Basal-like Carcinomas
Key Facts
Terminology
Triple negative breast cancer (TNBC)
Basal-like carcinoma (BLC)
Lack of hormone receptor expression
Low expression of HER2
High expression of basal cytokeratins 5, 14, & 17
High expression of proliferation-related genes
TNBC increasingly used as surrogate for BLC
Most but not all BLCs fall into the TNBC category
Clinical Issues
Approximately 15% of infiltrating carcinomas of the breast
BRCA1-associated cancers are usually BLC
More frequent in premenopausal African-American women
Most BLCs demonstrate an aggressive clinical course
Increased risk for early relapse/recurrence
Increased risk for visceral organs & CNS recurrence
No role for endocrine- or HER2-targeted therapies
Most patients receive aggressive multiagent chemotherapy
Tumors may be hypersensitive to DNA-damaging agents
Microscopic Pathology
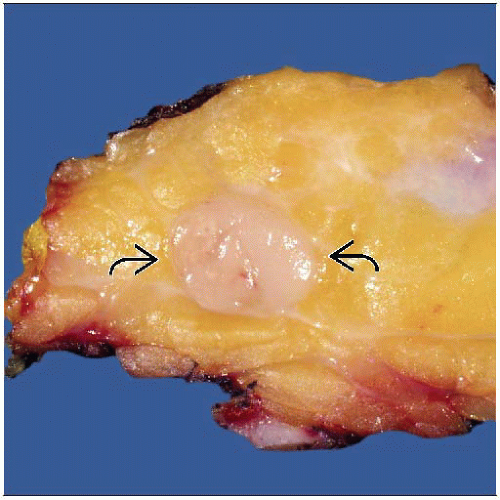
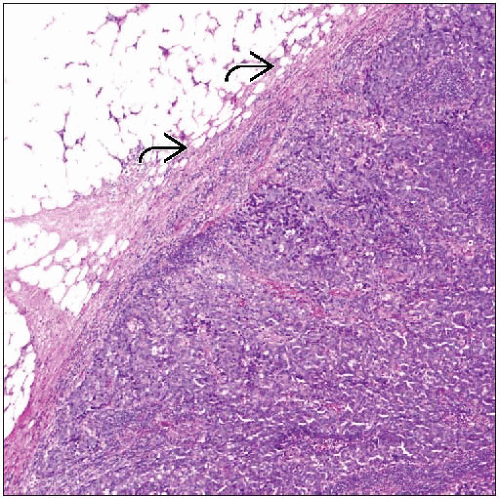
BLC has distinctive morphologic features
Circumscription with pushing borders
Pleomorphic tumor cells, syncytial-like growth
High nuclear grade
Areas of geographic necrosis
Brisk lymphocytic stromal reaction
TERMINOLOGY
Abbreviations
Basal-like carcinoma (BLC)
Triple negative breast cancer (TNBC)
Definitions
BLC is a type of invasive breast cancer originally defined by gene expression profiling studies
ETIOLOGY/PATHOGENESIS
Gene Expression Profiling
4 major types of carcinoma are identified by their patterns of gene expression
Luminal A (˜ 55%), luminal B (˜ 15%), HER2 (˜ 15%), and BLC (˜ 15%)
BLC and myoepithelial cells share expression of similar groups of genes
Term “basal” was chosen to include myoepithelial cells as well as possible precursor or progenitor cells
Actual cell of origin is unknown
Gene expression patterns characteristic of BLC include
Lack of hormone receptor expression (or only very rare expression)
Low or absent expression of HER2
High expression of basal cytokeratins 5, 14, and 17 (specific for BLC)
Cytokeratin 5/6 present in majority in most studies; however, in 1 study, only 6% of BLCs were positive, suggesting there may be variability in antibodies
Cytokeratin 17 present in 50% but may be focal and weak
Most also express luminal cytokeratins 7, 8/18, and 19
High expression of proliferation-related genes
High expression of EGFR (HER1)
45-75% positive
Less common in non-BLC
Expression of other proteins: C-Kit (CD117), VEGF, cyclin-E, fascin, α B-crystallin
p53 overexpression present in 50-60%
Mutations of TP53 are more common compared to all breast cancers
CD117 (C-Kit): Majority of positive cancers are BLC
Positive in ˜ 45% of BLC
Does not correlate with mutations indicative of sensitivity to tyrosine kinase inhibitors
Not all cancers with increased mRNA levels have increased protein expression
BRCA1, BLC, and Hereditary Breast Cancer
Majority of breast cancers occurring in BRCA1 mutation carriers are in BLC group
BRCA1 has many functions
DNA repair of double-strand breaks by homologous recombination: Cells that lack BRCA1 must rely on other less reliable modes of repair and are genetically unstable
Cell cycle regulation, checkpoint control
Transcriptional control, ubiquitination, chromatin remodeling, and regulation of apoptosis
Required for transactivation of the ER gene promoter: Loss may result in ER negativity
Genetic instability results in replication errors
Result in accumulation of chromosomal abnormalities
Enables mutations in genes essential to cell cycle checkpoint activation
Accumulating mutations predispose to tumor formation
BRCA1 defects are postulated to be initiating oncogenic events in hereditary and sporadic BLC
Mammary stem cells demonstrate a basal-like gene expression profile
Many sporadic BLCs also have altered BRCA1 activity and loss of function
CLINICAL ISSUES
Epidemiology
Incidence
10-15% of invasive breast carcinomas
Age
More common in younger patient population
Range: 47-55 years
Patients more likely to be premenopausal
Treatment
Adjuvant therapy
No role for endocrine- or HER2-targeted therapy due to lack of expression of hormone receptors and HER2
Most patients treated with aggressive multiagent chemotherapy
Hypersensitivity to DNA-damaging agents due to abnormal DNA repair function
Anthracyclines and platinum agents
BLC may show resistance to mitotic spindle poisons (taxanes)
BLC often shows response after neoadjuvant chemotherapy
About 15% demonstrate pathologic complete response
Some of these patients may be cured
Patients without pathologic complete response to neoadjuvant chemotherapy have poor prognosis
Prognosis
Most BLCs demonstrate aggressive clinical course and poor prognosis
Decreased disease-free interval, disease-specific survival, and overall survival compared with other breast cancers
Increased risk for early relapse/recurrence
Increased risk for visceral organs & CNS recurrence
However, some carcinomas within this group have exceptionally good prognosis
Adenoid cystic carcinoma, secretory carcinoma, low-grade adenosquamous carcinoma, and (to some extent) medullary carcinoma
In these cancers, histologic classification is more important than expression profiling classification
Other special histologic types of BLC share same poor prognosis
Metaplastic carcinoma, spindle cell carcinoma
Poor prognosis may be due to overexpression of genes promoting proliferation and migration
EGFR activates signaling pathways involved in cell proliferation
α B-crystallin, a heat shock protein, inhibits apoptosis
Fascin, a cell motility protein, promotes tumor cell invasion
VEGF promotes angiogenesis
BLC has specific pattern of metastases
Higher incidence of metastasis to brain (central nervous system) and lung
Metastases to these sites have poorer prognosis
Less likely to metastasize to bones or lymph nodes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree