DRUG CLASSES
Direct acting
Indirect acting (anticholinesterase)
Acetylcholine (ACh) is the substance that transmits nerve impulses across the parasympathetic branch of the autonomic nervous system. There are two types of receptors in the parasympathetic nervous branch: muscarinic receptors (which stimulate smooth muscle) and nicotinic receptors (which stimulate skeletal muscle). Stimulation of this pathway results in the opposite reactions to those triggered by the adrenergic system: blood vessels dilate, sending blood to the gastrointestinal (GI) tract; secretions and peristalsis are activated and salivary glands increase production; the heart slows and pulmonary bronchioles constrict; the smooth muscle of the bladder contracts and the pupils of the eyes constrict (Fig. 26.1). Activation of these nerves is sometimes called the rest-and-digest response.
PHARMACOLOGY IN PRACTICE

Mr. Park is in the perioperative area, having just been given his preoperative medications for hip surgery. He is very concerned about the function of his bladder and bowels, because after falling in the garden he was unable to get up to urinate and needed to be straight-catheterized in the emergency room. Mr. Park is fearful that the surgery will lead to more retention issues and another infection, this time in his bladder.
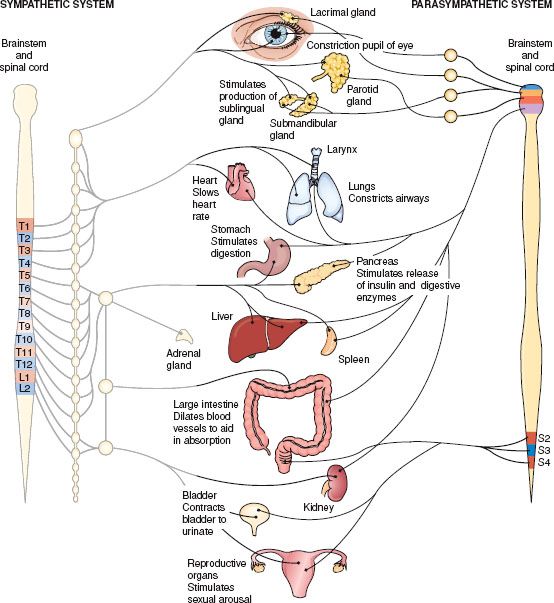
Figure 26.1 Action on body organs and structures when the parasympathetic nervous system is stimulated. (Adapted from Cohen, B. J. [2003]. Medical terminology [4th ed.]. Philadelphia: Lippincott Williams & Wilkins.)
Cholinergic drugs mimic the activity of the parasympathetic nervous system. They also are called parasympathomimetic drugs. What makes the parasympathetic system function differently is the enzyme acetylcholinesterase. Acetylcholinesterase (AChE) is an enzyme that can inactivate the neurotransmitter ACh, thereby preventing the nerve synapse from continuing the nerve impulse. This interruption in neurotransmission can diminish cognitive function, which is seen in illnesses such as Alzheimer’s disease. Drugs that inhibit the enzyme AChE are called anticholinesterases or acetylcholinesterase inhibitors. These drugs are discussed specifically in Chapter 19.
Actions
Cholinergic drugs that act like the neurotransmitter ACh are called direct-acting cholinergics. The parasympathetic branch of the autonomic nervous system partly controls the process of micturition (voiding of urine) by constricting the detrusor muscle and relaxing the bladder sphincter (see Fig. 26.1). Micturition is both a voluntary and an involuntary act. Urinary retention (not caused by a mechanical obstruction, such as a stone in the bladder) results when micturition is impaired. Treatment of urinary retention with direct-acting cholinergic drugs causes contraction of the bladder smooth muscles and passage of urine.
Myasthenia gravis is a disease that involves rapid fatigue of skeletal muscles because of the lack of ACh released at the nerve endings of parasympathetic nerves. Cholinergic drugs that prolong the activity of ACh by inhibiting the release of AChE are called indirect-acting cholinergics or anticholinesterase muscle stimulants. Drugs used to treat this disorder act indirectly to inhibit the activity of AChE and promote muscle contraction.
Treatment of glaucoma with an indirect-acting cholinergic drug produces miosis (constriction of the iris). Although used for many years, these drugs are rarely used today due to frequency of dosing and side effects experienced. See the Summary Drug Table: Cholinergic Drugs for a more complete listing of these drugs.
Uses
Major uses of the cholinergic drugs are in the treatment of the following:
• Urinary retention
• Myasthenia gravis
Adverse Reactions
Topical administration usually produces few adverse effects, but a temporary reduction of visual acuity (sharpness) and headache may occur. With the exception of those applied topically, cholinergic drugs are not selective in action. General adverse reactions include the following:
• Nausea, diarrhea, abdominal cramping
• Salivation
• Flushing of the skin
• Cardiac arrhythmias and muscle weakness
Contraindications
These drugs are contraindicated in patients with known hypersensitivity to the drugs, asthma, peptic ulcer disease, coronary artery disease, and hyperthyroidism. Bethanechol is contraindicated in those with mechanical obstruction of the GI or genitourinary tracts. Patients with secondary glaucoma, iritis, corneal abrasion, or any acute inflammatory disease of the eye should not use the ophthalmic cholinergic preparations.
Precautions
These drugs are used cautiously in patients with hypertension, epilepsy, cardiac arrhythmias, bradycardia, recent coronary occlusion, and megacolon. The safety of these drugs has not been established for use during pregnancy (pregnancy category C) or lactation, or in children.
Interactions
The following interactions may occur when a cholinergic drug is administered with another agent:
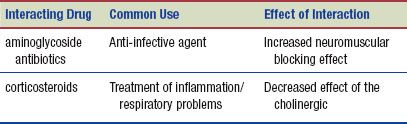
When cholinergic drugs are administered with other cholinergics, there is a synergistic effect of the drugs and greater risk for toxicity. Concurrent use of more than one anticholinergic drug antagonizes the effects of cholinergic drugs. Because of this property, atropine is considered an antidote for overdosage of cholinergic drugs.
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
The preadministration assessment depends on the drug and the reason for administration.
URINARY RETENTION. If a patient receives a cholinergic drug for the treatment of urinary retention, palpate the abdomen in the pelvic area and scan the bladder to determine if urine retention is present. A rounded swelling over the pelvis usually indicates retention and a distended bladder. The patient may also complain of discomfort in the lower abdomen. In addition, take and document the patient’s blood pressure and pulse rate.
MYASTHENIA GRAVIS. Before giving a cholinergic drug to a patient with myasthenia gravis, the primary health care provider performs a complete neurologic assessment. Assessment is made for signs of muscle weakness, such as drooling (i.e., the lack of ability to swallow), inability to chew and swallow, drooping of the eyelids, inability to perform repetitive movements (e.g., walking, combing hair, using eating utensils), difficulty breathing, and extreme fatigue.
Ongoing Assessment
While the patient is receiving a cholinergic drug, it is important to monitor for drug toxicity or cholinergic crisis.
 NURSING ALERT
NURSING ALERT
Cholinergic crisis (cholinergic drug toxicity) symptoms include severe abdominal cramping, diarrhea, excessive salivation, muscle weakness, rigidity and spasm, and clenching of the jaw. Patients exhibiting these symptoms require immediate medical treatment. In the case of drug overdose, an antidote such as atropine (0.4 to 0.6 mg intravenously [IV]) is administered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


