DRUG CLASSES
PHARMACOLOGY IN PRACTICE

Each chapter in this book features a specific case study corresponding to the drug therapy in each chapter. In this chapter, the patient featured is Mrs. Moore. She is 85 years old and has been prescribed a sulfonamide for a urinary tract infection (UTI). She is to take the drug for 10 days. Mrs. Moore seems forgetful and a bit confused as you talk with her. As you begin learning about the preassessment interview, think about Mrs. Moore.
Drugs that are used against bacteria are either bacteriostatic (they slow or retard the multiplication of bacteria) or bactericidal (they destroy the bacteria). To choose the appropriate drug, the primary health care provider needs to know how sensitive the bacteria will be to the drugs.
Culture and Sensitivity Testing
To determine if a specific type of bacteria is sensitive to an antibiotic drug, culture and sensitivity tests are performed. A culture is performed by placing infectious material obtained from areas such as the skin, respiratory tract, and blood on a culture plate that contains a special growing medium. This growing medium is “food” for the bacteria. After a specified time, the bacteria are examined under a microscope and identified. The sensitivity test involves placing the infectious material on a separate culture plate and then placing small disks impregnated with various antibiotics over the area. After a specified time, the culture plate is examined. If there is little or no growth around a disk, the bacteria are considered sensitive to that particular antibiotic. Therefore, the infection will be controlled by this antibiotic. If there is considerable growth around the disk, then the bacteria are considered resistant to that particular antibiotic, and the infection will not be controlled by this antibiotic (Fig. 6.1).
SULFONAMIDES
Sulfonamides (commonly called sulfa drugs) are antibacterial agents, meaning they are active against bacteria. Sulfadiazine, sulfisoxazole, and sulfamethizole are examples of sulfonamide preparations. Although the use of sulfonamides began to decline after the introduction of more effective anti-
infectives such as the penicillins and other antibiotics, these drugs remain important for the treatment of certain types of infections.
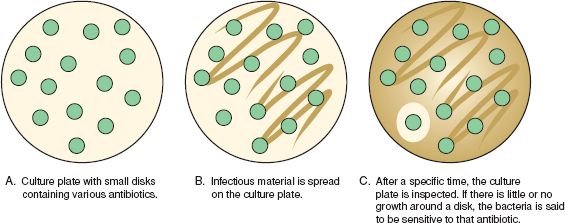
Figure 6.1 Culture and sensitivity tests indicate which drug is most effective against the bacteria on the culture plate.
Actions
The sulfonamides are primarily bacteriostatic because of their ability to inhibit the activity of folic acid in bacterial cell metabolism. The sulfonamides are well absorbed by the gastrointestinal (GI) system and excreted by the kidneys (see Chapter 48). They are often used to control infections caused by both gram-positive and gram-negative bacteria, such as Escherichia coli, Staphylococcus aureus, and Klebsiella and Enterobacter species. Once the rate of bacterial multiplication is slowed, the body’s own defense mechanisms (white blood cells) are able to rid the body of the invading microorganisms and therefore control the infection.
When sulfasalazine interacts with intestinal bacteria, it helps to inhibit the inflammatory process, which is how the drug works to treat ulcerative colitis.
Uses
The sulfonamides are often used according in the treatment of infections such as:
• Urinary tract infections (UTIs) and acute otitis media
• Ulcerative colitis
• Mafenide (Sulfamylon) and silver sulfadiazine (Silvadene) are topical sulfonamides used in the treatment and prevention of infections in second- and third-degree burns.
Additional uses of the sulfonamides are given in the Summary Drug Table: Sulfonamides.
Adverse Reactions
The sulfonamides are capable of causing a variety of adverse reactions. Some of these are serious or potentially serious; others are mild. Anorexia (loss of appetite) is an example of a mild adverse reaction.
Gastrointestinal System Reactions
• Nausea, vomiting, anorexia
• Diarrhea, abdominal pain
• Stomatitis (inflammation of the mouth)
In some instances, these may be mild. At other times they may cause serious problems, such as pronounced weight loss, requiring discontinuation of the drug.
Other Reactions
• Chills, fever
• Crystalluria (crystals in the urine)
• Photosensitivity
Various types of hypersensitivity (allergic) reaction may be seen during sulfonamide therapy, including urticaria (hives), pruritus (itching), generalized skin eruptions, or severe reactions leading to potentially lethal conditions such as toxic epidermal necrolysis (TEN) or Stevens-Johnson syndrome (SJS).
 NURSING ALERT
NURSING ALERT
TEN and SJS are serious and sometimes fatal hypersensitivity reactions. Widespread sloughing of both the skin and mucous membranes can occur. Internal organ involvement can cause death. Patients with SJS may complain of fever, cough, muscular aches and pains, and headache, all of which are signs and symptoms of many other disorders. Be alert for the additional signs of lesions on the skin and mucous membranes, eyes, and other organs, a diagnostically important indicator of these problems. The lesions appear as red wheals or blisters, often starting on the face, in the mouth, or on the lips, neck, and extremities. These conditions may occur with the administration of other types of drugs. Notify the primary health care provider and withhold the next dose of the drug. In addition, exercise care to prevent injury to the involved areas.
The most frequent adverse reaction seen with the topical application of a sulfonamide is a burning sensation or pain when the drug is applied to the skin. Other possible allergic reactions include rash, itching, edema, and urticaria. Burning, rash, and itching may also be seen with the use of silver sulfadiazine. It may be difficult to distinguish between adverse reactions due to the use of mafenide or silver sulfadiazine and those that occur from a severe burn injury or from other agents used for the management of burns.
The following hematologic changes may occur during prolonged sulfonamide therapy:
• Leukopenia—decrease in the number of white blood cells
• Thrombocytopenia—decrease in the number of platelets
• Aplastic anemia—deficient red blood cell production in the bone marrow
These changes are examples of serious adverse reactions. If any of these occur, discontinuation of sulfonamide therapy may be required.
Contraindications
The sulfonamides are contraindicated in patients with hypersensitivity to the sulfonamides, during lactation, and in children younger than 2 years of age. The sulfonamides are not used near the end (at term) of pregnancy (pregnancy category D). If the sulfonamides are given near the end of pregnancy, significantly high blood levels of the drug may occur, causing jaundice or hemolytic anemia in the neonate. In addition, the sulfonamides are not used for infections caused by group A beta (β)-hemolytic streptococci because the sulfonamides have not been shown to be effective in preventing the complications of rheumatic fever or glomerulonephritis.
Precautions
The sulfonamides are used with caution in patients with renal impairment, hepatic impairment, or bronchial asthma.
These drugs are given with caution to patients with allergies. Safety for use during pregnancy has not been established (pregnancy category C, except at term; see above).
Interactions
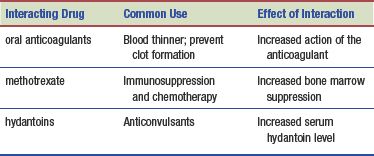
The following interactions may occur when a sulfonamide is administered with another agent:
 CHRONIC CARE CONSIDERATIONS
CHRONIC CARE CONSIDERATIONS
When diabetic patients are prescribed sulfonamides, assess for a possible hypoglycemic reaction. Sulfonamides may inhibit the (hepatic) metabolism of the oral hypoglycemic drugs tolbutamide and chlorpropamide (Diabinese).
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Cranberries and cranberry juice are commonly used folk remedies for preventing and relieving symptoms of UTIs. The use of cranberries in combination with antibiotics has been recommended by physicians for the long-term suppression of UTIs. Cranberries are thought to prevent bacteria from attaching to the walls of the urinary tract. The suggested dose is 6 ounces of juice twice daily. Cranberry capsules are not recommended because the fluid for hydration may be as helpful as the berries (Brown, 2012). Extremely large doses can produce GI disturbances, such as diarrhea or abdominal cramping. Although cranberries may relieve symptoms or prevent the occurrence of a UTI, their use will not cure a UTI. If an individual suspects a UTI, medical attention is necessary.
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
Before the initial administration of the drug, it is important to assess the patient’s general appearance and take and record the vital signs. Obtain information regarding the symptoms experienced by the patient and the length of time these symptoms have been present. If an elderly patient appears distracted or the family notes sudden confusion, these may be signs of a genitourinary infection. Many infections are diagnosed and treated in ambulatory settings; therefore, it is important to ask about self-remedies the patient may have tried before seeing a primary health care provider. Depending on the type and location of the infection or disease, review the results of tests such as a urine culture, urinalysis, complete blood count, intravenous pyelogram, renal function tests, and examination of the stool.
Ongoing Assessment
During the course of therapy, evaluate the patient at periodic intervals for response to the drug—that is, a relief of symptoms and a decrease in temperature (if it was elevated before therapy started), as well as the occurrence of any adverse reactions.
If fever is present and the patient’s temperature suddenly increases or if the temperature was normal and suddenly increases, instruct the patient to contact the primary health care provider immediately.
The ongoing assessment for patients receiving sulfasalazine for ulcerative colitis includes observation for evidence of the relief or intensification of the symptoms of the disease. Ask the patient to monitor when using the bathroom for changes in number or appearance of the stool. The patient should contact the primary health care provider regarding changes.
When administering a sulfonamide for a burn, inspect the burned areas every 1 to 2 hours, because some treatment regimens require keeping the affected areas covered with the mafenide or silver sulfadiazine ointment at all times. Any adverse reactions should be reported immediately to the primary health care provider.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Impaired Urinary Elimination related to effect on the bladder from sulfonamides
Impaired Urinary Elimination related to effect on the bladder from sulfonamides
 Impaired Skin Integrity related to burns
Impaired Skin Integrity related to burns
 Impaired Skin Integrity related to photosensitivity or severe allergic reaction to the sulfonamides
Impaired Skin Integrity related to photosensitivity or severe allergic reaction to the sulfonamides
 Risks for (Secondary) Infection related to lowered white blood cell count resulting from sulfonamide therapy
Risks for (Secondary) Infection related to lowered white blood cell count resulting from sulfonamide therapy
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected patient outcomes depend on the reason for administration of the sulfonamide but may include an optimal response to drug therapy, meeting patient needs related to the management of adverse drug reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
The patient receiving a sulfonamide drug almost always has an active infection. Some patients may be receiving one of these drugs to prevent an infection (prophylaxis) or as part of the management of a disease such as ulcerative colitis.
Unless the primary health care provider orders otherwise, give sulfonamides to the patient whose stomach is empty—that is, 1 hour before or 2 hours after meals. If GI irritation occurs, give sulfasalazine with food or immediately after meals.
Sulfasalazine may cause the urine and skin to take on an orange-yellow color; this is normal. Crystalluria may occur during administration of a sulfonamide, although this problem occurs less frequently with some of the newer sulfonamide preparations. Often, this potentially serious problem can be prevented by increasing fluid intake during sulfonamide therapy. It is important to instruct the patient to drink a full glass (8 ounces) of water when taking an oral sulfonamide and to drink at least eight large glasses of water each day until therapy is finished.
Monitoring and Managing Patient Needs
Observe the patient for adverse reactions, especially an allergic reaction (see Chapter 1). If one or more adverse reactions should occur, withhold the next dose of the drug and notify the primary health care provider.
IMPAIRED URINARY ELIMINATION. Because one adverse effect of the sulfonamide drugs is altered elimination patterns, it is important to help the patient maintain adequate fluid intake and output. Encourage patients to increase fluid intake to 2000 mL or more per day to prevent crystalluria and stones (calculi) forming in the genitourinary tract, as well as to aid in removing microorganisms from the urinary tract. It is important to measure and record the patient’s intake and output every 8 hours and notify the primary health care provider if the urinary output decreases or the patient fails to increase his or her oral intake (Fig. 6.2).

Figure 6.2 Nurses monitor for decreased urinary output and possible crystal formation in the patient receiving sulfonamides.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


