Boundaries of resection for a mastectomy. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Internal Structure of the Breast
•There are 15 to 20 lobes of glandular tissue
•The lobes are interdigitated throughout the breast and drain into the lactiferous ducts and sinuses in the retroareolar area
•There is a retromammary bursa posterior to the breast tissue and anterior to the pectoralis major muscle fascia
•The subcutaneous fascia extends through the breast tissue to the skin overlying the breast and provides support to the breast (Cooper ligaments)
Polythelia and Polymastia
•The milk line extends from the axilla to the groin
•Polythelia is accessory nipples along the milk line
•Polymastia is accessory breast tissue along the milk line
•Amastia is the absence of one or both breasts
•It is differentiated from Poland syndrome by the presence of the chest wall musculature in amastia (absent in Poland syndrome)
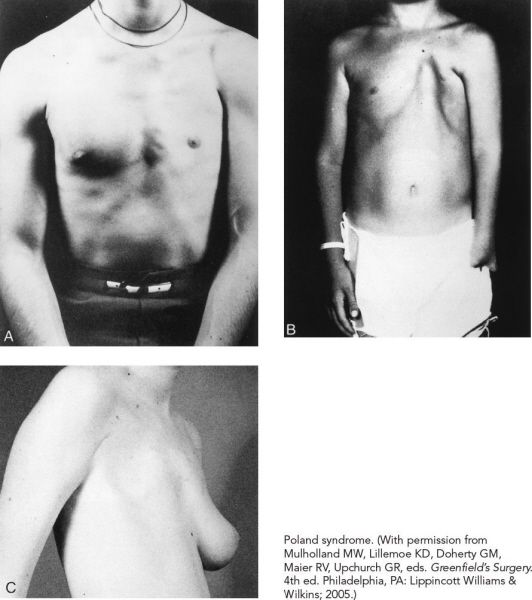
Poland syndrome. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Absence of the musculature of the shoulder girdle (pectoralis major and pectoralis minor) and malformation of the ipsilateral upper limb
•Other findings may include partial absence of the external oblique and serratus anterior, hypoplasia or complete absence of the breast or nipple, costal cartilage and rib defects, hypoplasia of subcutaneous tissues of the chest wall, and brachysyndactyly
•Usually unilateral
•Higher incidence in females than males
•The most common component is breast hypoplasia
Breast Changes in Pregnancy
•Early in pregnancy, the breast increases in volume, which is associated with breast tenderness
•The terminal ductal lobular unit undergoes extensive hyperplasia and formation of new ductules
•Occurs mostly in the first half of pregnancy
•The secretory activity of the breast is increased in the later months of pregnancy
•In the postpartum lactating female, the breast tissue is stimulated by prolactin and produces colostrum initially, followed by breast milk
A 25-year-old woman presents with a red painful area in her breast. She is 6 weeks postpartum and is breastfeeding. What is the most likely diagnosis?
Mastitis is the most likely diagnosis given the recent history of breastfeeding and the sign of a local infection (pain); however, it is important to consider a diagnosis of inflammatory breast cancer in any patient with breast redness (especially in the absence of signs or symptoms of infection).
Mastitis
•Most commonly occurs in the lactating female and results from an area of unexpressed milk that becomes secondarily infected
•Mastitis is treated with oral antibiotics and continuation of breastfeeding
•Warm compresses and breast massage can also be used to try to express the trapped milk
•Mastitis can proceed to become a breast abscess, which must be treated by drainage, either through repeated aspirations or incision and drainage
•The most common organisms of mastitis and breast abscess are Staphylococcus aureus (most common) and Streptococcus species
•If there are any systemic signs of infection, the patient should be started on antibiotics and a workup for inflammatory breast cancer should be initiated
If the diagnosis of breast abscess or mastitis is made, a full evaluation of the breast should be completed once the symptoms resolve.
A 40-year-old woman presents with severe pain in the lateral half of the breast. Physical examination reveals a painful cord. What are the most likely diagnosis and treatment?
Mondor disease is a superficial thrombophlebitis of the veins of the anterior thoracoabdominal wall (the lateral thoracic vein, the thoracoepigastric vein, or the superficial epigastric vein).

Mondor disease. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Mondor Disease
•Most common at the lower outer quadrant of the breast
•May be associated with local inflammatory states, previous surgery, trauma, or strenuous exercise
•It is NOT associated with neoplasm
•If any suspicious mass is identified on physical examination, it should be biopsied
•Treat with nonsteroidal anti-inflammatory drugs (NSAIDs)
Therapy for Mondor disease is supportive with analgesics and warm compresses. The pain and cord usually resolve within 2 to 8 weeks.
A 25-year-old female presents to the office complaining of bilateral breast pain. The pain is cyclic and is associated with her menstrual cycle. What should she do?
Cyclic mastodynia is treated with cessation of caffeine intake and smoking as well as the use of NSAIDs.
Mastodynia
•Cyclic mastodynia
•Most often benign
•Pain is associated with the menstrual cycle and most often fibrocystic disease
•Treatment is with a supportive bra, NSAIDs, decreased caffeine intake, and smoking cessation
•Continuous mastodynia
•Often represents an acute or subacute infection
•If new onset, do a bilateral mammogram if the patient is over 30 or bilateral whole breast ultrasound if the patient is under 30 to rule out cancer
What is the significance of unilateral bloody nipple discharge in a young pregnant woman in the late second trimester?
Bloody nipple discharge in a pregnant patient may be physiologic but requires an evaluation to rule out malignancy.
•Most nipple discharge is benign
•All patients with new nipple discharge should have a bilateral mammogram and ultrasound of the retroareolar area
•Bloody nipple discharge
•Most is benign and is secondary to an intraductal papilloma or papillomatosis
•10% of patients with a bloody nipple discharge have breast cancer
•Treatment: Galactogram and excision of ductal area
•Green discharge
•Usually secondary to fibrocystic disease
•If cyclic and non-spontaneous, do not need to do excision—just reassure patient
•Serous discharge
•Concerning for cancer, especially if coming from only one duct or spontaneous
•Treatment: Excisional biopsy of ductal area
•Spontaneous discharge
•No matter what color or consistency, spontaneous discharge is worrisome for cancer
•All patients need a biopsy
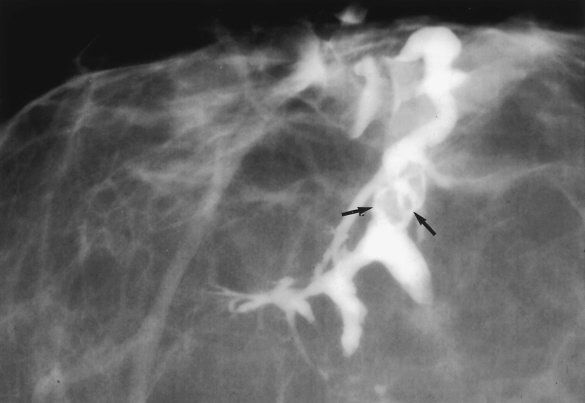
Ductogram demonstrating an intraductal papilloma. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
If the workup of bloody discharge is negative and the discharge persists, the ductal system should be excised to rule out malignancy.
A 36-year-old woman presents with a complaint of a new breast mass. What should the initial workup include?
Imaging studies include ultrasound and mammogram (with shielding if pregnant) and a physical examination. If the abnormality is suspicious by imaging or physical examination, a core needle biopsy should be performed.
•A history, physical exam, and ultrasound are appropriate first steps
•A mammogram can be performed in a young woman if the breasts are not markedly dense
•If a simple cyst is suspected, a cyst aspiration can be performed in the office
•If the mass resolves completely after the aspiration and the fluid is not bloody, the area can safely be followed with serial physical exams
•If an ultrasound documents a simple cyst, it can safely be followed clinically
•Solid lesions can be followed with imaging and physical examination if they are small and have classic characteristics of benign lesions
•All complex cysts or solid lesions that are not classically benign should undergo a core needle biopsy if possible
•If a core needle biopsy is not possible, an excisional biopsy should be performed
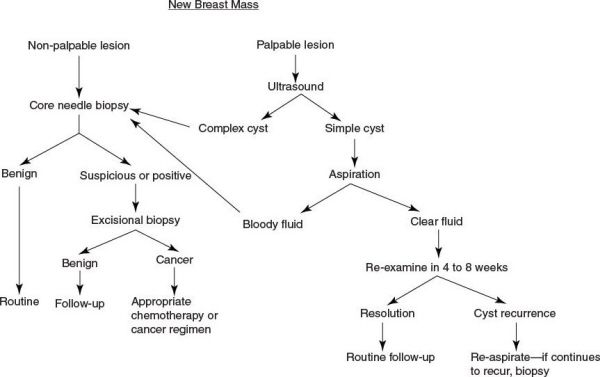
(With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
An ultrasound should be performed for evaluation of all palpable breast lesions.
A 24-year-old female presents with a firm, mobile mass in her left breast. What is the most likely diagnosis?
A benign fibroadenoma.
Fibroadenoma
•Benign mass made of stromal and glandular elements
•Most common breast lesion in women <30 years
•May have single or multiple and can be bilateral (10%)
•Often have pain in these lesions with the menstrual cycle
•Can enlarge during pregnancy
•Should have workup above
Fibrocystic Disease
•Benign disease associated with proliferation of fibrous tissue  cysts and nodularity of breasts
cysts and nodularity of breasts
•Most common breast lesion overall
•Most commonly found in women aged 30 to 50 years
•Have firm, mobile breast masses that become tender during the menstrual cycle
•Treatment
•Control pain by minimizing caffeine intake
•Symptoms improve post-menopause
A 48-year-old woman presents with a new palpable breast mass. Her mammogram and ultrasound are normal. What is the most appropriate next step?
If the mass is clinically suspicious, a core needle biopsy should be performed. Mammogram and ultrasound can miss up to 20% of all breast cancers.
Mammography
•Mammograms have a 50% false-positive rate over 10 years
•Only about 20% of biopsies performed because of an abnormal mammogram have significant pathology
•Magnification views can be used to help define microcalcifications
•If a density is seen on mammography, compression views can be used to help differentiate the nature of the abnormality
If the density effaces on compression then it is probably benign.
Ultrasound Findings Suspicious for Malignancy
•Irregular shape
•Rough uneven border
•Heterogeneous internal echoes
•Posterior shadowing indicating that the lesion is solid and not cystic
•No lateral shadows or hyperechoic border
•Masses that are taller than they are wide
•Disrupted fascial planes
Mammographic Findings Suspicious for Malignancy
•Asymmetric density
•Any new mass
•Microcalcifications
•Clustered
•Stellate pattern
•Pleomorphic
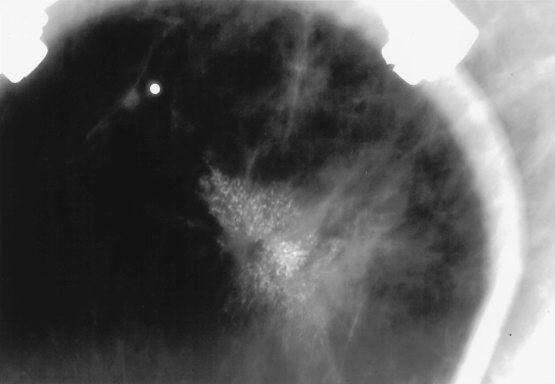
Mammogram with clustered microcalcifications. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
All new breast masses in postmenopausal women should have a histologic (tissue) diagnosis.
A 63-year-old woman is noted to have a mammographic abnormality upon routine screening. What is the next step in management?
•Compare the mammogram to previous mammograms.
•Perform magnification and spot compression views.
•Perform an ultrasound evaluation of the area if there is a density present on mammogram.
Follow-Up of an Abnormal Mammogram
•All mammograms are interpreted using the Breast Imaging Reporting and Data System
•BIRADS 0: Needs additional imaging
•BIRADS 1: Completely normal mammogram
•BIRADS 2: Abnormality that is benign (e.g., simple cyst, duct ectasia, and benign calcifications)
•BIRADS 3: Abnormality that is probably benign (e.g., unchanged calcifications and density that resolves with compression)
•BIRADS 4: Abnormality that is possibly malignant (e.g., new calcifications and new density that persists with compression)
•BIRADS 5: Abnormality that is probably malignant (e.g., new highly suspicious calcifications and new highly suspicious density)
•BIRADS 6: Known malignancy present
BIRADS 1 and 2 mammographic lesions are followed with yearly screening.
BIRADS 3 mammographic lesions should have repeat imaging in 6 months.
BIRADS 4 and 5 mammographic lesions should be biopsied.
A 53-year-old woman presents for evaluation following a mammogram, which was significant for a small cluster of microcalcifications in her left breast. She does not have any masses on physical exam. What is the next step in management?
When available, a stereotactic core needle biopsy is minimally invasive and can sometimes provide a diagnosis; it is often preferable to a needle-guided excisional biopsy as an initial step in management.
Biopsy Approaches for Evaluating Breast Abnormalities
•Stereotactic core needle biopsy is most utilized for microcalcifications
•This technique uses mammographic guidance to perform a core needle biopsy
•Ultrasound-guided core needle biopsy is used when the lesion is visible on ultrasound
•Palpation-directed core needle biopsy can be performed for palpable lesions
•A fine needle aspiration (FNA) is adequate for simple cyst aspiration and biopsy of a suspicious axillary node, but not much else
•For suspicious lesions, a core needle biopsy can provide enough tissue to differentiate between an in situ vs. invasive tumor and for tumor markers such as estrogen and progesterone receptors and Her-2-neu
•When possible, core needle biopsy is preferable to excisional biopsy to reach a diagnosis
•This results in a reduced positive margin rate and allows for axillary staging, which reduces the total number of surgeries required for management
•When a core needle biopsy is not possible, an excisional biopsy can be performed, either with wire localization, image guidance, or palpation directed
•An incisional biopsy has very limited indications in the management of breast tumors
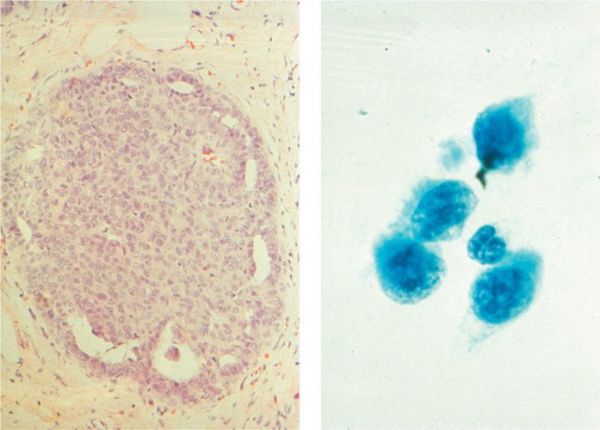
Comparison of (A) core needle and (B) FNA biopsy specimens. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
If inflammatory breast cancer or Paget disease is suspected, a punch biopsy of the suspicious skin should be performed.
A 38-year-old woman with a breast mass has a core needle biopsy of a mammographic abnormality demonstrating a radial scar. What is the next step in management?
A radial scar is one of the histologic findings that should be followed with an excisional biopsy.
Histologic Findings on Core Needle Biopsy That Require Excisional Biopsy
•Radial scar
•Atypical hyperplasia
•Lobular carcinoma in situ (LCIS)
•Discordant biopsy (i.e., the pathologic findings are not consistent with the imaging studies or physical examination findings)
•Papillary lesion
An excisional biopsy is a term sometimes used interchangeably with lumpectomy, partial mastectomy, and breast preservation. In the context of nearly all breast cancers, these procedures should have adequate clear margins (usually 1 to 2 cm), a sentinel node biopsy (unless nodes are palpable), and be coupled with postoperative radiation.
Histologic Findings on Core Needle Biopsy That Do Not Require Excisional Biopsy
•No increased risk of breast cancer
•Duct ectasia
•Fibrocystic breast disease
•Apocrine metaplasia
•Cysts
•Fibroadenoma
•Fibrosis
•Usual duct hyperplasia
•Mastitis
•Periductal mastitis
•Squamous metaplasia
•Slightly increased risk (1.5 to 2.0 times normal)
•Florid epithelial hyperplasia
•Sclerosing adenosis
Histologic Characteristics of Breast Cancer
•Monomorphic pattern
•Nuclear crowding with a variation in nuclear size
•Chromatin clumping
•Prominent nucleoli
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


