DRUG CLASSES
Cardiotonic
Inotropic
The cardiotonics are drugs used to increase the efficiency and improve the contraction of the heart muscle, which leads to improved blood flow to all tissues of the body. These drugs have long been used to treat heart failure, a condition in which the heart cannot pump enough blood to meet the tissue needs of the body. Although the term congestive heart failure is commonly used, a more accurate term is simply heart failure.
Heart failure is a complex clinical syndrome that can result from any number of cardiac or metabolic disorders, such as ischemic heart disease, hypertension, or hyperthyroidism. Any condition that impairs the ability of the ventricle to pump blood can lead to heart failure. In heart failure, the heart fails in its ability to pump enough blood to meet the needs of the body or can do so only with an elevated filling pressure. Heart failure causes a number of neurohormonal changes as the body tries to compensate for the increased workload of the heart. Display 38.1 discusses this neurohormonal response.
PHARMACOLOGY IN PRACTICE

Mrs. Moore’s daughter calls the clinic after her hospital discharge. She is concerned because her mother lives alone and that her mother will not be able to recognize toxicity symptoms and have to return to the hospital. Read about the drugs and their toxic effects and then think about what your approach to Mrs. Moore’s daughter would be.
Display 38.1 Neurohormonal Responses Affecting Heart Failure
The body activates the neurohormonal compensatory mechanisms, which result in:
- Increased secretion of the neurohormones by the sympathetic nervous system
- Activation of the renin-angiotensin-aldosterone (RAA) system
- Remodeling of the cardiac tissue
The sympathetic nervous system increases the secretion of the catecholamines (the neurohormones epinephrine and norepinephrine), which results in increased heart rate and vasoconstriction. The activation of the renin-angiotensin-aldosterone (RAA) system occurs because of decreased perfusion to the kidneys. As the RAA system is activated, angiotensin II and aldosterone levels increase, which increases the blood pressure, adding to the workload of the heart. These increases in neurohormonal activity cause a remodeling (restructuring) of the cardiac muscle cells, leading to hypertrophy (enlargement) of the heart, increased need for oxygen, and cardiac necrosis, which worsens the heart failure. The tissue of the heart is changed such that there is an increase in the cellular mass of cardiac tissue, the shape of the ventricle(s) is changed, and the heart’s ability to contract effectively is reduced.
Heart failure is best described by denoting the area of initial ventricular dysfunction: left-sided (left ventricular) dysfunction or right-sided (right ventricular) dysfunction. Left ventricular dysfunction leads to pulmonary symptoms, such as dyspnea and moist cough with the production of frothy, pink (blood-tinged) sputum. Right ventricular dysfunction leads to neck vein distention, peripheral edema, weight gain, and hepatic engorgement. Because both sides of the heart work together, ultimately both sides are affected in heart failure. Typically the left side of the heart is affected first, followed by right ventricular involvement. The most common symptoms associated with heart failure include the following:
• Left ventricular dysfunction
• Shortness of breath with exercise
• Dry, hacking cough or wheezing
• Orthopnea (difficulty breathing while lying flat)
• Restlessness and anxiety
• Right ventricular dysfunction
• Swollen ankles, legs, or abdomen, leading to pitting edema
• Anorexia
• Nausea
• Nocturia (the need to urinate frequently at night)
• Weakness
• Weight gain as the result of fluid retention
Other symptoms include:
• Palpitations, fatigue, or pain when performing normal activities
• Tachycardia or irregular heart rate
• Dizziness or confusion
Left ventricular dysfunction, also called left ventricular systolic dysfunction, is the most common form of heart failure and results in decreased cardiac output and decreased ejection fraction (the amount of blood that the ventricle ejects per beat in relationship to the amount of blood available to eject). Typically, the ejection fraction should be greater than 60%. With left ventricular systolic dysfunction, the ejection fraction is less than 40%, and the heart is enlarged and dilated.
In the past, the cardiotonics were the mainstay in heart failure treatment; currently, however, they are used in the treatment of patients who continue to experience symptoms after using the angiotensin-converting enzyme (ACE) inhibitors, diuretics, and beta (β) blockers. Although their use is diminished, they remain a low-cost option for therapy.
Cardiotonic drugs are used for patients with persistent symptoms or recurrent hospitalizations or as indicated in conjunction with ACE inhibitors, loop diuretics, and β blockers.
Digoxin (Lanoxin) is the most commonly used cardiotonic drug. Other terms used to identify the cardiotonics are cardiac glycosides or digitalis glycosides. The digitalis or cardiac glycosides are obtained from the leaves of the foxglove plant (Digitalis purpurea and Digitalis lanata).
Another drug with positive inotropic action is milrinone, a nonglycoside used in the short-term management of heart failure. See the Summary Drug Table: Cardiotonic and Inotropic Drugs for information concerning these drugs.
Actions
Cardiotonics increase cardiac output through positive inotropic activity (an increase in the force of the contraction). They slow the conduction velocity through the atrioventricular (AV) node in the heart and decrease the heart rate through a negative chronotropic effect. Milrinone has inotropic action and is used in the short-term management of severe heart failure that is not controlled by the digitalis preparation.
Uses
The cardiotonics are used to treat the following:
• Heart failure
• Atrial fibrillation
Atrial fibrillation is a cardiac arrhythmia characterized by rapid contractions and quivering of the atrial myocardium, resulting in an irregular and often rapid ventricular rate. See Chapter 39 for more information on arrhythmias and their treatment. These drugs do not cure heart failure; rather, they control its signs and symptoms.
Adverse Reactions
Central Nervous System Reactions
• Headache
• Weakness, drowsiness
• Visual disturbances (blurring or yellow halo)
Cardiovascular and Gastrointestinal System Reactions
• Arrhythmias
• Nausea and anorexia
Because some patients are more sensitive to side effects of digoxin, dosage is calculated carefully and adjusted as the clinical condition indicates. There is a narrow margin of safety between the full therapeutic effects and the toxic effects of cardiotonic drugs. Even normal doses of a cardiotonic drug can cause toxic drug effects. Because substantial individual variations may occur, it is important to individualize the dosage. The term digitalis toxicity (or digitalis intoxication) is used to describe toxic drug effects that occur when digoxin is administered.
Contraindications and Precautions
The cardiotonics are contraindicated in the presence of digitalis toxicity and in patients with known hypersensitivity, ventricular failure, ventricular tachycardia, cardiac tamponade, restrictive cardiomyopathy, or AV block.
The cardiotonics are given cautiously to patients with electrolyte imbalance (especially hypokalemia, hypocalcemia, and hypomagnesemia), thyroid disorders, severe carditis, heart block, myocardial infarction, severe pulmonary disease, acute glomerulonephritis, and impaired renal or hepatic function.
Digoxin is classified as a pregnancy category C drug and is used cautiously during pregnancy and lactation. Exposure to digoxin in a nursing infant is typically below an infant maintenance dose, yet caution should be exercised when digoxin is taken by a nursing woman.
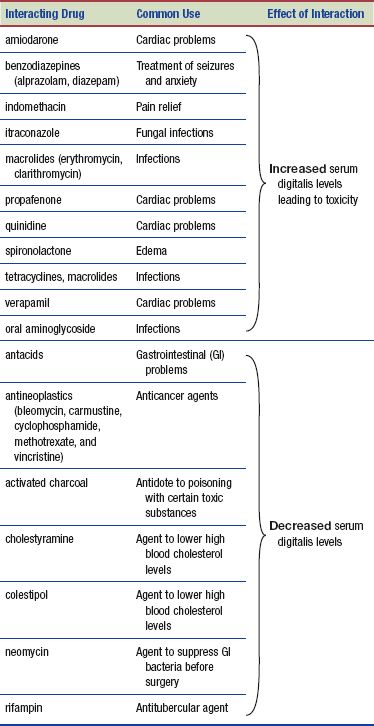
Interactions
When the cardiotonics are taken with food, absorption is slowed, but the amount absorbed is the same. However, if taken with high-fiber meals, absorption of the cardiotonics may be decreased. The following interactions may occur with the cardiac glycosides:
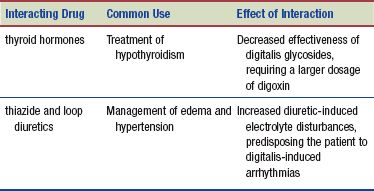
Patients may not always volunteer information regarding their use of complementary and alternative remedies. Be sure to inquire about use of herbal products. St. John’s wort (used to relieve depression) causes a decrease in serum digitalis levels. Certain drugs may increase or decrease serum digitalis levels as follows:
NURSING PROCESS
PATIENT RECEIVING AN UPPER RESPIRATORY SYSTEM DRUG
ASSESSMENT
Preadministration Assessment
The cardiotonics are potentially toxic drugs. Therefore, patients are observed closely, especially during initial therapy. The physical assessment of a person in heart failure should include information to establish a database for comparison during therapy. The physical assessment should include the following:
 Taking blood pressure, apical-radial pulse rate, respiratory rate
Taking blood pressure, apical-radial pulse rate, respiratory rate
 Auscultating the lungs, noting any unusual sounds during inspiration and expiration
Auscultating the lungs, noting any unusual sounds during inspiration and expiration
 Examining the extremities for edema
Examining the extremities for edema
 Checking the jugular veins for distention
Checking the jugular veins for distention
 Measuring weight
Measuring weight
 Inspecting sputum raised (if any) and noting the appearance (e.g., frothy, pink tinged, clear, yellow)
Inspecting sputum raised (if any) and noting the appearance (e.g., frothy, pink tinged, clear, yellow)
 Looking for evidence of other problems such as cyanosis, shortness of breath on exertion (if the patient is allowed out of bed) or when lying flat, and mental changes
Looking for evidence of other problems such as cyanosis, shortness of breath on exertion (if the patient is allowed out of bed) or when lying flat, and mental changes
The primary health care provider also may order laboratory and diagnostic tests, such as an electrocardiogram, renal and hepatic function tests, complete blood count, and serum enzyme and electrolyte levels. Renal function is particularly important because diminished renal function could affect the prescribed dosage of digoxin. Because digoxin interacts with many medications, take a careful drug history.
Ongoing Assessment
Before administering each dose of a cardiotonic, take the apical pulse rate for 60 seconds (Fig. 38.1). Document the apical pulse rate in the designated area on the chart or the medication administration record. If the pulse rate is below 60 bpm in adults or greater than 100 bpm, withhold the drug and notify the primary health care provider, unless there is a written order giving different guidelines for withholding the drug.

Figure 38.1 Nurse counts the apical pulse for 1 minute before administering the cardiotonic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


