DRUG CLASSES
Fluoroquinolones
As antibiotics become resistant to various microorganisms, researchers develop drugs that affect different portions of the bacterial cell. In Chapters 7 and 8 you read about how the cell wall and protein-building capabilities of the bacteria are targeted by antibacterial drugs. In this chapter, you will read about drugs that kill bacteria by interfering with the synthesis of DNA or RNA. When these processes are interrupted, the bacterial cell cannot reproduce and it dies (Fig. 9.1). Some of these drugs are used to treat a broad spectrum of infections, others only for the treatment of one type of infection, and still others may be limited to the treatment of serious infections not treatable by other anti-infectives. The Summary Drug Table: Antibacterial Drugs That Interfere With DNA/RNA Synthesis lists the drugs discussed in this chapter.
PHARMACOLOGY IN PRACTICE

Mr. Park, 77 years old, is a patient in a skilled nursing facility receiving gemifloxacin (Factive) for a lower respiratory infection over the last 9 days. Think about the adverse reactions experienced by patients as they end a course of antibacterial drug therapy.
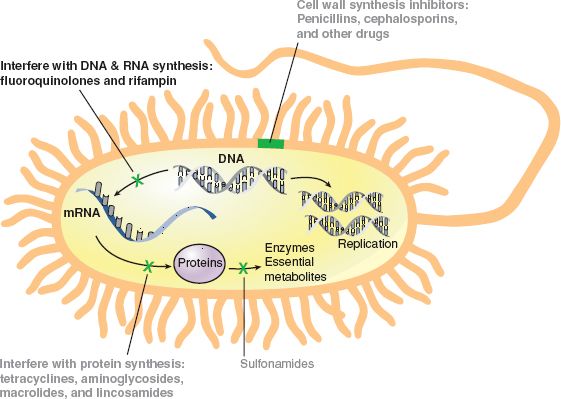
Figure 9.1 Action of bacterial DNA/RNA synthesis inhibitors such as the fluoroquinolones.
FLUOROQUINOLONES
The fluoroquinolone drugs include ciprofloxacin (Cipro), gemifloxacin (Factive), levofloxacin (Levaquin), moxifloxacin (Avelox), norfloxacin (Noroxin), and ofloxacin (Floxin).
Actions
The fluoroquinolones exert their bactericidal effect by interfering with the synthesis of bacterial DNA. This interference prevents cell reproduction, causing death of the bacterial cell (Fig. 9.1).
Uses
The fluoroquinolones are effective in treating infections caused by gram-positive and gram-negative microorganisms. They are primarily used in the treatment of the following:
• Lower respiratory infections
• Bone and joint infections
• Urinary tract infections
• Infections of the skin
• Sexually transmitted infections
Ciprofloxacin, norfloxacin, and ofloxacin are available in ophthalmic forms for infections in the eyes.
Adverse Reactions
Common adverse effects include the following:
• Nausea
• Diarrhea
• Headache
• Abdominal pain or discomfort
• Dizziness
• Photosensitivity (exaggerated skin reaction to sun exposure), which is a more serious adverse reaction seen with the administration of the fluoroquinolones, especially ofloxacin.
The administration of any drug may result in a hypersensitivity reaction, which can range from mild to severe and, in some cases, be life-threatening. Mild hypersensitivity reactions may require only discontinuing the drug, whereas the more serious reactions require immediate treatment. Bacterial or fungal superinfections and pseudomembranous colitis may occur with the use of these drugs.
Superinfections
A superinfection can develop rapidly and is potentially serious and even life-threatening. Antibiotics can disrupt the normal flora (nonpathogenic bacteria in the bowel), causing a secondary infection or superinfection. This new infection is “superimposed” on the original infection. The destruction of large numbers of nonpathogenic bacteria (normal flora) by the antibiotic alters the chemical environment. This allows uncontrolled growth of bacteria or fungal microorganisms that are not affected by the antibiotic being administered. A superinfection may occur with the use of any antibiotic, especially when these drugs are given for a long time or when repeated courses of therapy are necessary.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older adults who are debilitated, chronically ill, or taking oral antibiotics for an extended period are more likely to develop a superinfection.
Symptoms of bacterial superinfection of the bowel include diarrhea or bloody diarrhea, rectal bleeding, fever, and abdominal cramping. Pseudomembranous colitis is one type of a bacterial superinfection. This potentially life-threatening problem develops because of an overgrowth of the microorganism Clostridium difficile (C. diff) in the bowel. This organism produces a toxin that affects the lining of the colon. Signs and symptoms include severe diarrhea with visible blood and mucus, fever, and abdominal cramps. This adverse reaction usually requires immediate discontinuation of the antibiotic. Mild cases may respond to drug discontinuation. Moderate to severe cases may require treatment with intravenous (IV) fluids and electrolytes, protein supplementation, and treatment with drugs such as fidaxomicin (Dificid) to eliminate the microorganism.
Candidiasis or moniliasis is a common type of fungal superinfection. Fungal superinfections commonly occur throughout the gastrointestinal (GI) and reproductive systems. Symptoms include lesions of the mouth or tongue, vaginal discharge, and anal or vaginal itching.
Vaginal yeast infections are frequent because a yeast-like fungus normally exists in small numbers in the vagina. The multiplication rate of these microorganisms is normally slowed and kept under control by a strain of bacteria (Döderlein’s bacillus) in the vagina. If anti-infective therapy destroys these normal microorganisms of the vagina, the fungi become uncontrolled, multiply at a rapid rate, and cause symptoms of the fungal infection candidiasis (or moniliasis).
Contraindications and Precautions
Fluoroquinolones are contraindicated in patients with a history of hypersensitivity to the fluoroquinolones, in children younger than 18 years of age, and in pregnancy (pregnancy category C). These drugs also are contraindicated in patients whose lifestyles do not allow for adherence to the precautions regarding photosensitivity.
Tendonitis and tendon rupture risk increase when taking a fluoroquinolone. Although this can happen at any age, those older than 60 years who also take corticosteroids are at greater risk.
Fluoroquinolones are used cautiously in patients with diabetes, renal impairment, or a history of seizures; older patients; and patients on dialysis.
Interactions
The following interactions may occur when a fluoroquinolone is administered with another agent:
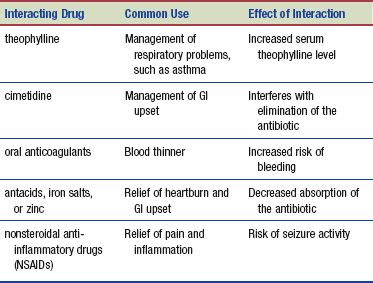
There is also a risk of severe cardiac arrhythmias when the fluoroquinolones—moxifloxacin are administered with drugs that increase the QT interval (e.g., quinidine, procainamide, amiodarone, sotalol).
NURSING PROCESS
PATIENT RECEIVING A FLUOROQUINOLONE OR MISCELLANEOUS ANTI-INFECTIVE
ASSESSMENT
Preadministration Assessment
Before administering a fluoroquinolone or miscellaneous DNA/RNA inhibitors, identify and record the signs and symptoms of the infection, and also take and record vital signs. It is particularly important to obtain a thorough allergy history, especially any drug-related allergies. The primary health care provider may order culture and sensitivity tests, and the culture is obtained before the first dose of the drug is given. Other laboratory tests, such as renal and hepatic function tests, complete blood count, and urinalysis, also may be ordered before and during drug therapy for early detection of toxic reactions.
Ongoing Assessment
During drug therapy with the miscellaneous DNA/RNA inhibitors, it is important for you to perform an ongoing assessment. In general, compare the initial signs and symptoms of the infection, which were recorded during the initial assessment, with the current signs and symptoms. Document these findings in the patient’s chart. Monitor the patient’s vital signs every 4 hours or as ordered by the primary health care provider. Notify the primary health care provider if there are changes in the vital signs, such as a significant drop in blood pressure, an increase in the pulse or respiratory rate, or a sudden increase in temperature.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Risk for Impaired Comfort related to fever
Risk for Impaired Comfort related to fever
 Risk for Impaired Skin Integrity related to photosensitivity
Risk for Impaired Skin Integrity related to photosensitivity
 Acute Pain related to tissue injury during drug therapy
Acute Pain related to tissue injury during drug therapy
 Diarrhea related to superinfection secondary to antibiotic therapy, adverse drug reaction
Diarrhea related to superinfection secondary to antibiotic therapy, adverse drug reaction
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient may include an optimal response to therapy, which includes control of the infectious process, meeting of patient needs related to the management of adverse drug reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
A variety of adverse reactions can be seen with the administration of the fluoroquinolones. You should observe the patient, especially during the first 48 hours of therapy. It is important to report the occurrence of any adverse reaction to the primary health care provider before the next dose of the drug is due. If a serious adverse reaction, such as a hypersensitivity reaction, respiratory difficulty, severe diarrhea, or a decided drop in blood pressure, occurs, then contact the primary health care provider immediately. These adverse reactions can be distressing for the patient, so be sure to offer comfort measures, such as a warm blanket or gentle touch, while awaiting a response from the primary health care provider.
Always listen to, evaluate, and report any complaints the patient may have; certain complaints may be an early sign of an adverse drug reaction. Report all changes in the patient’s condition and any new problems that occur (e.g., nausea or diarrhea) as soon as possible. The primary health care provider will determine if these changes or problems are a part of the patient’s infectious process or the result of an adverse drug reaction.
Encourage patients who receive the fluoroquinolones to increase their fluid intake. Norfloxacin is given on an empty stomach (e.g., 1 hour before or 2 hours after meals). Some drugs are made so that they release the drug over time in the body; these formulations are known as extended-release (XR), sustained-release (SR), or controlled-release (CR) drugs. Because the amount of drug would be too great if released in the body at once, it is important to swallow these medications whole. Patients should not crush, chew, or break extended-release medications. If the patient is taking an antacid, ciprofloxacin and moxifloxacin should be administered 2 to 4 hours before or 6 to 8 hours after the antacid.
INTRAVENOUS ADMINISTRATION. When these drugs are administered intravenously, inspect the needle site and area around the needle at frequent intervals for signs of extravasation, or leakage into the soft tissue, of the IV fluid. More frequent assessments are performed if the patient is restless or uncooperative. Many of the miscellaneous anti-infectives irritate the vein when administered by the IV route.
The rate of infusion is checked every 15 minutes and adjusted as needed. Inspect the vein used for the IV infusion every 4 to 8 hours for signs of tenderness, pain, and redness (which may indicate phlebitis or thrombophlebitis). If these symptoms are apparent, the IV infusion is restarted in another vein and the problem is brought to the attention of the primary health care provider.
Monitoring and Managing Patient Needs
Although the drugs in this chapter are different, many of the patient problems are similar. Consider the commonalities of the drugs to look for common problems.
IMPAIRED COMFORT: INCREASED FEVER. The infectious process is accompanied by an elevation in temperature. Monitor the vital signs, particularly the body temperature, when patients have an infection. As the anti-infective works to rid the body of the infectious organism, the body temperature should return to normal. Monitoring the vital signs (temperature, pulse, and respiration) frequently aids in assessing the drug’s effectiveness in eradicating the infection. Promptly notify the primary health care provider if a temperature rises over 101°F.
IMPAIRED SKIN INTEGRITY. The fluoroquinolone drugs cause severe photosensitivity reactions. Patients may experience “sunburn” reactions even when they use sunscreen or sunblock products. Caution patients to wear cover-up clothing with long sleeves and wide-brimmed hats when outside in addition to sunblock preparations. Remind patients that sunscreen needs to be applied repeatedly throughout the day or when going into water. Patients should be aware that glare during hazy or cloudy days can cause skin reactions as readily as direct sunlight on a clear day.
ACUTE PAIN: TISSUE INJURY. Many of these antibacterial drugs are irritating to the vein when administered IV. You should read instructions carefully for infusion rates. For intravenously administered fluoroquinolones, as with other caustic drugs, inspect the needle site and the area around the needle every hour for signs of extravasation of the IV fluid while the drug is infused. Inspect the vein used for the IV infusion every 4 hours for signs of tenderness, pain, and redness (which may indicate phlebitis or thrombophlebitis). Perform these assessments more frequently if the patient is restless or uncooperative. Be sure the proper flush solution is used after the infusion to keep the vein open and minimize irritation. If tissue or vein injury is apparent, the IV is stopped and restarted in another vein and the problem brought to the attention of the primary health care provider.
 NURSING ALERT
NURSING ALERT
There is a risk with all fluoroquinolone drugs of causing pain, inflammation, or rupture of a tendon. The Achilles tendon is particularly vulnerable. Those 60 years of age and older who take corticosteroids are at greatest risk for tendon rupture.
DIARRHEA. Frequent liquid stools may be an indication of a superinfection or pseudomembranous colitis. If pseudomembranous colitis occurs, it is usually seen 4 to 10 days after treatment is started.
Teach the patient or family to feel confident in the ability to check bowel movements and immediately reporting to the primary health care provider the occurrence of diarrhea or loose stools containing blood and mucus. It may be necessary to discontinue drug therapy and institute treatment for diarrhea, a superinfection, or pseudomembranous colitis.
If blood and mucus appear to be in the stool, save a sample of the stool and test for occult blood using a test such as Hemoccult. If the stool tests positive for blood, the sample is saved for possible additional laboratory testing.
Educating the Patient and Family
When you teach the patient and family members, explain all adverse reactions associated with the specific prescribed antibiotic. Use written materials in the language of preference to describe the signs and symptoms of potentially serious adverse reactions, such as hypersensitivity reactions, moderate to severe diarrhea, and sudden onset of chills and fever. The patient should feel confident about when to contact the primary health care provider if such symptoms occur. Instruct the patient not to take the next dose of the drug until the problem is discussed with the primary health care provider (see Patient Teaching for Improved Patient Outcomes: Superinfections).
EVALUATION
 Therapeutic response is achieved, and there is no evidence of infection.
Therapeutic response is achieved, and there is no evidence of infection.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
• Patient reports comfort without fever.
• Skin is intact and free of inflammation, irritation, infection, or ulcerations.
• Patient reports no pain or injury.
• Patient does not experience diarrhea.
 Patient and family express confidence and demonstrate an understanding of the drug regimen.
Patient and family express confidence and demonstrate an understanding of the drug regimen.
PHARMACOLOGY IN PRACTICE
THINK CRITICALLY
 Mr. Park complains about gas pains in his stomach and lots of “rumbling feelings.” The nursing assistant reports that he has made multiple trips to the bathroom due to diarrhea for the past 2 days. He gets upset and says he can’t wait for ambulation assistance; the nursing assistant is concerned he will get up at night by himself and fall. Analyze whether this matter should be investigated.
Mr. Park complains about gas pains in his stomach and lots of “rumbling feelings.” The nursing assistant reports that he has made multiple trips to the bathroom due to diarrhea for the past 2 days. He gets upset and says he can’t wait for ambulation assistance; the nursing assistant is concerned he will get up at night by himself and fall. Analyze whether this matter should be investigated.
Patient Teaching for Improved Patient Outcomes
Superinfections
Antibiotics are one of the most commonly administered types of drug therapy in the home. Any patient taking antibacterial drugs is susceptible to superinfection. Make sure the patient knows the signs and symptoms of superinfection. A bacterial superinfection commonly occurs in the bowel.
When you teach, make sure your patient understands the following:
Report any of the following:
✓ Fever
✓ Burning sensation in the mouth or throat
✓ Localized redness, inflammation, and excoriation, particularly inside the mouth, in the groin, or in skin folds of the anogenital area
✓ Abdominal cramps
✓ Scaly, reddened, papular rash commonly in the breast folds, axillae, groin, or umbilicus
✓ Diarrhea, possibly severe with visible blood and mucus
A fungal superinfection commonly occurs in the mouth, vagina, and anogenital areas. Teach the patient to report any of the following:
✓ Creamy white, lace-like patches on the tongue, mouth, or throat
✓ White or yellow vaginal discharge
✓ Anal or vaginal itching
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


