9 Cardiovascular system
ANATOMY
HEART
Development of the heart
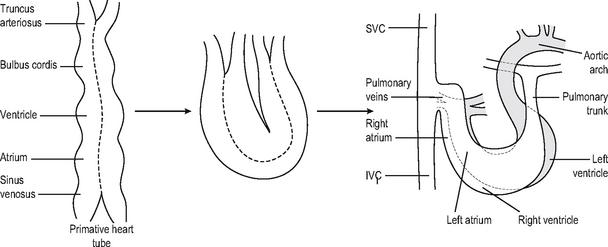
The primitive heart tube develops grooves which divide it into five regions: the sinus venosus, atrium, ventricle, bulbus cordis and truncus arteriosus (Fig. 9.1). The arterial and venous ends of the tube are surrounded by a layer of visceral pericardium. The primitive heart tube then elongates within the pericardial cavity, with the bulbus cordis and ventricle growing more rapidly than the attachments at either end, so that the heart first takes a U-shape and later an S-shape. At the same time it rotates slightly anticlockwise and twists so that the right ventricle lies anteriorly and the left atrium and ventricle posteriorly (Fig. 9.1). Despite this, and an increase in the number of vessels entering and leaving, they still continue to be enclosed together in this single tube of pericardium.
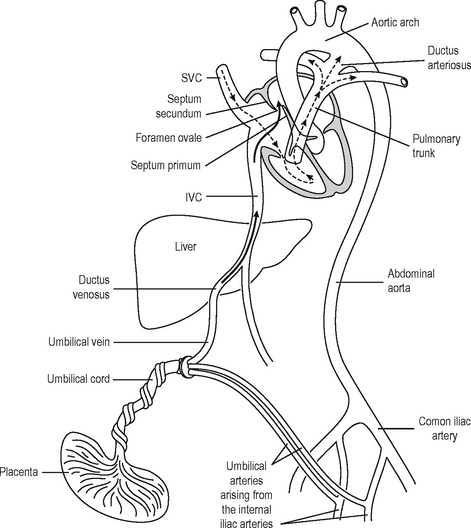
The division of the atrium is slightly more complicated. A structure called the septum primum grows down to fuse with the endocardial cushions, but leaves a hole in the upper part which is termed the foramen ovale. A second incomplete membrane develops known as the septum secundum. This is just to the right of the septum primum and foramen ovale. Thus a valve-like structure develops which allows blood to go from the right to the left side of the heart in the fetus (Fig. 9.2). At birth, when there is an increased blood flow through the lungs and a rise in the left atrial pressure, the septum primum is pushed across to close the foramen ovale. Usually the septa fuse, obliterating the foramen ovale and leaving a small residual dimple (the fossa ovalis). The sinus venosus joins the atria, becoming the two venae cavae on the right and the four pulmonary veins on the left (Fig. 9.1).
Development of the aortic arches
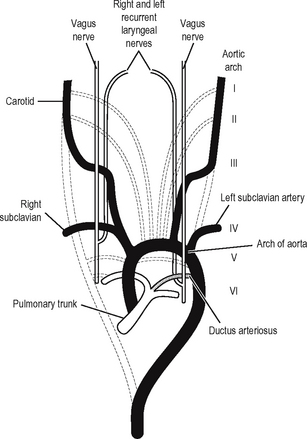
A common arterial trunk, the truncus arteriosus, continues from the bulbus cordis and gives off six pairs of aortic arches (Fig. 9.3). These curve around the pharynx to join to dorsal aortae which join together lower down as the descending aorta. These aortic arches are equivalent to those supplying the gill clefts of a fish. The first and second aortic arches disappear early, the third remains as the carotid artery, and the fourth becomes the subclavian on the right, and the arch of the aorta on the left, giving off the left subclavian. The fifth artery disappears early and the ventral part of the sixth becomes the right and left pulmonary artery, with the connection to the dorsal aortae disappearing on the right but continuing as the ductus arteriosus on the left connecting with the aortic arch.
Fetal circulation
Before birth the circulation (Fig. 9.2) obviously differs from that in the adult because oxygen and food must be obtained from maternal blood instead of from the lungs and the digestive organs. Oxygenated blood from the placenta travels along the umbilical vein, where virtually all of it bypasses the liver in the ductus venosus joining the inferior vena cava (IVC) and then travelling on to the right atrium. Most of the blood then passes straight through the foramen ovale into the left atrium so that oxygenated blood can go into the aorta. The remainder goes through the right ventricle with the returning systemic venous blood into the pulmonary trunk. In the fetus the unexpanded lungs present a high resistance to pulmonary flow, so that blood in the main pulmonary trunk would tend to pass down the low resistance ductus arteriosus into the aorta. Thus the best-oxygenated blood travels up to the brain, leaving the less well-oxygenated blood to supply the rest of the body. The blood is returned to the placenta via the umbilical arteries, which are branches of the internal iliac artery. At birth when the baby starts to breathe, there is a rise in the left atrial pressure, causing the septum primum to be pushed against the septum secundum and thus to close the foramen ovale. The blood flow through the pulmonary arteries increases and becomes poorly oxygenated, as it is now receiving the systemic venous blood.
Congenital abnormalities of the heart and great vessels
Left to right shunts (late cyanosis)
Atrial septal defect (ASD)
This may be from the ostium primum, secundum or sinus venosus and represents failure in the primary or secondary septa. Clinically important septal defects with intracardiac shunting should be differentiated from a persistent patent foramen ovale, where a probe may be passed obliquely through the septum, but flow of blood does not occur after birth, because of the higher pressure in the left atrium. This condition is said to occur in 10% of subjects, but it is not normally of any significance. Atrial septal defects requiring closure have previously been treated with a pericardial patch but more recently catheter-introduced atrial baffles made of Dacron have been used.
Anatomy of the heart
Surfaces and borders
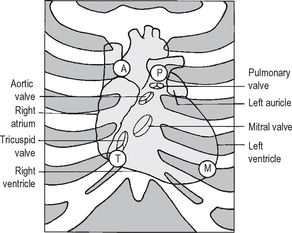
The heart (Fig. 9.4) is a muscular organ which pumps the blood around the arterial system. It consists of four chambers: right and left atria and right and left ventricles. When viewed from the front it has three surfaces and three borders. The anterior surface consists almost entirely of the right atrium and right ventricle with a narrow strip of left ventricle on the left border and the auricle of the left atrium just appearing over the top of this. It lies just behind the sternum and costal cartilages. The posterior surface consists of the left ventricle and left atrium with the four pulmonary veins entering it, and the right edge is visible. The inferior or diaphragmatic surface consists of the right atrium with the IVC entering it and the lower part of the ventricles.
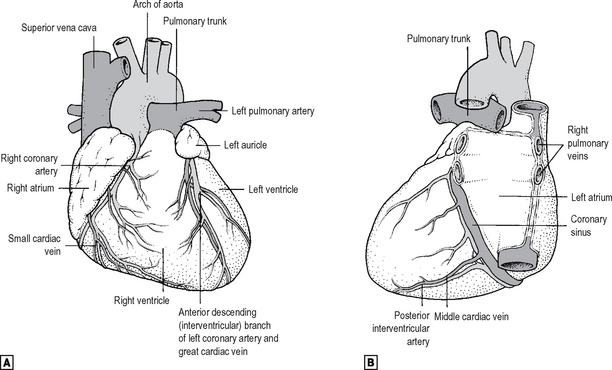
Fig. 9.4 The heart and great vessels. ![]() anterior view.
anterior view. ![]() posterior view.
posterior view.
Source: Rogers, A W Textbook of anatomy; Churchill Livingstone, Edinburgh (1992).
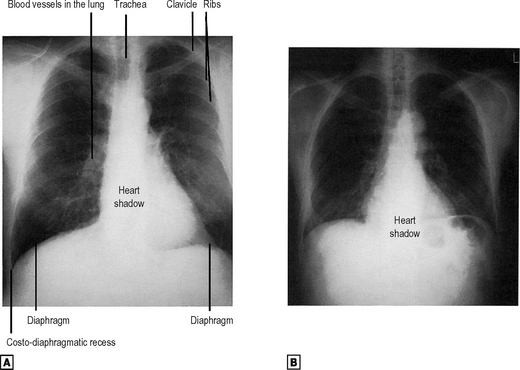
The three borders are the right, the inferior and the left. The right is made up entirely of the right atrium with the SVC and IVC. This extends from the third to the sixth right costal cartilage approximately 3 cm from the midline. The inferior border consists of the right ventricle and the apex of the left ventricle. It extends from approximately 3 cm to the right of the midline at the level of the sixth costal cartilage to the apex which is in the fifth left interspace in the mid-clavicular line (approximately 6 cm from the midline). The left border extends from the apex up to the second left interspace approximately 3 cm from the midline (Fig. 9.5). The outline of the heart can be seen clearly on a chest x-ray (Fig. 9.6). The apex of the heart is the lowest and most lateral point on the chest wall at which the cardiac impulse can be felt. As the heart is in contact with the diaphragm, it moves with each respiration. However, the anterior fibres of the diaphragm are short, so that the central tendon on which the heart rests moves relatively less.
Chambers of the heart
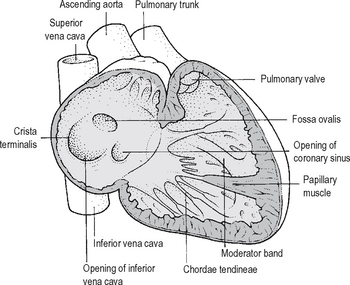
The heart (Fig. 9.7) consists of a right side which pumps blood through the lungs and the left side which pumps it through the systemic circulation. The atria collect blood from the veins and pump it into the ventricles during ventricular relaxation (diastole). When the ventricles are full they contract (systole), the valves between the atria and ventricles close, and the ventricles discharge their contained blood into the appropriate great vessel.
Right atrium
This receives blood from the SVC and IVC and from the coronary sinus. Running down between the venae cavae is a muscular ridge, the crista terminalis, which separates the smooth walled posterior part of the atrium, which is derived from the sinus venosus, from the rougher area due to the pectinate muscles derived from the true atrium. The interatrial septum has an oval depression (the fossa ovalis) which marks the site of the fetal foramen ovale (Fig. 9.7).
Right ventricle
The walls (Fig. 9.7) are much thicker than those of the atrium and there are a series of muscular thickenings, the trabeculae carnae. The tricuspid valve lies between the right atrium and right ventricle, and the three valve cusps are referred to as septal, anterior and posterior. The atrial surfaces are smooth, but the ventricular surfaces have a number of fibrous cords, the chordae tendineae, which attach them to the papillary muscles on the wall of the ventricle. These prevent the valve cusps from being everted into the atrium when the ventricle contracts.
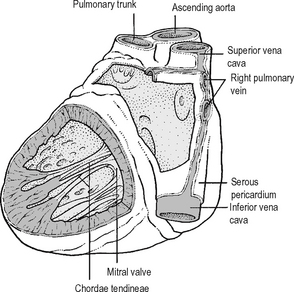
Left atrium
The left atrium (Fig. 9.8) also develops both from a combination of the fetal atrium and the sinus venosus. There are four pulmonary veins, two from each side. On the interatrial surface there is again an impression representing the site of the fetal interatrial foramen.
Left ventricle
The walls of the left ventricle (Fig. 9.8) are three times thicker than those of the right ventricle because the vascular resistance of the systemic circulation is so much greater than that of the pulmonary vasculature. The mitral valve lies between the atrium and ventricle and has two large cusps which were thought by early anatomists to look like a bishop’s mitre. Chordae tendineae run from the ventricular surfaces and margins of these cusps to papillary muscles in the ventricular wall, as with the right ventricle.
The aortic valve is similar to the pulmonary valve but stronger to cope with the higher pressure. There are three cusps – right, left and posterior – and each also has a central nodule in the free edge and a sinus or dilatation in the aortic wall alongside each cusp. The left and right coronary arteries open from the left and right valves, respectively. In about 1% of the population the aortic valve is bicuspid, and these individuals are more likely to develop calcification and stenosis in later life.
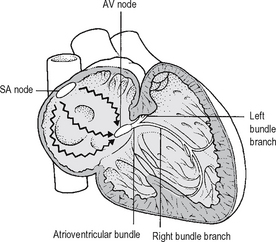
Conducting system
Although cardiac muscle is similar to skeletal muscle in many ways, it does have certain differences. Cardiac muscle cells tend to be shorter and are frequently Y-shaped and are linked at each end to other muscle cells. At the sites of attachment there is an intercalated disc which, as well as anchoring the membranes of the cells, permits the spread of electrical activity. Cardiac muscle cells are able to contract both spontaneously and rhythmically, and indeed isolated cells in culture contract regularly. As all the cells are in contact with each other and can all contract spontaneously, those with the fastest rate of contraction will drive the others. These are situated in the wall of the right atrium at the upper end of the crista terminalis (Fig. 9.9) and are termed the sinoatrial node (SA node or ‘pacemaker of the heart’). From there the cardiac impulse spreads through the atrial muscles to reach the atrioventricular node, which lines the atrial septum close to the opening of the coronary sinus. From there the atrioventricular bundle (of His) passes through a channel in the fibrous skeleton of the heart to the membranous part of the interventricular septum, where it divides into a right and left bundle branch. The left bundle is larger than the right and divides into an anterior and posterior fascicle. These run underneath the endocardium to activate all parts of the ventricular musculature in such a way that the papillary muscles contract first and then the wall and septum in rapid sequence from the apex towards the outflow track, with both ventricles contracting together. The atrioventricular bundle is normally the only pathway through which impulses can reach the ventricles.
Blood supply to the heart
The arterial supply (Fig. 9.4) is of great clinical importance, as coronary occlusion is the chief cause of mortality in the western world. The right and left coronary arteries arise from the anterior and the left aortic sinuses, respectively, just above the aortic valve, and the main branches lie in the interventricular and the atrioventricular grooves.
Right coronary artery
This passes between the pulmonary trunk and the right atrium and runs along the atrioventricular groove around the inferior border to the diaphragmatic surface. It ends by anastomosing with the terminal branch of the left coronary artery. The main branches are an artery to the SA node and adjacent atrium, the right marginal artery and the posterior interventricular which really runs inferiorly and is often called by clinicians the posterior descending artery. This branch also supplies the AV node and bundle, and parts of the right and left bundle branches.
Left coronary artery
Arising from the left aortic sinus the left coronary artery (the left main stem) varies from 4–10 mm in length and is the most important artery in the human body, in that occlusion will invariably lead to rapid demise! If stenosis of this artery is diagnosed, urgent operation is required to bypass it. It continues passing to the left behind the pulmonary trunk, reaching the atrioventricular groove. It is initially under cover of the left auricle, where it divides into two branches of equal size: the anterior interventricular (left anterior descending) and the circumflex artery. The circumflex artery continues around the left surface of the heart in the atrioventricular groove to anastomose with the terminal branches of the right coronary artery. The left anterior descending (also known as ‘the widow maker’!) runs down to the apex of the heart in the anterior interventricular groove, supplying the walls of the ventricles down the interventricular septum. It gives off the diagonal branch and goes on to anastomose with the posterior interventricular artery. However the natural anastomosis is poor and unless there has been a gradual stenosis giving time for collaterals to develop, sudden occlusion of a mild stenosis from plaque rupture (see p. 271), is almost invariably fatal, hence it’s nickname.
Venous drainage
There are three groups of veins of the heart (Fig. 9.4):
Pericardium
Fibrous pericardium
The heart and the roots of the great vessels are contained within the fibrous pericardium. It is fused with the adventitia of the great vessels. You will remember from the development of the heart that the pericardium surrounded the original primitive heart tube, which subsequently had two arteries and two veins at each end and then, as the heart enlarged, folded upon itself so that the arteries and the veins were close to each other. This still applies, and the two arteries become the aorta and the pulmonary trunk while the veins to the right atrium become the SVC and IVC and to the left the four pulmonary veins, and these latter two structures become incorporated into their respective atria. Thus, the SVC and IVC and the four pulmonary veins are all invested with the same layer of fibrous pericardium, while there is another layer investing the aorta and the pulmonary trunk, and the gap between the two becomes the transverse sinus while the blind end coming up between the four pulmonary veins and the IVC becomes the oblique sinus.
Clinical features
Cardiac surgery
Transplantation
The patient’s heart is removed, incising through the right atrium, leaving the two venae cavae, the posterior wall of the atrium and the region of the SA node intact. The posterior part of the left atrium with the four pulmonary veins is also left in situ. The incision continues through the aorta and pulmonary trunk, and the donor heart is trimmed in a similar way and anastomosed along this line described.
AORTA AND GREAT VESSELS
Branches
The left and right coronary arteries are the only branches; these have already been described on pages 230 and 231.
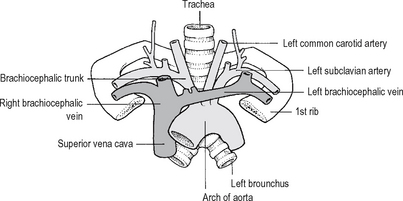
The arch of the aorta
This is a continuation of the ascending aorta and travels first superiorly and to the left, and slightly posteriorly, crossing the anterior surface of the trachea and posteriorly over the root of the left lung, and finishing just to the left of the fourth thoracic vertebra where it becomes the descending aorta (Fig. 9.10). Its apex reaches the midpoint of the manubrium sterni.
Branches
There are three major branches:
Descending thoracic aorta
This is the continuation of the arch and starts opposite the lower border of the 4th thoracic vertebra and slightly to the left of it. It ends in the midline at the lower border of the 12th thoracic vertebra, where it passes behind the median arcuate ligament of the diaphragm.
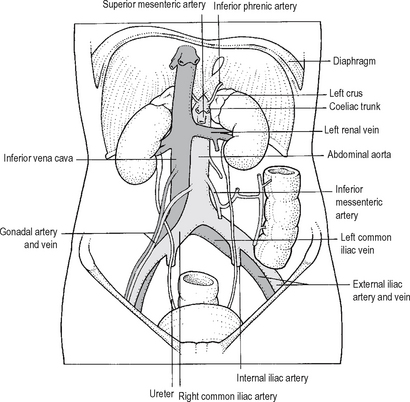
Abdominal aorta
The abdominal aorta (Fig. 9.11) commences at the aortic opening of the diaphragm at the level of the 12th thoracic vertebra, descending to the 4th lumbar vertebra where it divides into the two common iliacs. It tapers as it gives off a number of large branches.
Branches
Posterior lateral branches to the body wall
There are five-paired branches: the inferior phrenic artery and four lumbar arteries.
Midline unpaired branches to the viscera
There are three such branches, as follows:
Other great vessels of the thorax
These are systemic arteries, namely the brachiocephalic, left common carotid and left subclavian artery, and veins: right and left brachiocephalic vein and the SVC. In addition there are the pulmonary trunk, right and left pulmonary arteries and the four pulmonary veins which are the great vessels of the pulmonary circulation (see Chapter 11).
The brachiocephalic artery
This is the first and largest of the three great arteries arising from the aortic arch. It originates from the apex of the arch in the midline, travelling superiorly and posteriorly to the right, and it terminates behind the right sternoclavicular joint by dividing into the right subclavian and right common carotid artery.
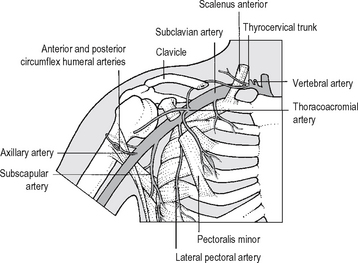
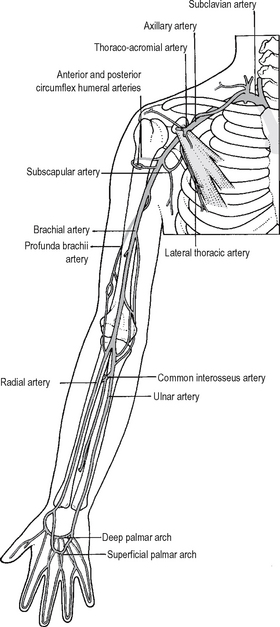
Right subclavian artery
This arises from the bifurcation of the brachiocephalic artery and courses to the outer border of the first rib where it becomes the axillary artery (Fig. 9.12). It arches laterally over the apex of the lung to reach the superior surface of the first rib, where it lies in a groove just behind the insertion of the scalenus anterior. It is divided into three parts by the scalenus anterior muscle. The first part is medial to it and gives off three branches.
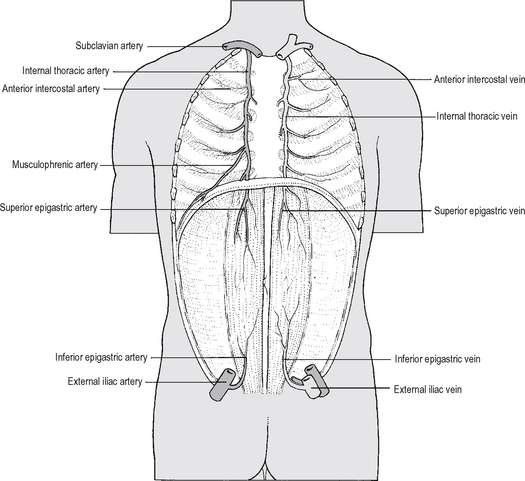
Fig. 9.13 The internal thoracic artery and vein and the anastomoses in the rectus sheath.
Source: Rogers op. cit.
The third part is lateral to the scalenus anterior and normally has no branches.
Relations
Behind the scalenus anterior muscle, the artery is closely related to the lower trunk of the brachial plexus posteriorly, and the upper and middle trunks are superior to it. The phrenic nerve runs down in front of the scalenus anterior, crossing it from lateral to medial. In surgical exploration of the subclavian artery, the scalenus anterior is divided to expose the artery, the phrenic nerve initially being retracted medially.
Left subclavian artery
This is the third and most posterior branch of the arch of the aorta. It ascends posterior and to the left of the common carotid artery to the thoracic inlet, where it arches over with similar course and relations to those of the right subclavian artery, which have previously been described. There are no branches in the thoracic part of the left subclavian.
The great systemic veins of the thorax
The SVC which carries blood into the right atrium is formed from the union of the right and left brachiocephalic veins (Fig. 9.10). These receive blood from the head and neck and upper limbs as well as from the upper half of the body wall of the trunk.
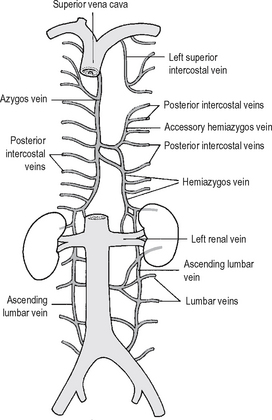
Superior vena cava
This starts behind the first right costal cartilage by the union of the two brachiocephalic veins. It passes inferiorly to enter the right atrium behind the third right costal cartilage. It is important to be aware of these landmarks when inserting a central venous pressure line since the end should lie in the SVC, and this should be checked on x-ray. The lower part of the SVC is within the fibrous pericardium. It receives one other major tributary, which is the azygos vein, into which most of the venous drainage from the thoracic and abdominal walls drains (Fig. 9.14).
BLOOD SUPPLY TO THE TRUNK
Segmental branches from the aorta
The segmental branches from the aorta which supply the body wall are:
Branches from the subclavian and axillary arteries
The internal thoracic artery has already been described and is shown in Fig. 9.13.
Branches of the external iliac artery
Venous drainage of the body wall
This consists of the following.
Azygos veins
These are three longitudinal veins lying on the bodies of the thoracic vertebrae (Fig. 9.14). There is a single azygos vein on the right, while on the left there are the hemiazygos and the accessory hemiazygos.
Vertebral venous plexus
This lies in the external surface of the vertebrae and is also known as Batson’s plexus.
Iliac veins
The external iliac veins (Fig. 9.11) run at first medially and, as they ascend and become common iliac veins, they run posterior to the iliac arteries. They join at the level of the fifth lumbar vertebra behind the right common iliac artery. Thus the left iliac vein is longer than the right. The tributaries of the internal and external iliac veins are equivalent to those of the arteries. The common iliac veins lie behind and slightly to the right of the common iliac arteries, to which they are very closely related. In aortoiliac operations, when the iliac arteries need to be clamped, great care is needed in dissecting to avoid damage to the iliac veins.
Inferior vena cava
From its origin at the level of the 5th lumbar vertebra to the right of the midline and behind the right common iliac artery, the IVC ascends vertically through the abdomen, piercing the central tendon of the diaphragm to the right of the midline to empty into the right atrium (Fig. 9.11). It is larger than the aorta, and as it ascends, is related anteriorly to the small intestine, the third part of the duodenum, the head of the pancreas with the common bile duct and then the first part of the duodenum. It lies in a deep groove in the liver before piercing the diaphragm. It receives the right and left hepatic veins from the liver. Sometimes these fuse to give one trunk going into the vena cava, but occasionally the central hepatic vein opens separately. In partial liver resections or in operations for transplantation, it is obviously important to know the precise anatomy prior to surgery. See Chapter 17.
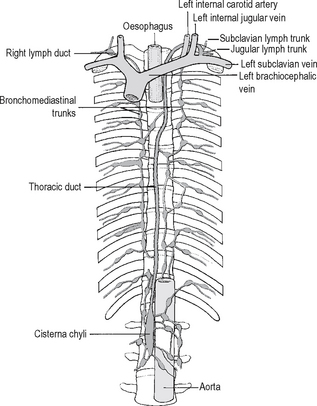
Lymphatics
The lymphatics (Fig. 9.15) from the abdomen and lower limbs drain into the cisterna chyli, which lies between the abdominal aorta and the right crus of the diaphragm. It passes through the aortic opening to become the thoracic duct, ascending behind the oesophagus. At the level of T5 it inclines to the left of the oesophagus and runs upwards behind the left carotid sheath. It then passes around and over the left subclavian artery and drains into the commencement of the brachiocephalic vein. The left jugular, subclavian and mediastinal lymph trunks, draining the head and neck, the left upper limb and the thorax, respectively, usually join the thoracic duct shortly before it enters the brachiocephalic vein, although they may open directly into it. The equivalent lymph vessels on the right join to become the right lymphatic duct which enters the origin of the right brachiocephalic vein.
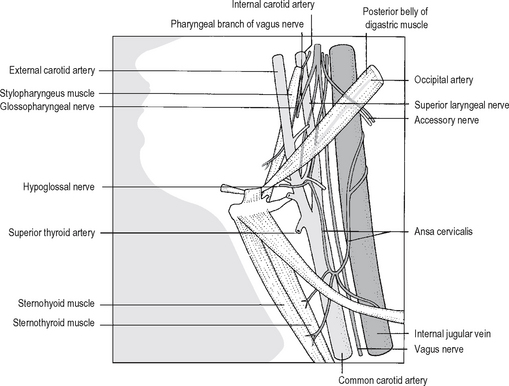
Blood supply of the head and neck
The brachiocephalic artery and the left common carotid artery in the chest have already been described (pp. 235–237). Each common carotid artery enters the neck (Fig. 9.16), from behind the sternoclavicular joint, and thereafter on both sides they have a similar course and relationships. They ascend in the carotid fascial sheath with the internal jugular vein lying laterally and the vagus nerve between and somewhat behind them. The cervical sympathetic chain ascends immediately posterior to the carotid sheath, while the sternocleidomastoid muscle is superficial to it. The carotid sheath is crossed superficially by the omohyoid muscle. At the level of the upper border of the thyroid cartilage the common carotid artery bifurcates into the internal and external carotid artery. There are no other branches of the common carotid.
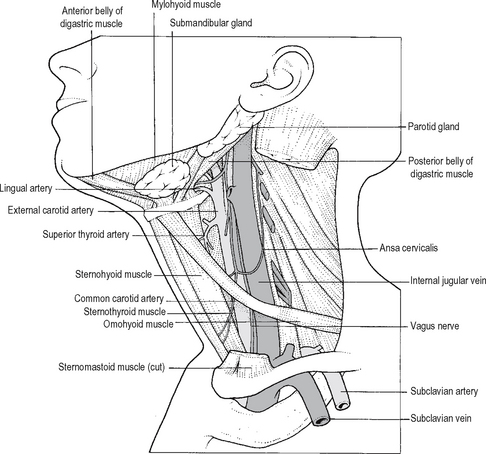
Fig. 9.16 The carotid arteries and the internal jugular vein after removal of the sternomastoid muscle.
Source: Rogers op. cit.
Internal carotid artery
This commences at the bifurcation of the common carotid artery, and at its origin is dilated into the carotid sinus which acts as a baroreceptor. In the bifurcation is the carotid body, a chemoreceptor. Both are supplied by the ninth cranial nerve. At first the internal carotid lies lateral and slightly more superficial to the external, but it rapidly passes medial and posterior to it, as it ascends to the base of the skull between the side wall of the pharynx and the internal jugular vein. The upper part of the internal carotid artery and the internal jugular vein are closely related to the last four cranial nerves (Fig. 9.17). The internal carotid is separated from the external in the upper part by the styloid process, the stylopharyngeus muscle, and the glossopharyngeal nerve and pharyngeal branch of the vagus.
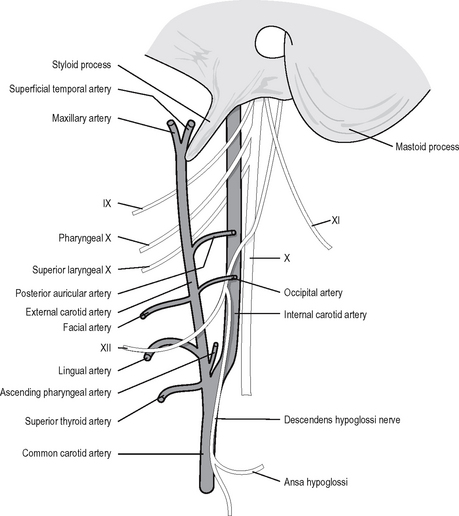
External carotid artery
The external carotid (Fig. 9.18) extends from the upper border of the thyroid cartilage to a point midway between the angle of the mandible and the mastoid process. At its origin it is anteromedial to the internal carotid but, as it ascends, it becomes more superficial. Almost immediately it gives off two branches: the ascending pharyngeal and the superior thyroid. Shortly above, it gives off the lingual artery, and then the facial and occipital artery, with the hypoglossal nerve crossing the external carotid just beneath the occipital branch. It then gives off the posterior auricular artery and terminates by dividing into the maxillary and superficial temporal artery.
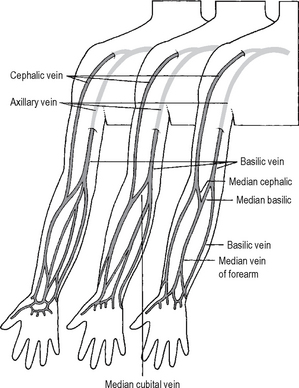
BLOOD SUPPLY OF THE UPPER LIMB (Fig. 9.19)
VENOUS DRAINAGE OF THE UPPER LIMBS (Fig. 9.20)
Superficial veins
Deep veins
The axillary lymphatics are described in Chapter 15. Suffice it to say that in block dissection of the axilla, one of the early steps is to divide the pectoralis minor muscle as high as possible. This exposes the axillary contents and in particular the axillary vein, which has to be dissected clean of lymph nodes.
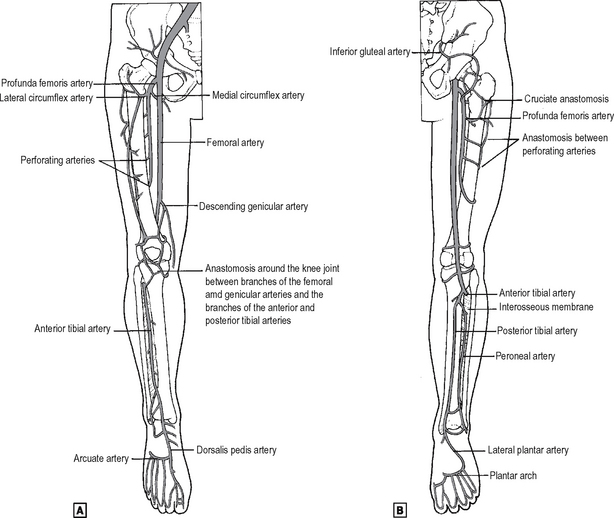
BLOOD SUPPLY OF THE LOWER LIMBS
Femoral artery
This is a continuation of the external iliac artery after it has passed deep to the inguinal ligament at its midpoint (Fig. 9.21). The upper part lies in the femoral triangle and the lower part in the adductor canal. Anatomists talk about the whole artery from the inguinal ligament to the popliteal fossa as being ‘the femoral artery’. However, vascular surgeons and radiologists describe the first inch or so as being ‘the common femoral artery’, which gives off two branches: the deep femoral or profunda femoris artery, and the superficial femoral artery which is the main artery entering the adductor canal. The main branches are shown in Fig. 9.21.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree