Chapter 49 Antimycobacterial Agents
| Abbreviations | |
|---|---|
| AIDS | Acquired immunodeficiency syndrome |
| CNS | Central nervous system |
| CSF | Cerebral spinal fluid |
| DNA | Deoxyribonucleic acid |
| DOT | Directly observed therapy |
| GI | Gastrointestinal |
| HIV | Human immunodeficiency virus |
| IM | Intramuscular |
| INH | Isoniazid (isonicotinic acid hydrazide) |
| IV | Intravenous |
| LTBI | Latent TB infection |
| MAC | Mycobacterium avium complex |
| MDR | Multi-drug resistance |
| PAS | p-Aminosalicylic acid |
| POA | Pyrazinoic acid |
| PZA | Pyrazinamide |
| PZase | Nicotinamidase/pyrazinamidase |
| RNA | Ribonucleic acid |
| TB | Tuberculosis |
| WHO | World Health Organization |
| XDR-TB | Extensive drug-resistant TB |
Therapeutic Overview
countries. Overall, it is estimated that one third of the people in the world are currently infected with the TB bacillus. In the United States there was a resurgence of TB between 1985 and 1992, largely because of underfunding and decline of the public health infrastructure. With increased attention and funding, since 1992 there has been a decline in the number of TB cases in the United States to 14,097 TB cases in 2005 (4.8 per 100,000 population). The global epidemic of TB has impacted the United States, where most cases now occur among foreign-born persons. There are great racial/ethnic disparities among case rates. For individuals born in the United States, in 2005, the rate among African-Americans was almost eight times that of Caucasians.
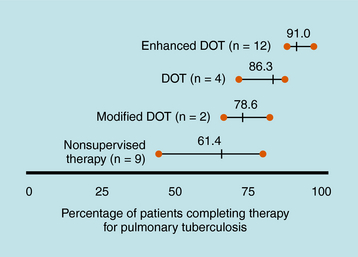
Treatment of TB is much different than treatment of other diseases because of its public health implications. The provider has the responsibility for prescribing an appropriate regimen and ensuring that treatment is completed. Directly observed therapy (DOT) is recommended for all patients with active TB disease and can help ensure higher completion rates (Fig. 49-1), decrease risk for emergence of resistance, and enhance TB control. DOT is generally provided by public health agencies. Active TB should never be treated with a single drug because of the risk of emergence of resistance; therefore multidrug therapy is required. The minimum length of therapy is 6 to 9 months. Patients with drug resistance, especially multidrug resistance (MDR) (i.e., resistance to at least isoniazid and rifampin) require longer therapy. MDR-TB is associated with much higher morbidity and mortality. Drug resistance is an important factor in determining the appropriate therapeutic regimen. Patients who are infected with M. tuberculosis (latent TB infection, or LTBI) are at risk for progressing to active disease. This can be greatly reduced by treating persons with LTBI who are at high or increased risk for progression to active disease (e.g., HIV infection, other illnesses that increase risk of progression, recent infection, or recent immigration from high TB endemic area).
| Therapeutic Overview |
|---|
| Tuberculosis |
| Tuberculosis is a huge global health problem; the second leading cause of death due to an infectious disease worldwide. |
| More than 8 million new cases and 1.5 million deaths occur annually. |
| M. tuberculosis is an aerobic organism. |
| M. tuberculosis can cause latent infection and active pulmonary or extrapulmonary disease. |
| Combinations of drugs are used for active disease; a single drug can be used for latent infection. |
| Long-term treatment is needed (at least 6-9 months). |
| Bacterial resistance is of growing importance. |
| Multidrug-resistant tuberculosis is associated with increased morbidity and mortality. |
| Directly observed therapy is an important component in treatment. |
| Leprosy (Hansen’s disease) |
| Leprosy is caused by M. leprae, an aerobic acid-fast bacillus organism. |
| M. leprae grows extremely slowly with a long incubation period (average 2-4 years). |
| It is a chronic disease; clinical manifestations depend upon immune responses. |
| Long-term treatment is needed, usually with multidrug therapy. |
| Leprosy “reactions” can result from immunologically mediated acute inflammatory responses. |
| Mycobacterium avium complex (MAC) disease |
| Disseminated MAC most commonly occurs in patients with advanced HIV/AIDS. |
| Pulmonary infections are also seen in HIV-seronegative individuals, particularly with underlying or chronic pulmonary disease. |
| Treatment requires a multidrug regimen for prolonged periods. |
| Prophylaxis is indicated in patients with advanced HIV infection. |
Mechanisms of Action
Inhibition of Protein Synthesis
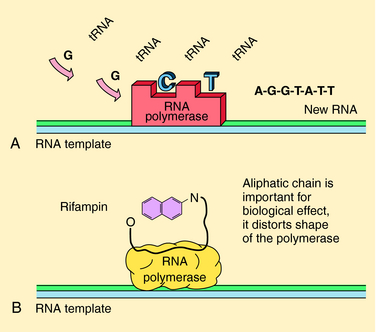
The rifamycins (rifampin, rifabutin, rifapentine) are bactericidal and inhibit deoxyribonucleic acid (DNA)-dependent ribonucleic acid (RNA) polymerase of mycobacteria (but not mammals). This enzyme is composed of four subunits; rifamycins bind to the β-subunit, which results in blocking the growing RNA chain (Fig. 49-2). Resistance is conferred by single mutations that tend to occur (>95%) in an 81-base pair region of the rpoB gene that codes for the β-subunit. The aminoglycosides streptomycin, kanamycin, and amikacin act by inhibiting protein synthesis and are described in Chapter 47. Capreomycin, a macrocyclic polypeptide antibiotic, has similar activity and toxicities as aminoglycosides.
Inhibition of Cell Wall Synthesis: Isoniazid (INH)
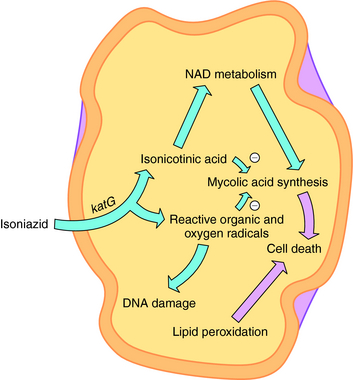
INH is a bactericidal agent that is thought to inhibit mycolic acid synthesis. Mycolic acids are a major constituent of mycobacterial cell walls (along with arabinogalactan and peptidoglycan). The mode of action of INH is complex, and a current model is shown in Figure 49-3. INH is a prodrug that has to be activated by the M. tuberculosis catalase-peroxidase enzyme encoded by the katG gene. Deletions or mutations in this gene may account for 40% to 50% of clinical INH-resistant isolates. Other mechanisms of resistance may include mutations in three other genes. inhA and kasA code for mycolic acid biosynthetic enzymes, and mutations are found in some INH-resistant isolates. ahpC has also been associated with some INH resistance strains, but its role is unclear.
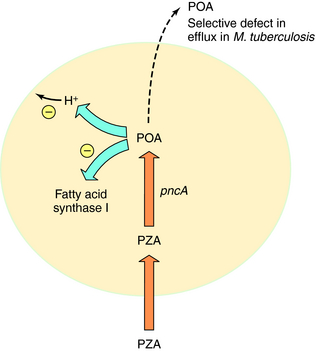
Pyrazinamide (PZA) is active only against M. tuberculosis and M. africanum; it is inactive against M. bovis and nontuberculous mycobacteria. PZA is active at a low pH (e.g., pH 5), is bactericidal, and has excellent sterilizing activity against semidormant bacteria. PZA is thought to enter M. tuberculosis by passive diffusion and is then converted to the active metabolite pyrazinoic acid (POA) by nicotinamidase/pyrazinamidase (PZase). The target of POA may involve fatty acid synthase I and disruption of mycobacterial membranes by acid (Fig. 49-4). Selected mutations in the PZase gene (pncA) are associated with PZA resistance in M. tuberculosis.
Drugs for treatment of leprosy include rifampin, dapsone, clofazimine, ofloxacin, and minocycline. Rifampin is highly bactericidal against M. leprae and is discussed in the previous text. Its mechanism of action is presumed to be inhibition of M. leprae DNA-dependent RNA polymerase. Similar to sulfonamides, dapsone acts as an inhibitor of dihydropteroate synthetase in folate synthesis to produce a bacteriostatic effect. Clofazimine is active against M. leprae (weakly bactericidal), but its mechanism of action is unknown. Ofloxacin, a fluoroquinolone, is discussed in Chapter 48, and the tetracycline minocycline is discussed in Chapter 47.
Anti-M. avium Complex (MAC) Drugs
Clarithromycin and azithromycin have excellent activity against MAC, and these macrolides are the cornerstone of therapy. They can be used in both prevention and treatment of disease (see Chapter 47). Ethambutol is usually combined with clarithromycin (or azithromycin) for treatment of MAC infections, especially among HIV-infected patients with disseminated MAC. Rifabutin can also be used to prevent MAC in HIV-infected patients who are unable to take macrolide drugs, and it can also be used in combination with other agents. Amikacin and the fluoroquinolones also have activity against MAC and are discussed in Chapters 47 and 48, respectively.
Pharmacokinetics
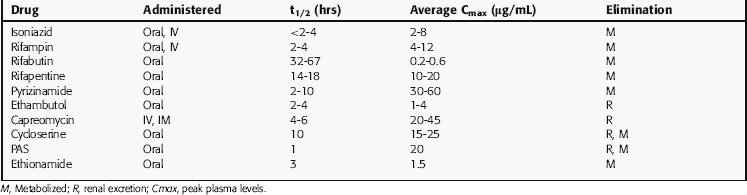
Key pharmacokinetic parameters are summarized in Table 49-1 and in Chapters 47 and 48.
INH is well absorbed orally and is widely distributed, with peak concentrations achieved in pleural, peritoneal, and synovial fluids. Cerebrospinal fluid (CSF) concentrations are approximately 20% of plasma levels but can increase to 100% with meningeal inflammation. INH is metabolized by a liver N-acetyltransferase, and the rate of acetylation determines its concentration in plasma and its half-life. As discussed in Chapter 2, slow acetylation is inherited as an autosomal recessive trait. The average plasma concentration of drug in rapid acetylators is half of that in slow acetylators. However, there is no evidence that these differences are therapeutically important if INH is administered once daily, because plasma levels are well above inhibitory concentrations.
Rifampin is well absorbed orally and widely distributed, achieving therapeutic concentrations in lung, liver, bile, bone, and urine and entering pleural, peritoneal, and synovial fluids and CSF, tears, and saliva. Its high lipid solubility enhances its entrance into phagocytic cells, where it kills intracellular bacteria. Rifampin is metabolized in the liver to a desacetyl derivative that is biologically active. Unmetabolized drug is excreted in bile and reabsorbed from the gastrointestinal (GI) tract into the enterohepatic circulation; the deacetylated metabolite is poorly reabsorbed with eventual elimination in urine and from the GI tract. Rifampin induces its own metabolism by inducing the expression of cytochrome P450s, resulting in increased biliary excretion with continued therapy. Induction of metabolism results in reduction of the plasma life by 20% to 40% after 7 to 10 days of therapy. Patients with severe liver disease may require dose reduction, but dose adjustment is not necessary in renal failure. Oral bioavailability of rifabutin is less than that of rifampin, and the plasma half-life is approximately 10 times greater. Rifabutin is more lipid soluble than rifampin and is extensively distributed. Rifabutin also induces its own metabolism but has less of an effect on cytochrome P450s. Rifapentine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree