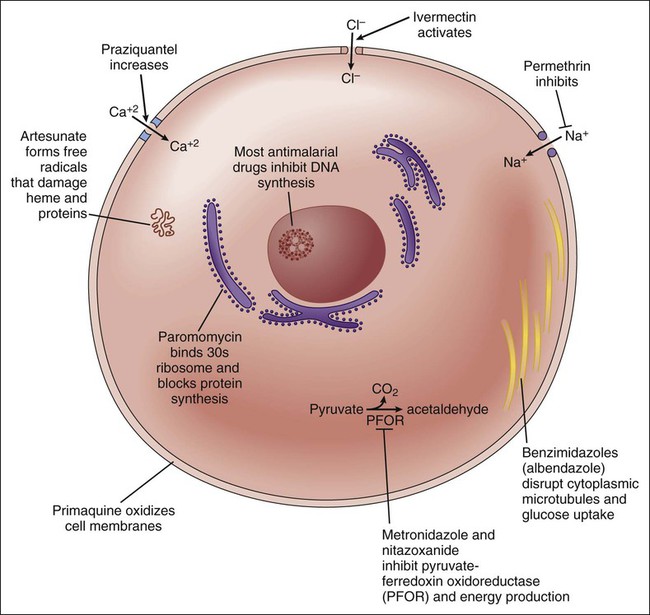
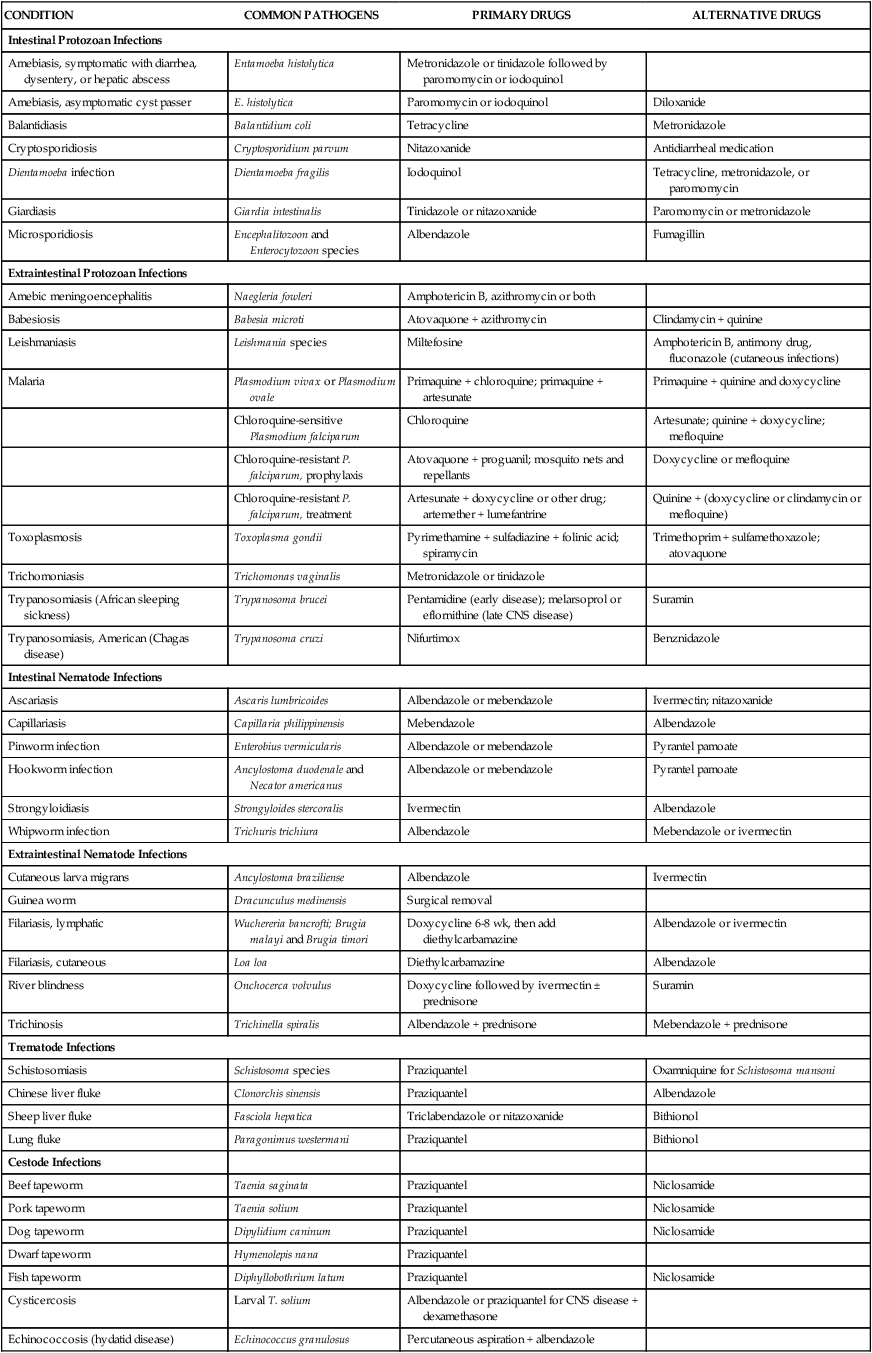
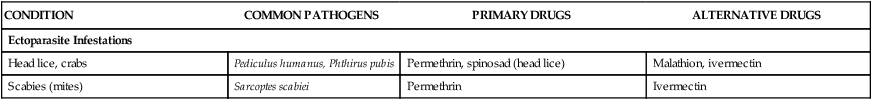
Since 1960 the introduction of new drugs has enabled remarkable advances in the chemotherapy of some endoparasitic infections. Albendazole and mebendazole have significantly improved the treatment of several intestinal nematode infections, whereas praziquantel has revolutionized the treatment of trematode and cestode infections. At the same time, metronidazole and tinidazole have provided more effective and less-toxic drugs for the treatment of amebiasis, giardiasis, and trichomoniasis. The sites and mechanisms of action of selected antiparasitic drugs are depicted in Figure 44-1. Table 44-1 provides information about the causes and treatment of numerous protozoan infections, helminthic infections, and ectoparasitic infestations. The antiparasitic agents that are commonly used or represent pharmacologic advances are discussed in this chapter. In some cases an antibacterial or antifungal agent (e.g., tetracycline or amphotericin B) is listed as either a preferred or an alternative drug; these agents are discussed in earlier chapters. A detailed discussion of other agents listed in the table is beyond the scope of this chapter. TABLE 44-1 Causes and Treatment of Parasitic Infections and Infestations Amebiasis, balantidiasis, cryptosporidiosis, giardiasis, and trichomoniasis are examples of infections caused by protozoan parasites that dwell in the lumen and tissues of their human hosts. Among the agents used to treat these infections are metronidazole, tinidazole, iodoquinol, and paromomycin (see Table 44-1).
Antiparasitic Drugs
Overview
CONDITION
COMMON PATHOGENS
PRIMARY DRUGS
ALTERNATIVE DRUGS
Intestinal Protozoan Infections
Amebiasis, symptomatic with diarrhea, dysentery, or hepatic abscess
Entamoeba histolytica
Metronidazole or tinidazole followed by paromomycin or iodoquinol
Amebiasis, asymptomatic cyst passer
E. histolytica
Paromomycin or iodoquinol
Diloxanide
Balantidiasis
Balantidium coli
Tetracycline
Metronidazole
Cryptosporidiosis
Cryptosporidium parvum
Nitazoxanide
Antidiarrheal medication
Dientamoeba infection
Dientamoeba fragilis
Iodoquinol
Tetracycline, metronidazole, or paromomycin
Giardiasis
Giardia intestinalis
Tinidazole or nitazoxanide
Paromomycin or metronidazole
Microsporidiosis
Encephalitozoon and Enterocytozoon species
Albendazole
Fumagillin
Extraintestinal Protozoan Infections
Amebic meningoencephalitis
Naegleria fowleri
Amphotericin B, azithromycin or both
Babesiosis
Babesia microti
Atovaquone + azithromycin
Clindamycin + quinine
Leishmaniasis
Leishmania species
Miltefosine
Amphotericin B, antimony drug, fluconazole (cutaneous infections)
Malaria
Plasmodium vivax or Plasmodium ovale
Primaquine + chloroquine; primaquine + artesunate
Primaquine + quinine and doxycycline
Chloroquine-sensitive Plasmodium falciparum
Chloroquine
Artesunate; quinine + doxycycline; mefloquine
Chloroquine-resistant P. falciparum, prophylaxis
Atovaquone + proguanil; mosquito nets and repellants
Doxycycline or mefloquine
Chloroquine-resistant P. falciparum, treatment
Artesunate + doxycycline or other drug; artemether + lumefantrine
Quinine + (doxycycline or clindamycin or mefloquine)
Toxoplasmosis
Toxoplasma gondii
Pyrimethamine + sulfadiazine + folinic acid; spiramycin
Trimethoprim + sulfamethoxazole; atovaquone
Trichomoniasis
Trichomonas vaginalis
Metronidazole or tinidazole
Trypanosomiasis (African sleeping sickness)
Trypanosoma brucei
Pentamidine (early disease); melarsoprol or eflornithine (late CNS disease)
Suramin
Trypanosomiasis, American (Chagas disease)
Trypanosoma cruzi
Nifurtimox
Benznidazole
Intestinal Nematode Infections
Ascariasis
Ascaris lumbricoides
Albendazole or mebendazole
Ivermectin; nitazoxanide
Capillariasis
Capillaria philippinensis
Mebendazole
Albendazole
Pinworm infection
Enterobius vermicularis
Albendazole or mebendazole
Pyrantel pamoate
Hookworm infection
Ancylostoma duodenale and Necator americanus
Albendazole or mebendazole
Pyrantel pamoate
Strongyloidiasis
Strongyloides stercoralis
Ivermectin
Albendazole
Whipworm infection
Trichuris trichiura
Albendazole
Mebendazole or ivermectin
Extraintestinal Nematode Infections
Cutaneous larva migrans
Ancylostoma braziliense
Albendazole
Ivermectin
Guinea worm
Dracunculus medinensis
Surgical removal
Filariasis, lymphatic
Wuchereria bancrofti; Brugia malayi and Brugia timori
Doxycycline 6-8 wk, then add diethylcarbamazine
Albendazole or ivermectin
Filariasis, cutaneous
Loa loa
Diethylcarbamazine
Albendazole
River blindness
Onchocerca volvulus
Doxycycline followed by ivermectin ± prednisone
Suramin
Trichinosis
Trichinella spiralis
Albendazole + prednisone
Mebendazole + prednisone
Trematode Infections
Schistosomiasis
Schistosoma species
Praziquantel
Oxamniquine for Schistosoma mansoni
Chinese liver fluke
Clonorchis sinensis
Praziquantel
Albendazole
Sheep liver fluke
Fasciola hepatica
Triclabendazole or nitazoxanide
Bithionol
Lung fluke
Paragonimus westermani
Praziquantel
Bithionol
Cestode Infections
Beef tapeworm
Taenia saginata
Praziquantel
Niclosamide
Pork tapeworm
Taenia solium
Praziquantel
Niclosamide
Dog tapeworm
Dipylidium caninum
Praziquantel
Niclosamide
Dwarf tapeworm
Hymenolepis nana
Praziquantel
Fish tapeworm
Diphyllobothrium latum
Praziquantel
Niclosamide
Cysticercosis
Larval T. solium
Albendazole or praziquantel for CNS disease + dexamethasone
Echinococcosis (hydatid disease)
Echinococcus granulosus
Percutaneous aspiration + albendazole
Ectoparasite Infestations
Head lice, crabs
Pediculus humanus, Phthirus pubis
Permethrin, spinosad (head lice)
Malathion, ivermectin
Scabies (mites)
Sarcoptes scabiei
Permethrin
Ivermectin
Drugs for Infections Caused by Lumen- and Tissue-Dwelling Protozoa
Metronidazole
Drug Properties
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antiparasitic Drugs
Only gold members can continue reading. Log In or Register to continue