Chapter 44 Calcium-Regulating Hormones and Other Agents Affecting Bone
| Abbreviations | |
|---|---|
| EDTA | Ethylenediamine tetraacetic acid |
| GI | Gastrointestinal |
| OPG | Osteoprotegerin |
| PTH | Parathyroid hormone |
| RANK | Receptor activator of nuclear factor-κB |
| RANKL | Receptor activator of nuclear factor-κB ligand |
| SERM | Selective estrogen receptor modulator |
Therapeutic Overview
The primary sites of regulation of Ca++ levels are the kidney, gastrointestinal (GI) tract, and bone (Fig. 44-1). The GI tract can normally absorb 10% to 20% of dietary Ca++, and effectiveness is directly dependent on vitamin D levels. Renal tubular reabsorption is highly efficient (99%) and recovers 10 to 20 gm of Ca++ filtered per day. Skeletal bone is the major site of Ca++ storage, containing approximately 1 kg in a 70-kg human. Of this, more than 99% is normally in a stable state, and 1% is in an exchangeable pool that turns over at a rate of approximately 20 g of Ca++ per day.
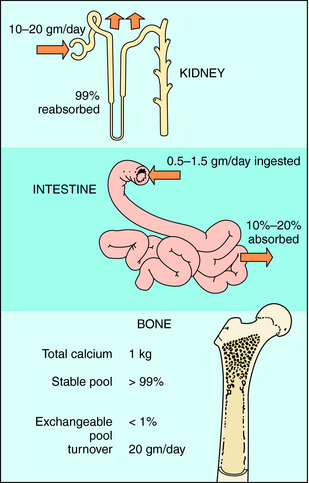
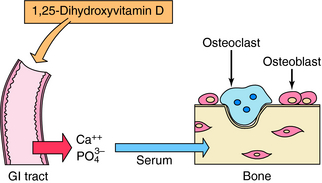
FIGURE 44–1 Sites of Ca++ regulation. Bone is the primary storage site, containing approximately 1 kg of Ca++.
associated with Ca++ or bone metabolism are dependent on the cause and severity of the disease and are summarized in the Therapeutic Overview Box (See page 501).
Hypercalcemia can result from a variety of diverse disorders including primary hyperparathyroidism, hyperparathyroidism caused by chronic renal disease, PTH-secreting parathyroid carcinoma, PTH-related protein producing-malignancy (bronchogenic carcinoma), and bone-wasting neoplasia. Management of mild hypercalcemia (10.5 to 11.4 mg/dL) usually involves dietary restriction of Ca++ and maintenance of hydration. Moderate hypercalcemia (11.5 to 14 mg/dL) has the same considerations as the mild form but requires a more aggressive and timely management plan. Specifically, it is necessary to rapidly reduce blood Ca++ levels using saline infusion and a diuretic, if renal function is intact, or dialysis, if renal function is impaired. The loop diuretics such as furosemide increase both Ca++ and Na+ excretion (see Chapter 21). Severe hypercalcemia (> 14 mg/dL) is a life-threatening condition often involving serious bone or renal pathology and requires immediate and intensive treatment. High Ca++ levels, dehydration, and volume depletion must be addressed. To rapidly reduce Ca++, intravenous administration of bisphosphonates with or without calcitonin is the safest option. Other agents and approaches have been used but are associated with frequent and severe side effects that reduce their desirability.
| Therapeutic Overview |
|---|
| Hypocalcemia |
| Disorders: |
| Hypoparathyroidism; pseudohypoparathyroidism; renal failure; inadequate calcium intake or absorption; abnormal vitamin D metabolism, ingestion, or absorption; tissue resistance |
| Management: |
| Soluble Ca++ salts and/or vitamin D or its analogs |
| Hypercalcemia |
| Disorders: |
| Hyperparathyroidism, hypervitaminosis D, neoplasia, sarcoidosis, hyperthyroidism |
| Management (based on cause and severity): |
| Mild hypercalcemia: dietary restriction of calcium |
| Moderate hypercalcemia: loop diuretics and intravenous saline |
| Severe hypercalcemia: intravenous bisphosphonates, replace phosphate as needed, calcitonin, glucocorticoids |
| Abnormal Bone Remodeling |
| Disorders: |
| Paget’s disease of bone, rickets (osteomalacia), drug-induced, osteopenia, osteoporosis |
| Management: |
| Oral/intravenous bisphosphonates, calcitonin, Ca++, vitamin D, selective estrogen receptor modulators (SERMs) teriparatide |
Mechanisms of Action
Vitamin D, Metabolites, and Analogs
The structure and metabolism of vitamin D is shown in Figure 44-2. Vitamin D is a secosteroid, a steroid in which the B ring is cleaved and the A ring rotated. Vitamin D3, cholecalciferol, is the natural form of vitamin D in humans and is synthesized from cholesterol in the skin in response to solar ultraviolet light. Vitamin D2, ergocalciferol, is the plant-derived form of vitamin D; both vitamins D2 and D3 are present in the diet and equally effective in adults. The activation of vitamin D requires enzymatic hydroxylation by the liver and the kidney. In the endoplasmic reticulum and mitochondria of the liver, vitamin D is hydroxylated to form 25-hydroxyvitamin D (calcifediol), which becomes the primary circulating metabolite. Renal metabolism of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (calcitriol) involves mitochondrial P450-catalyzed hydroxylation by the enzyme 1α-hydroxylase (CYP27B1), whose activity is stimulated by PTH and low plasma PO4 concentrations.
Calcitriol and active vitamin D analogs bind primarily to nuclear receptors in target cells and act as ligand-activated transcription factors by binding to response elements on genes and modulating synthesis of specific proteins. Among the protein products resulting from actions of vitamin D on the intestine are two high-affinity Ca++-binding proteins, the calbindins, which play a role in stimulation of intestinal Ca++ transport. Vitamin D metabolites increase absorption of dietary Ca++ and PO4−3 by stimulating uptake across the GI mucosa, leading to an increase in serum Ca++ concentration (Fig. 44-3). The antirachitic effect of vitamin D on bone mineralization is an indirect result of this increased Ca++ and PO4−3 absorption, which also results in deposition of more mineral in bone.
Vitamin D metabolites, especially at higher concentrations, stimulate the release of Ca++ from bone. The synthesis of a membrane-associated cytokine, receptor activator of nuclear factor-κB ligand (RANKL), is activated. Interaction of RANKL with receptor activator of nuclear factor-κB (RANK) receptors on osteoclasts stimulates osteoclast differentiation, survival, and activity, resulting in Ca++ release (Fig. 44-4). A decoy receptor, osteoprotegerin (OPG), is produced by bone marrow stromal cells and can competitively antagonize the effects of RANKL. Increased RANKL is a general mechanism by which many factors, including PTH, prostaglandins, and inflammatory cytokines, stimulate bone resorption. Vitamin D metabolites inhibit PTH synthesis and secretion. Vitamin D also affects differentiation of other cell types, including keratinocytes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree