma japonicum. 26. A patient with HIV/AIDS presented to the hospital with a 2-week history of headaches, weakness, and slurred speech. The results of a computed tomography scan with contrast and a magnetic resonance imaging revealed multiple ring-enhancing lesions. Tissue from a brain biopsy was negative on an acid-fast stain. Serodiagnostic tests were positive for the etiologic agent. Which one of the following is the most likely infectious cause of the brain lesions in this patient? B. Cryptosporidium parvum. C. Mycobacterium tuberculosis. D. Entamoeba histolytica. E. Balamuthia mandrillaris. 27. Some parasites are causative agents in transfusion-related infections. Which one of the following parasites is not transmitted by blood transfusion? B. Trypanosoma cruzi. C. Toxoplasma gondii. D. Plasmodium species. E. Strongyloides stercoralis. 28. Two siblings, 7 and 10 years old, presented to their pediatrician with a 2-day history of fever, facial swelling, and muscle pain. Two weeks earlier, they attended a county fair and consumed pork sandwiches, potato salad, and ice cream. Based on a blood smear, which demonstrated an eosinophilia of 20%, a biopsy was obtained (Figure 18-18). Which one of the following is the most likely etiologic agent for these children’s illness? B. Wuchereria bancrofti. C. Trichinella spiralis. D. Trichomonas hominis. E. Trichuria trichuria. 29. A 23-year-old woman presented to her doctor with a vaginal discharge that was frothy and malodorous (i.e., “fishy odor”). Which one of the following parasites (Figure 18-19) is the most likely cause of her infection? B. Gardnerella vaginalis. C. Treponema pallidum. D. Mobiluncus species. E. Trichomonas vaginalis. 30. A 19-year-old college student presented to the emergency department complaining of redness, pain, and decreased vision in his left eye. His level of discomfort prevented him from wearing his contact lenses for the previous 2 days. Corneal scrapings were obtained and inoculated on various microbiologic media. Which one of the following is the etiologic agent seen in Figure 18-20? B. Herpes simplex virus. C. Adenovirus. D. Acanthamoeba. E. Balamuthia. Major points of discussion ■ Chagas’ disease is endemic in Mexico, South America, and Central America. ■ Vector-borne transmission occurs when the infected triatomine bug (the “kissing bug”) takes a blood meal and defecates on the human target. The parasite-infected feces enter through mucous membranes or breaks in the skin. ■ The acute phase of Chagas’ disease is often asymptomatic and can last weeks to months. One sign of acute disease is called Romaña’s sign, manifested by swelling of the eyelids on the side of the face near the bite wound. ■ In the United States, antiparasitic therapy includes nifurtimox or benznidazole, both of which are available only through the Centers for Disease Control and Prevention (CDC). 2. A. Cyclospora cayetanensis. Major points of discussion ■ The G. intestinalis trophozoite is teardrop shaped and has four pairs of flagella, two nuclei, two linear axonemes, and two curved median bodies. The cyst form is oval and contains four nuclei, axenomes, and median bodies. ■ Giardia is transmitted by swallowing infectious cysts found in contaminated food or water. Water sources, such as ponds, lakes, and streams, harbor G. intestinalis cysts because of fecal contamination by animals and/or humans. ■ Rapid immunochromatographic screening methods are more sensitive than routine ova and parasite examinations. Duodenal aspirates may also be examined for the presence of the parasite. ■ Effective therapy for giardiasis includes metronidazole and nitazoxanide. ■ Hallmark symptoms of giardiasis are explosive watery, foul-smelling diarrhea and flatulence. 3. A. Tsetse fly. Major points of discussion ■ For diagnosis, both thick and thin Giemsa-stained blood smears are required, and 200 to 300 oil immersion fields should be examined. ■ P. falciparum infects all ages of red blood cells (RBCs) and infected RBCs appear to be of normal size. ■ The stages of P. falciparum observed by direct examination of blood smears are RBCs infected with multiple young trophozoite rings and/or banana-shaped gametocytes. ■ In the absence of gametoctyes, the travel history of the patient is critical because babesiosis can mimic P. falciparum infection.8,10 4. A. Ancylostoma duodenale. Major points of discussion ■ Infection is primarily acquired by ingestion of fertilized eggs present in the soil. Unfertilized Ascaris eggs are noninfectious. ■ The life cycle of Ascaris includes migration of larvae to the lungs, where they eventually migrate through alveolar walls, up the bronchus, and then are swallowed. Adult worms then develop in the small intestine. Loeffler syndrome is the pulmonary manifestation of the lung phase, which can include cough, dyspnea, and hemoptysis. ■ Diagnosis of the pulmonary phase of ascariasis is often made by visualizing larvae in expectorated sputum. ■ The drug of choice for treatment of ascariasis is albendazole. Mebendazole, ivermectin, and nitazoxanide are satisfactory alternatives.5 5. A. Plasmodium falciparum. Major points of discussion ■ Cases of transfusion-related babesiosis are on the rise. Infected blood donors appear healthy, and blood donation protocols do not currently include laboratory test screening for Babesia. ■ Diagnosis is based on microscopic identification of the organism on Giemsa-stained peripheral blood smears. Findings include RBCs infected with multiple ring forms (early trophozoites), which can sometimes appear as a tetrad or “Maltese cross” (Figure 18-5. B) and as extra-erythrocytic trophozoites. ■ Typically, the level of parasitemia for babesiosis is only 1% to 2%, but it can be more than 10% in immunocompromised patients, in which case RBC exchange transfusion may be indicated. ■ Babesiosis is usually treated with combination therapy, such as atovaquone and azithromycin or clindamycin and quinine. 6. A. Chilomastix mesnili. Major points of discussion ■ B. coli infection is usually limited to the intestines and is ingested in fecally contaminated food or water. Individuals who have close contact with pigs are commonly infected. ■ B. coli is best identified using wet mounts of stool because the parasite does not stain adequately. They can be seen and identified under low or high power because of their large size. ■ The symptoms associated with balantidiasis include diarrhea, dysentery, and abscess formation. ■ The treatment of choice for balantidiasis is tetracycline, although metronidazole and iodoquinol can be used as alternatives. 7. A. Schistosoma haematobium. Major points of discussion ■ C. sinensis miracidia are ingested by freshwater snails, which are the first intermediate host. ■ Cercariae are released from the snail host and encyst (referred to as metacercariae) in the skin of freshwater fish or on vegetation, which are the second intermediate hosts. ■ The most serious complication of infections with C. sinensis is cholangiocarcinoma, or cancer of the bile duct. ■ Praziquantel is the drug of choice for treating infections with C. sinensis. 8. A. Clonorchis species. Major points of discussion ■ Liver flukes are associated with neoplasia of the bile duct and cholangiocarcinoma, in particular, in elderly patients. ■ The laboratory diagnosis of C. sinensis is made by examining multiple stool specimens and comparing the size and morphology of the eggs (Table 18-1). Table 18-1
Microbiology
Parasitology


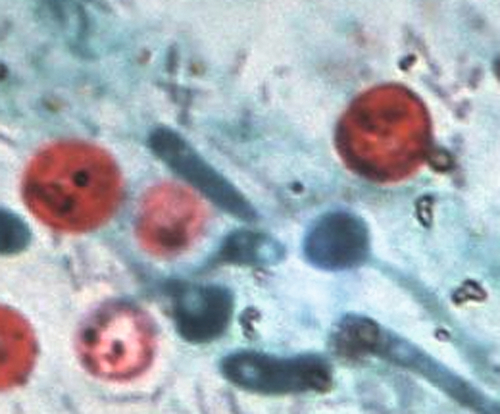
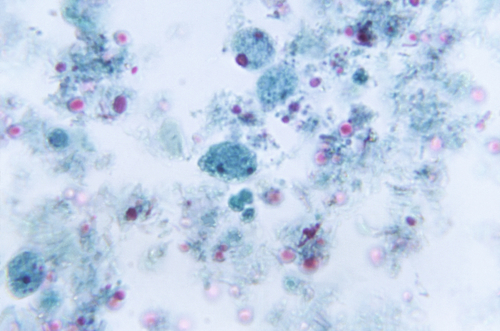

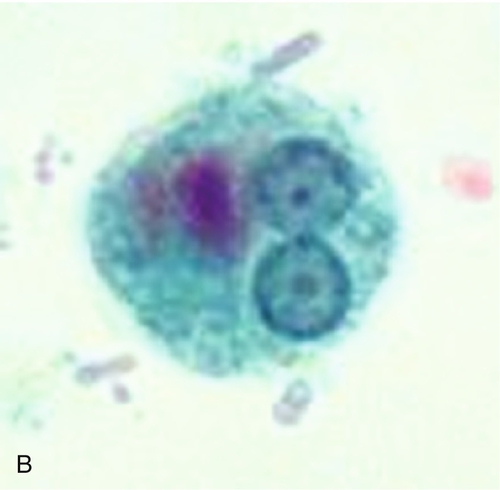




Rationale: C. cayetanensis is a pathogenic intestinal coccidia characterized by small oocysts that are positive in a modified acid-fast stain and have much thicker walls than C. parvum.
B. Trichomonas hominis.
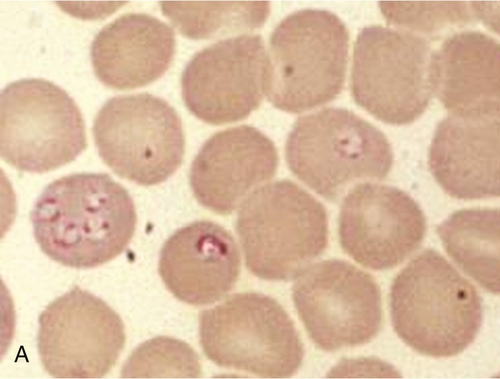
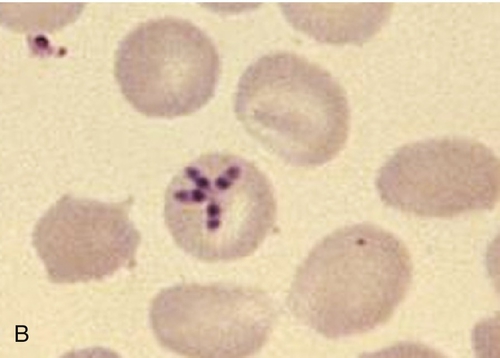
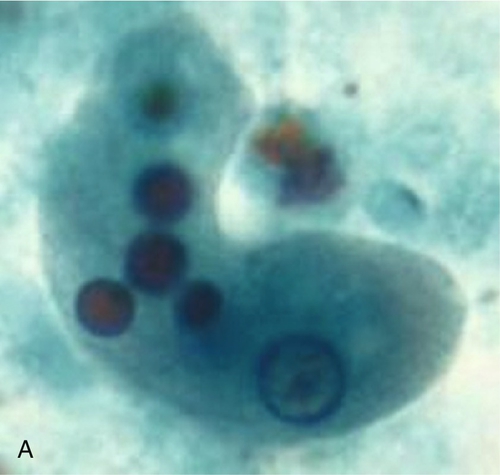
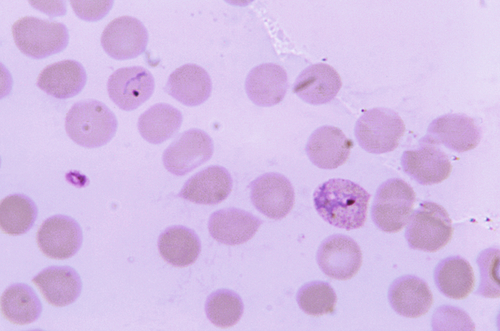
Rationale: T. hominis is a nonpathogenic intestinal flagellate with a single nucleus.
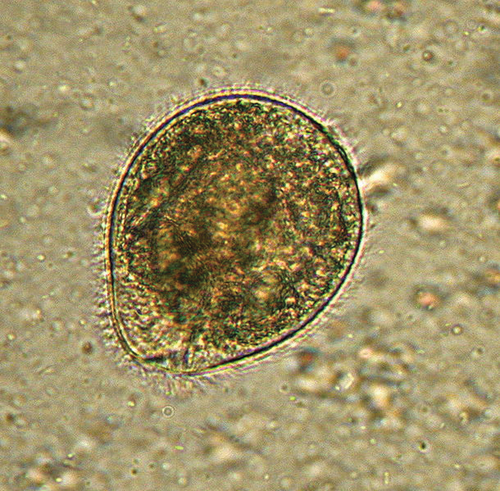
C. Cryptosporidium parvum.
Rationale: C. parvum is a pathogenic intestinal coccidia characterized by small oocysts that are positive in a modified acid-fast stain.
D. Chilomastix mesnili.
Rationale: C. mesnili is a nonpathogenic intestinal flagellate with a single nucleus.
E. Giardia intestinalis.
Rationale: G. intestinalis is a pathogenic intestinal flagellate with two nuclei.
Rationale: The tsetse fly is the vector responsible for transmitting Trypanosoma brucei.
B. Anopheline mosquito.
Rationale: The figure demonstrates a gametocyte of P. falciparum, a blood parasite transmitted by the female Anopheles mosquito.
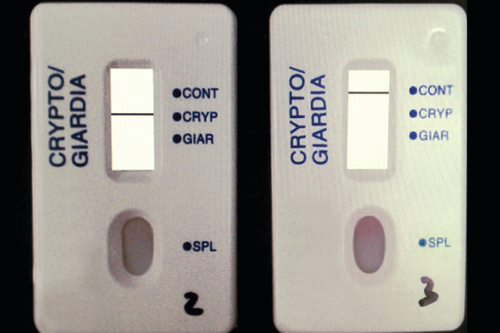
C. Reduviid bug.
Rationale: The reduviid bug, a triatomid, is the vector responsible for transmitting T. cruzi.
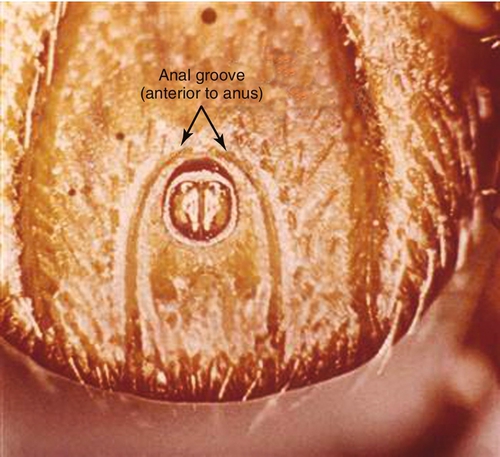
D. Ixodes scapularis.
Rationale: I. scapularis is the tick responsible for transmitting Borrelia burgdorferi, the causative agent of Lyme disease.
E. Black fly.
Rationale: The black fly is the vector for transmission of Onchocerca volvulus, which is associated with river blindness.
Rationale: The Ancylostoma (hookworm) egg is oval, thin shelled, and colorless and usually contains 8 to 16 embryonic cells. This egg cannot be distinguished from N. americanus.
B. Necator americanus.
Rationale: The Necator (hookworm) egg is oval, thin shelled, and colorless and usually contains 8 to 16 embryonic cells. This egg cannot be distinguished from that of A. duodenale.
C. Trichuris trichiura.
Rationale: The Trichuris (whipworm) egg is elongated, yellowish brown, and barrel shaped, with colorless polar plugs at each end.
D. Enterobius vermicularis.
Rationale: The Enterobius (pinworm) egg is elongated, oval, colorless, and flattened on one side.
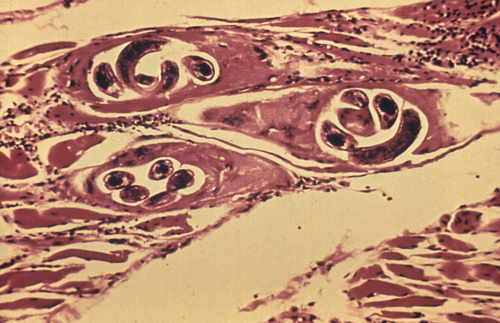
E. Ascaris lumbricoides.
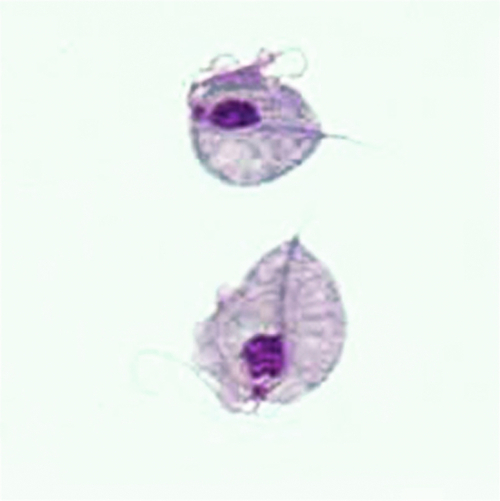
Rationale: The unfertilized Ascaris (roundworm) egg is elongated and brown, with a bumpy (i.e., mammillated) shell (Figure 18-4, A). The fertilized egg is ovoid and brown with a thick smooth shell (Figure 18-4, B).
Rationale: P. falciparum is characterized by RBCs infected with multiple ring forms. However, P. falciparum does not have a dormant liver stage, as with P. vivax and P. ovale infection, which would recrudesce 3 years after relevant travel.
B. Toxoplasma gondii.
Rationale: T. gondii is a protozoan parasite, characterized by crescent-shaped tachyzoites, which can sometimes be observed within Giemsa-stained leukocytes.
C. Plasmodium ovale.
Rationale: P. ovale typically demonstrates many developmental stages in peripheral blood and is not characterized by RBCs infected with multiple ring forms.
D. Ehrlichia chaffeensis.
Rationale: E. chaffeensis is an intracellular bacterial species that infects mononuclear leukocytes and appears as clusters of bacteria called morulae.
E. Babesia microti.
Rationale: B. microti is a protozoan parasite, characterized by RBCs infected with multiple ring forms, and has been transmitted through infected blood products.
Rationale: C. mesnili is a flagellated intestinal protozoan.
B. Enterocytozoon species.
Rationale: Enterocytozoon species is a microspordium and an obligate intracellular parasite. It is neither ciliated nor flagellated.
C. Balantidium coli.
Rationale: B. coli is the only ciliated parasite that infects humans.
D. Iodamoeba bütschlii.
Rationale: I. bütschlii is an intestinal ameba that moves sluggishly by means of cytoplasmic protrusions called pseudopods.
E. Leishmania species.
Rationale: Leishmania is a hemoflagellate that circulates in the bloodstream or may be present in lymph nodes or muscle.
Rationale: The egg of S. haematobium is 112 to 170 μm in length, has a yellow-brown shell, and has a distinct lateral spine.
B. Fasciola hepatica.
Rationale: The egg of F. hepatica is 130 to 150 μm in length, has a yellow-brown shell, and has an operculum but no opercular shoulders.
C. Fasciolopsis buski.
Rationale: The egg of F. buski is 130 to 140 μm in length, has a transparent shell, and has an operculum with no opercular shoulders at the narrower end.
D. Clonorchis sinensis.
Rationale: The egg of C. sinensis, or the liver fluke, is 20 to 35 μm in length, has a thick yellow-brown shell, and has an operculum with opercular shoulders.
E. Paragonimus westermani.
Rationale: The egg of P. westermani, or the lung fluke, is 80 to 120 μm in length, has a thick brown-yellow shell, and has an operculum with opercular shoulders.
Rationale: The trematode C. sinensis causes biliary infection and is known as the Chinese or Oriental liver fluke.
B. Paragonimus species.
Rationale: Paragonimus species is a lung fluke.
C. Diphyllobothrium latum.
Rationale: D. latum is an intestinal cestode or tapeworm.
D. Strongyloides stercoralis.
Rationale: S. stercoralis is an intestinal nematode (i.e., a roundworm).
E. Wuchereria bancrofti.
Rationale: W. bancrofti is a filarial nematode (i.e., a roundworm) that causes elephantiasis.
Trematode
Common Name
Foodborne Source
Definitive Host
Egg Size (μm)
Presence of Embryo in Egg
Clonorchis sinensis
Chinese liver fluke
Uncooked freshwater fish
Fish-eating mammals (e.g., dogs and cats)
12-19 × 28-35
Yes
Opisthorchis species
O. viverrini = Southeast Asian liver fluke;
Uncooked freshwater fish
Fish-eating mammals (e.g., dogs and cats)
11-17 × 19-30
Yes
O. felineus = cat liver fluke
Fasciola hepatica
Sheep liver fluke
Uncooked aquatic plants
Sheep and other herbivores
63-90 × 130-150
No ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Microbiology: Parasitology
Figure 18-1 Endomyocardial biopsy, H&E stain × 1000).
Figure 18-2 Wet mount (× 40). The organism is 15 μm long and 10 μm wide. (Courtesy Dr. Mae Melvin, Centers for Disease Control and Prevention.)
Figure 18-3 Giemsa stain (× 1000).
Figure 18-4 A and B, Structures observed on microscopic examination of a stool specimen (× 400).
Figure 18-5 A, Giemsa stain, peripheral blood (× 1000). B, Classic form of this parasite.
Figure 18-6 Wet mount of stool protozoan ciliate (× 400).
Figure 18-7 Wet mount of stool pathogenic trematode. (× 480).
Figure 18-8 Modified acid-fast stain (× 1000).
Figure 18-9 Trichrome stain of fecal material (× 150).
Figure 18-10 Microscopic examination of cellulose tape preparation (× 1000).
Figure 18-11 A and B, Trichrome stain (× 100).
Figure 18-12 Rapid antigen detection results for the patient (left) and a negative control (right).
Figure 18-13 Ventral view of ectoparasite.
Figure 18-14 Giemsa-stained peripheral blood smear (× 1000).
Figure 18-15 Wet mount of stool (× 480).
Figure 18-16 Giemsa-stained peripheral blood smear (× 1000).
Figure 18-17 Wet mount of stool (× 480).
Figure 18-18 Muscle biopsy, H&E stain (× 300).
Figure 18-19 Trophozoite with flagella and undulating membrane. The trophozoite is 7 to 23 μm long and 6 to 8 μm wide. The flagella and undulating membrane are present on one side.
Figure 18-20 Microscopic examination of corneal scraping (× 1125).
