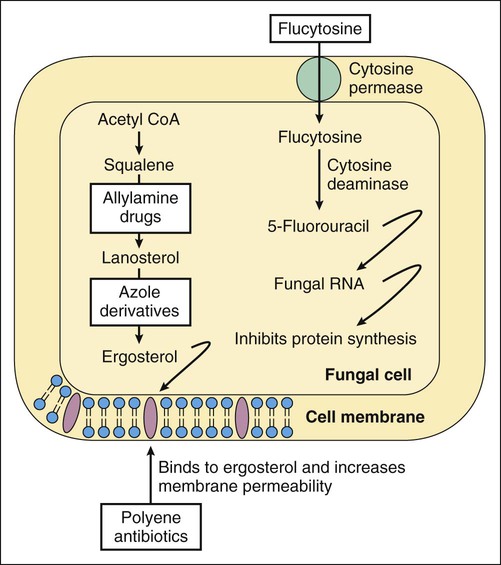
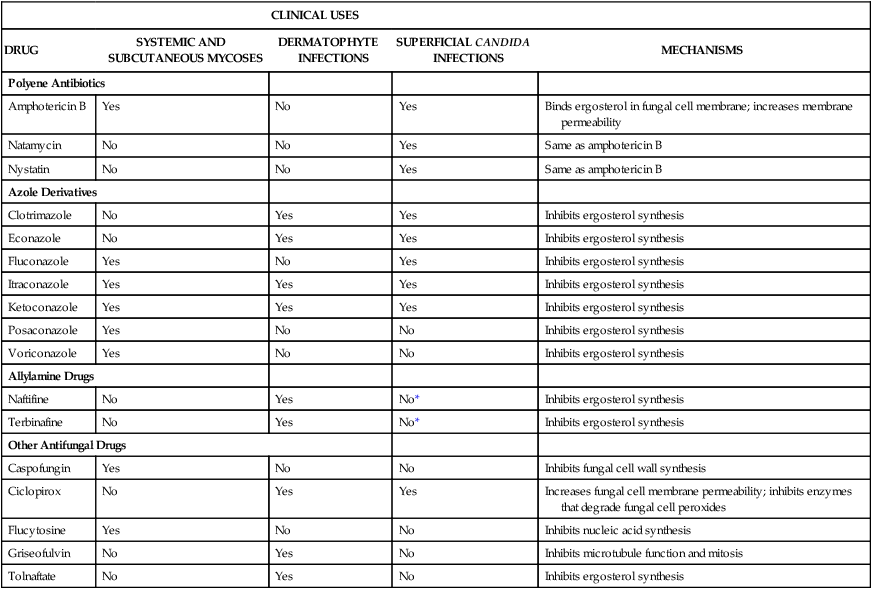
Superficial mycoses are infections of the nails, skin, and mucous membranes, and are usually caused by dermatophytes or yeasts. The most common dermatophytes are Epidermophyton, Microsporum, and Trichophyton species. Dermatophyte infections of the nails are referred to as tinea unguium or onychomycosis. Other dermatophyte infections include tinea pedis (athlete’s foot), tinea capitis (ringworm of the scalp; Box 42-1), tinea corporis (ringworm of the body), and tinea cruris (jock itch). These infections usually manifest as a rash with pruritus (itching) and erythema. Ringworm is described as an annular (ring-shaped), scaling rash with a clear center. As shown in Table 42-1, drugs used in the treatment of systemic and subcutaneous mycoses include a polyene antibiotic (amphotericin B), several azole derivatives (fluconazole, itraconazole, ketoconazole, and voriconazole), an echinocandin drug (caspofungin), and flucytosine. The other drugs listed are used in the treatment of superficial mycoses. Amphotericin B tends to be used for treating severe mycoses, whereas the azoles are used for less severe infections. Newer antifungal agents (e.g., voriconazole and caspofungin) can be used to treat invasive Candida and Aspergillus infections. Flucytosine is usually administered in combination with amphotericin B for the treatment of systemic Cryptococcus or Candida infections. TABLE 42-1 Clinical Uses and Mechanisms of Antifungal Drugs *Naftifine and terbinafine have fungistatic activity against Candida but are not approved for the treatment of candidiasis. Many antifungal drugs act by impairing plasma membrane function in fungal cells. The selective toxicity of these drugs is a result of the difference in the sterols found in fungal and mammalian cell membranes. Fungal cell membranes contain ergosterol, whereas mammalian cell membranes contain cholesterol. Some antifungal drugs bind to ergosterol and thereby increase plasma membrane permeability, whereas other drugs inhibit the synthesis of ergosterol (Fig. 42-1; see Table 42-1).
Antifungal Drugs
Overview
Fungal Infections
Clinical Uses and Mechanisms of Antifungal Drugs
CLINICAL USES
DRUG
SYSTEMIC AND SUBCUTANEOUS MYCOSES
DERMATOPHYTE INFECTIONS
SUPERFICIAL CANDIDA INFECTIONS
MECHANISMS
Polyene Antibiotics
Amphotericin B
Yes
No
Yes
Binds ergosterol in fungal cell membrane; increases membrane permeability
Natamycin
No
No
Yes
Same as amphotericin B
Nystatin
No
No
Yes
Same as amphotericin B
Azole Derivatives
Clotrimazole
No
Yes
Yes
Inhibits ergosterol synthesis
Econazole
No
Yes
Yes
Inhibits ergosterol synthesis
Fluconazole
Yes
No
Yes
Inhibits ergosterol synthesis
Itraconazole
Yes
Yes
Yes
Inhibits ergosterol synthesis
Ketoconazole
Yes
Yes
Yes
Inhibits ergosterol synthesis
Posaconazole
Yes
No
No
Inhibits ergosterol synthesis
Voriconazole
Yes
No
No
Inhibits ergosterol synthesis
Allylamine Drugs
Naftifine
No
Yes
No*
Inhibits ergosterol synthesis
Terbinafine
No
Yes
No*
Inhibits ergosterol synthesis
Other Antifungal Drugs
Caspofungin
Yes
No
No
Inhibits fungal cell wall synthesis
Ciclopirox
No
Yes
Yes
Increases fungal cell membrane permeability; inhibits enzymes that degrade fungal cell peroxides
Flucytosine
Yes
No
No
Inhibits nucleic acid synthesis
Griseofulvin
No
Yes
No
Inhibits microtubule function and mitosis
Tolnaftate
No
Yes
No
Inhibits ergosterol synthesis
Antifungal Drugs
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree