http://evolve.elsevier.com/McCuistion/pharmacology
The two groups of drugs that affect the parasympathetic nervous system are the cholinergic agonists—muscarinic agonists or parasympathomimetics—and the cholinergic antagonists (blocking agents)—muscarinic antagonists, parasympatholytics, or more commonly called anticholinergics. The Unit IV opener offers a discussion and comparison of the parasympathetic nervous system (parasympathomimetics and parasympatholytics) and the sympathetic nervous system.
Cholinergic Agonists
Drugs that stimulate the parasympathetic nervous system are called cholinergic agonists, or parasympathomimetics, because they mimic the parasympathetic neurotransmitter acetylcholine. The neurotransmitter located at the ganglions and the parasympathetic terminal nerve endings is acetylcholine (ACh). It innervates cholinergic receptors in organs, tissues, and glands. The two types of cholinergic receptors are muscarinic receptors, which stimulate smooth muscle and slow the heart rate, and nicotinic receptors (neuromuscular), which affect the skeletal muscles. Many cholinergic agonists are nonselective because they can affect both the muscarinic and the nicotinic receptors. However, there are selective cholinergic agonists for the muscarinic receptors that do not affect the nicotinic receptors. Fig. 16.1 illustrates the effects of parasympathetic, or cholinergic, stimulation.
There are two types of cholinergic agonists: direct-acting cholinergic agonists act on receptors to activate a tissue response (Fig. 16.2A), and indirect-acting cholinergic agonists inhibit the action of the enzyme cholinesterase (ChE), also called acetylcholinesterase (AChE), by forming a chemical complex that allows acetylcholine to persist and attach to the receptor (Fig. 16.2B). Drugs that inhibit ChE are called cholinesterase inhibitors, acetylcholinesterase inhibitors, or anticholinesterases. ChE may destroy acetylcholine before it reaches the receptor or after it has attached to the site. By inhibiting or destroying the ChE, more acetylcholine is available to stimulate the receptor and to remain in contact with it longer.
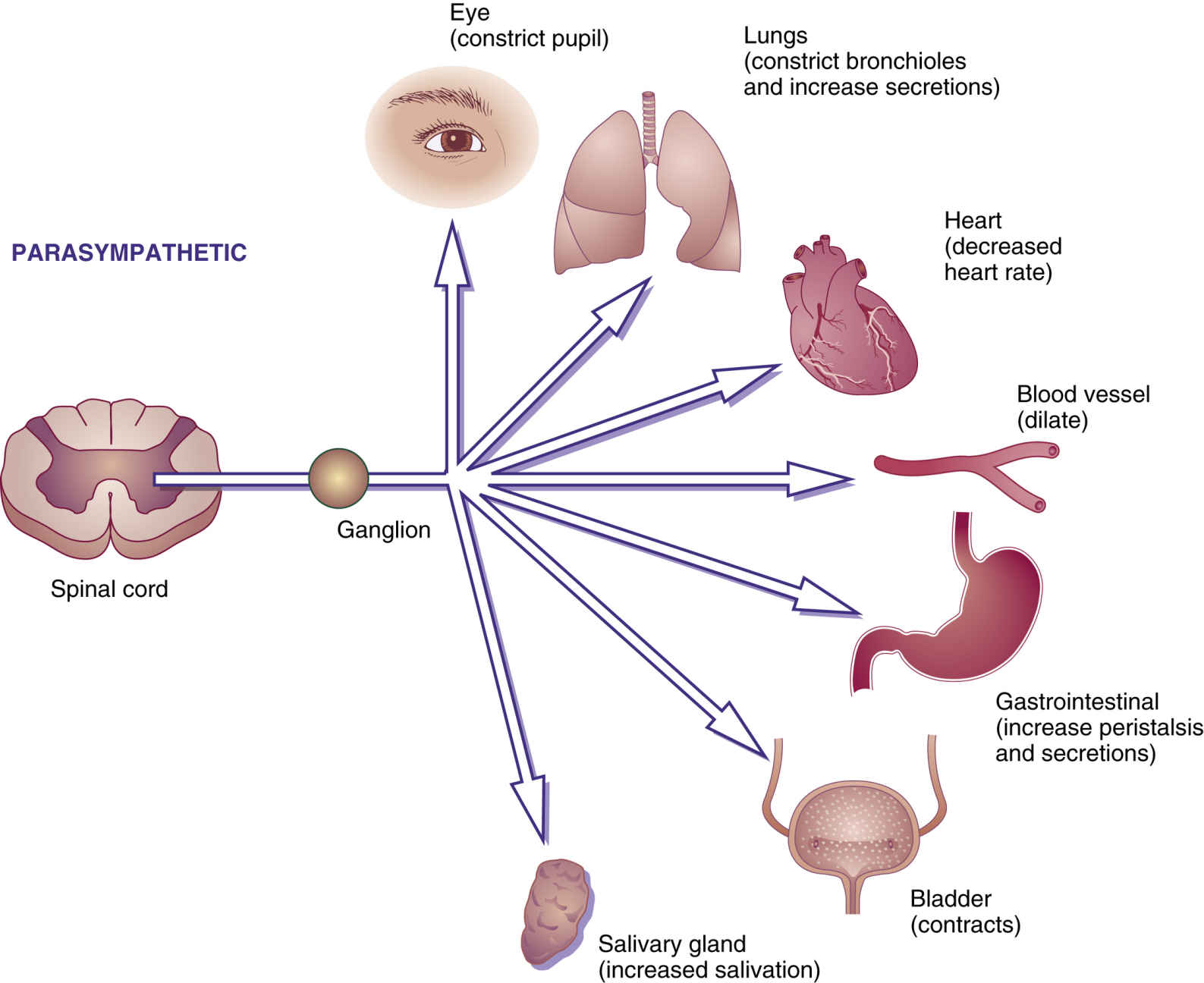
FIG. 16.1 Parasympathetic responses. Stimulation of the parasympathetic nervous system or use of parasympathomimetic drugs will cause the pupils to constrict, bronchioles to constrict and bronchial secretions to increase, heart rate to decrease, blood vessels to dilate, peristalsis and gastric secretions to increase, the bladder muscle to contract, and salivary glands to increase salivation.
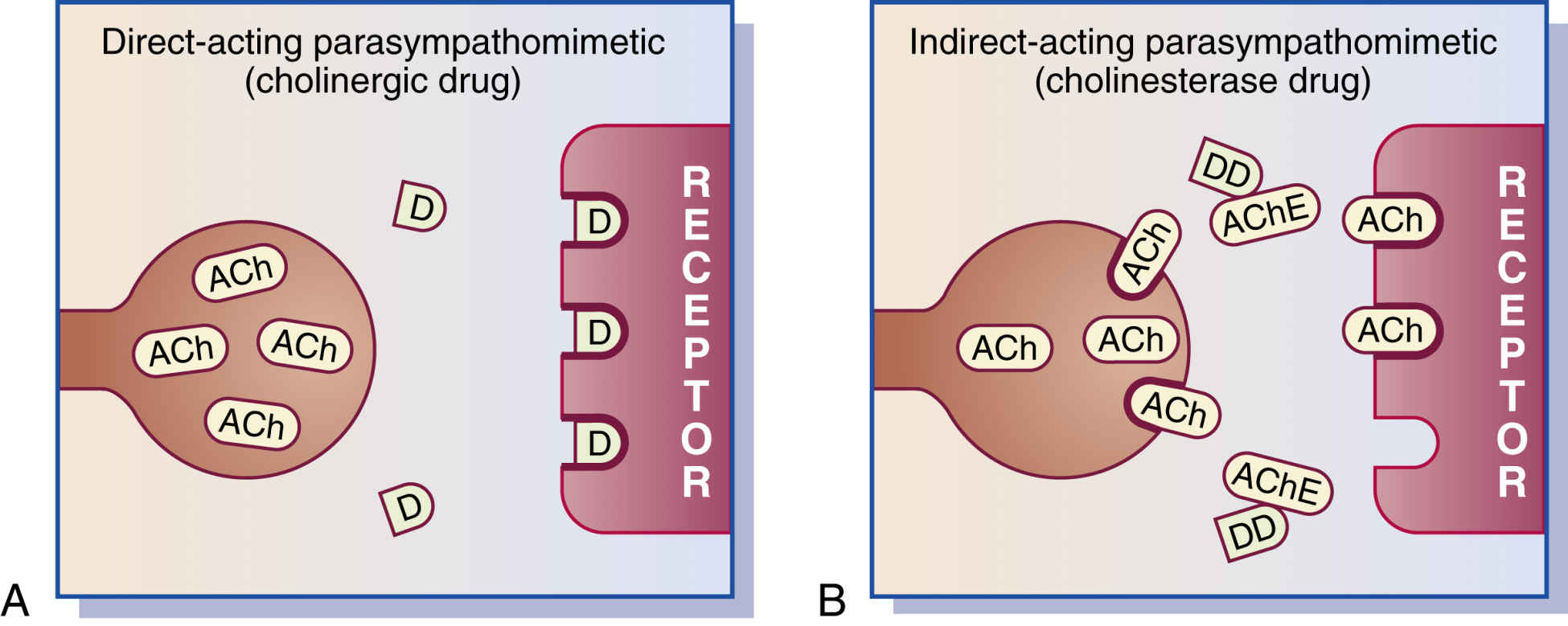
FIG. 16.2 A, Direct-acting parasympathomimetic (cholinergic agonist). Cholinergic agonists resemble acetylcholine and act directly on the receptor. B, Indirect-acting parasympathomimetic (cholinesterase inhibitor). Cholinesterase inhibitors inactivate the enzyme acetylcholinesterase (cholinesterase), thus permitting acetylcholine to react to the receptor. ACh, Acetylcholine; AChE, acetylcholinesterase or cholinesterase; D, cholinergic agonist; DD, cholinesterase inhibitor (anticholinesterase).
Cholinesterase inhibitors can be separated into reversible and irreversible inhibitors. The reversible inhibitors bind the ChE for several minutes to hours, and the irreversible inhibitors bind the enzyme permanently. The resulting effects vary with how long the ChE is bound.
The major responses of cholinergic agonists are to stimulate bladder and gastrointestinal (GI) tone, constrict the pupils of the eyes, known as miosis, and increase neuromuscular transmission. Other effects of cholinergic agonists include decreased heart rate and blood pressure and increased salivary, GI, and bronchial glandular secretions. Table 16.1 lists the functions of direct- and indirect-acting cholinergic agonists.
TABLE 16.1
Effects of Cholinergic Agonists
| Body Tissue | Response |
| Cardiovasculara | Decreased heart rate, lowered blood pressure because of vasodilation, and slowed conduction of atrioventricular node |
| Gastrointestinalb | Increased tone and motility of smooth muscle of stomach and intestine, increased peristalsis, and relaxed sphincter muscles |
| Genitourinary | Contraction of muscles of the urinary bladder, increased tone of ureters, relaxed bladder sphincter muscles, and stimulated urination |
| Ocularb | Increased pupillary constriction or miosis (pupil becomes smaller) and increased accommodation (flattening or thickening of eye lens for distant or near vision) |
| Glandulara | Increased salivation, perspiration, and tears |
| Bronchial (lung)a | Stimulation of bronchial smooth muscle contraction and increased bronchial secretions |
| Striated muscleb | Increased neuromuscular transmission and maintenance of muscle strength and tone |
Direct-Acting Cholinergic Agonists
Many drugs classified as direct-acting cholinergic agonists are primarily selective to the muscarinic receptors but are nonspecific because the muscarinic receptors are located in the smooth muscle of the GI and genitourinary tracts, glands, and heart. Bethanechol chloride, a direct-acting cholinergic agonist, acts on the muscarinic (cholinergic) receptor and is used primarily to increase urination in the treatment of urinary retention and neurogenic bladder. Metoclopramide hydrochloride (HCl) is a direct-acting cholinergic agonist that is usually prescribed to treat gastroparesis, nausea, and gastroesophageal reflux disease (GERD). In low doses, metoclopramide enhances gastric motility and thus accelerates gastric emptying time. Prototype Drug Chart 16.1 details the pharmacologic behavior of bethanechol, a classic cholinergic agonist.
Pharmacokinetics
Bethanechol chloride is poorly absorbed from the GI tract. The percentage of protein binding and the half-life are unknown. The drug is most likely excreted in the urine.
Pharmacodynamics
The principal use of bethanechol is to promote urination by stimulating the muscarinic cholinergic receptors in the detrusor muscle to contract the bladder and produce urine output. Because of the increased tone of the detrusor muscle, the onset of action is 30 to 90 minutes after taking an oral dose of bethanechol, and the duration is 2 hours. Bethanechol also increases peristalsis in the GI tract, and the drug should be taken on an empty stomach 1 to 2 hours before meals to minimize nausea and vomiting.
Side Effects and Adverse Reactions
Mild to severe side effects of most muscarinic agonists, such as bethanechol, include hypotension, tachycardia, blurred vision, excessive salivation, increased gastric acid secretion, abdominal cramps, diarrhea, bronchoconstriction, and, in some cases, cardiac dysrhythmias. This group of agents should be prescribed cautiously for patients with low blood pressure and low heart rates. Muscarinic agonists are contraindicated for patients with intestinal or urinary tract obstruction, severe bradycardia, or active asthma.
Direct-Acting Cholinergic Agonists: Eye
Pilocarpine is a direct-acting cholinergic agonist that constricts the pupils of the eyes, thus opening the Schlemm canal to promote drainage of aqueous humor (fluid). This drug is used to treat glaucoma by relieving (intraocular) fluid pressure in the eye and to promote miosis in eye surgery and examinations. Pilocarpine also acts on the nicotinic receptor, as does carbachol. Both agents are discussed in more detail in Chapter 44. An oral form of pilocarpine is used to relieve xerostomia (dry mouth).
Indirect-Acting Cholinergic Agonists
The indirect-acting cholinergic agonists do not act on receptors; instead, they inhibit or inactivate the enzyme cholinesterase, permitting acetylcholine to accumulate at the receptor sites (see Fig. 16.2B). This action gives them the name cholinesterase (ChE) inhibitors, acetylcholinesterase (AChE) inhibitors, or anticholinesterases, of which there are two types: reversible and irreversible.