Figure 11–1 Classification and pathophysiology of ischemic heart disease. Variant angina, also called Prinzmetal’s angina, is considered a form of unstable angina if the angina attacks occur with increasing severity or frequency.
Typical angina results from formation of atherosclerotic plaques in vessel walls that limit coronary blood flow and the supply of oxygen to the myocardium. The symptoms of angina, often described as resembling a heavy weight or pressure on the chest, occur when the oxygen supply is insufficient to meet the demand imposed by increased physical exertion. The condition is called stable angina if angina attacks have similar characteristics and occur in similar circumstances each time. It is known as unstable angina if the frequency and severity of attacks increase over time. Unstable angina, which may be caused by occlusion of a coronary vessel by small platelet thrombi and ruptured atheromatous plaque, is often the forerunner of MI. Variant angina (Prinzmetal’s angina) is caused by acute coronary vasospasm and may occur at rest or during sleep.
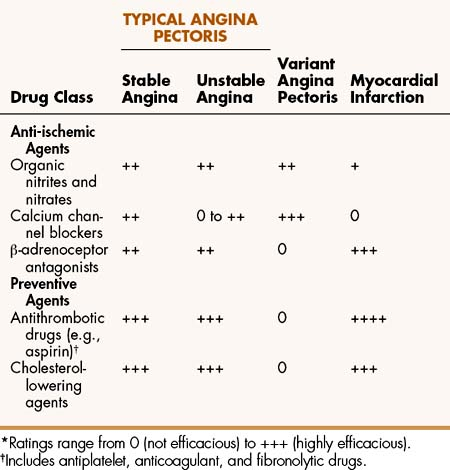
Table 11–1 lists five classes of drugs and compares their efficacy in treating different forms of CHD. This chapter focuses on the anti-ischemic agents: organic nitrites and nitrates, calcium channel blockers (CCBs), and β-adrenoceptor antagonists (β-blockers), which are the primary agents used to treat angina symptoms. Chapter 15 discusses drugs for hyperlipidemia, and Chapter 16 covers antithrombotic drugs (e.g., aspirin). These two groups of drugs have been shown to reduce the risk of MI and death in persons with CHD.
Mechanisms and Effects of Antianginal Drugs
The anti-ischemic agents used in treating angina serve to prevent or counteract myocardial ischemia and thereby increase exercise tolerance and reduce the frequency of anginal attacks. This is accomplished by restoring the balance between myocardial oxygen supply and demand, either by increasing oxygen supply or decreasing oxygen demand. The factors that determine supply and demand are illustrated in Figure 11–2.
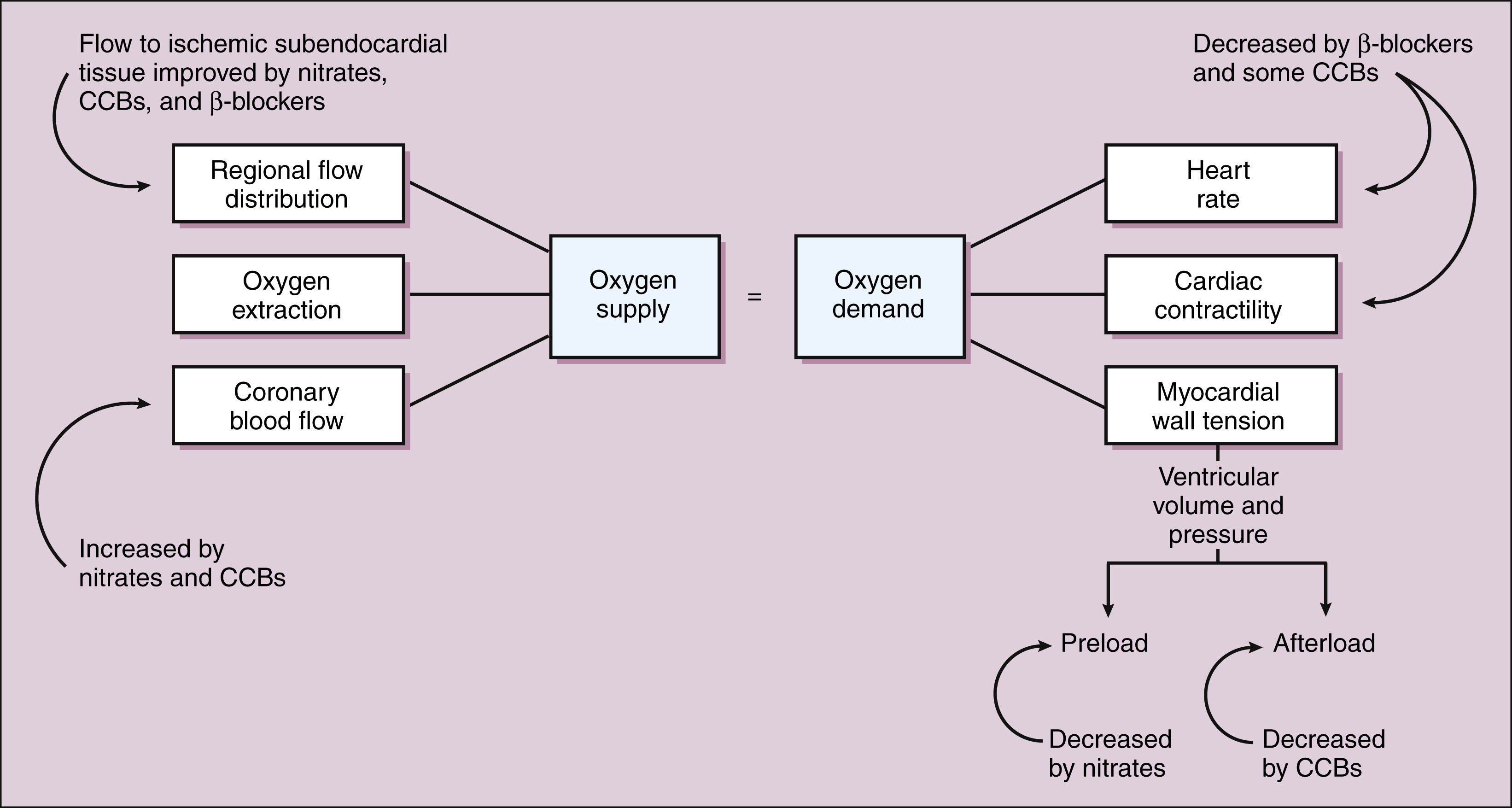
Figure 11–2 Effects of organic nitrites and nitrates, CCBs, and β-adrenoceptor antagonists (β-blockers) on myocardial oxygen supply and demand.
Myocardial oxygen supply is primarily determined by coronary blood flow and regional flow distribution but is also influenced by oxygen extraction. In patients with coronary artery disease, the subendocardial tissue is more likely to suffer from ischemia because it is not as well perfused as the subepicardial tissue. The use of nitrates or CCBs (vasodilator drugs) can reduce ischemia by increasing both the total coronary flow and the distribution of coronary flow to ischemic subendocardial tissue. The drugs increase the distribution of blood flow to subendocardial tissue by dilating collateral vessels and by decreasing intraventricular pressure and the resistance to perfusion of this tissue. The use of β-blockers may improve the distribution of coronary flow by reducing intraventricular pressure. Cardiac tissue extracts a higher percentage of oxygen from blood than does any other tissue, and this factor is not affected by existing drugs.
Myocardial oxygen demand is largely determined by the amount of energy required to support the work of the heart. The factors that influence cardiac work include the heart rate, cardiac contractility, and myocardial wall tension. Contractility is directly related to the amount of cytosolic calcium that is available to stimulate the shortening of myocardial fibers. As contractility increases, the velocity of fiber shortening and the peak systolic muscle tension also increase. Myocardial wall tension is equal to the product of ventricular volume (radius) and pressure, divided by wall thickness. Ventricular wall tension is primarily determined by arterial and venous blood pressure.
Antianginal drugs act by several mechanisms to reduce myocardial oxygen demand. The β-blockers decrease heart rate and contractility, whereas the organic nitrates and CCBs reduce wall tension via their effects on ventricular volume and pressure. Dilation of veins decreases venous pressure, cardiac filling pressure, and ventricular diastolic pressure (preload). Dilation of arteries decreases arterial and aortic pressure and thereby reduces ventricular systolic pressure (afterload) and impedance to ventricular ejection of blood. The organic nitrates act primarily on venous tissue and predominantly affect preload, whereas the CCBs act mostly on arteriolar muscle to reduce afterload.
In typical angina, which is caused by increased oxygen demand in the face of a limited oxygen supply, vasodilators and β-blockers act primarily by decreasing oxygen demand through the mechanisms described above. They can also increase the perfusion of ischemic subendocardial tissue. In variant angina, chest pain usually occurs at rest (when oxygen demand is relatively low), and ischemia results in a reduction in oxygen supply secondary to coronary artery spasm. Under these conditions, vasodilators increase oxygen supply by relaxing coronary smooth muscle and restoring normal coronary flow. The β-blockers are not effective in the treatment of variant angina, because they cannot counteract vasospasm and increase coronary blood flow. The β-blockers may actually reduce coronary blood flow by blocking the vasodilative effect of epinephrine, an effect that is mediated by β2-adrenoceptors in coronary smooth muscle.
VASODILATORS
Two classes of vasodilators are used in the management of angina pectoris. The first consists of organic nitrites and nitrates and the second consists of CCBs.
Organic Nitrites and Nitrates
The organic nitrites and nitrates are polyol esters of nitrous acid and nitric acid, respectively. Amyl nitrite, the only nitrite compound used to treat angina, is administered by inhalation. Nitroglycerin (glyceryl trinitrate), isosorbide dinitrate, and isosorbide mononitrate are compounds with sufficient solubility in water and lipids to enable rapid dissolution and absorption following sublingual, oral, or transdermal administration. The onset and duration of action of these drugs varies with their physical properties, route of administration, and rate of biotransformation. Amyl nitrite has the most rapid onset and the shortest duration of action, whereas isosorbide compounds have the slowest onset and the longest duration. Nitroglycerin has an intermediate onset and duration. All of these compounds are extensively metabolized in the liver.
Amyl Nitrite
Amyl nitrite is a volatile liquid that can be inhaled and absorbed through the lungs. Its action is rapid in onset (within 30 seconds) and brief in duration (3–5 minutes). Amyl nitrite is effective in the treatment of acute angina attacks, as well as in the initial management of cyanide poisoning. In patients with cyanide poisoning, amyl nitrite is used until intravenous sodium nitrite and sodium thiosulfate can be administered. The nitrites oxidize hemoglobin to methemoglobin. In comparison with hemoglobin, methemoglobin has a greater affinity for cyanide, and this allows it to trap the compound in the form of cyanmethemoglobin. Thiosulfate is then administered to convert cyanide to inactive thiocyanate.
Nitroglycerin, Isosorbide Dinitrate, and Isosorbide Mononitrate
PHARMACOKINETICS
Nitroglycerin and the isosorbide preparations are nitrate compounds used to prevent and treat angina attacks.
Nitroglycerin is available in formulations for sublingual, transdermal, topical, oral, and intravenous administration. The drug’s solubility in water and lipids permits its rapid dissolution and absorption after sublingual or buccal administration for the treatment of acute angina attacks. Its high lipid solubility and low dosage have enabled the formulation of skin patches for transdermal administration. The patches slowly release the drug for absorption through the skin into the circulation and are used in the prevention of angina attacks. In ointment form, nitroglycerin is absorbed through the skin over a period of several hours. The ointment is primarily used in hospitalized patients with angina or MI. Nitroglycerin is administered orally in the form of sustained-release capsules that are used to prevent angina attacks. The drug is well absorbed from the gut but undergoes considerable first-pass inactivation, thereby necessitating the use of larger doses when administered orally. Nitroglycerin is also available as an intravenous solution that is used chiefly to reduce preload but also to reduce afterload in patients who have acute heart failure associated with MI and other conditions.
Isosorbide dinitrate can be administered sublingually or orally and is used for both the prevention and the treatment of angina attacks. Isosorbide dinitrate produces the samepharmacologic effects as nitroglycerin, but it has a slightly slower onset of action and a greater duration of action. It is converted to an active compound, isosorbide mononitrate, which is now available as a drug preparation itself.
MECHANISMS AND PHARMACOLOGIC EFFECTS
The organic nitrates are believed to act by releasing nitric oxide in vascular smooth muscle cells (Fig. 11–3). The precise mechanisms by which nitroglycerin and other organic nitrates release nitric oxide are still under investigation. Some evidence suggests the involvement of thiol (−SH) compounds in this process. Recent evidence supports the involvement of aldehyde dehydrogenase in the release of nitric oxide as well as in the development of nitrate tolerance (see “TOLERANCE”).
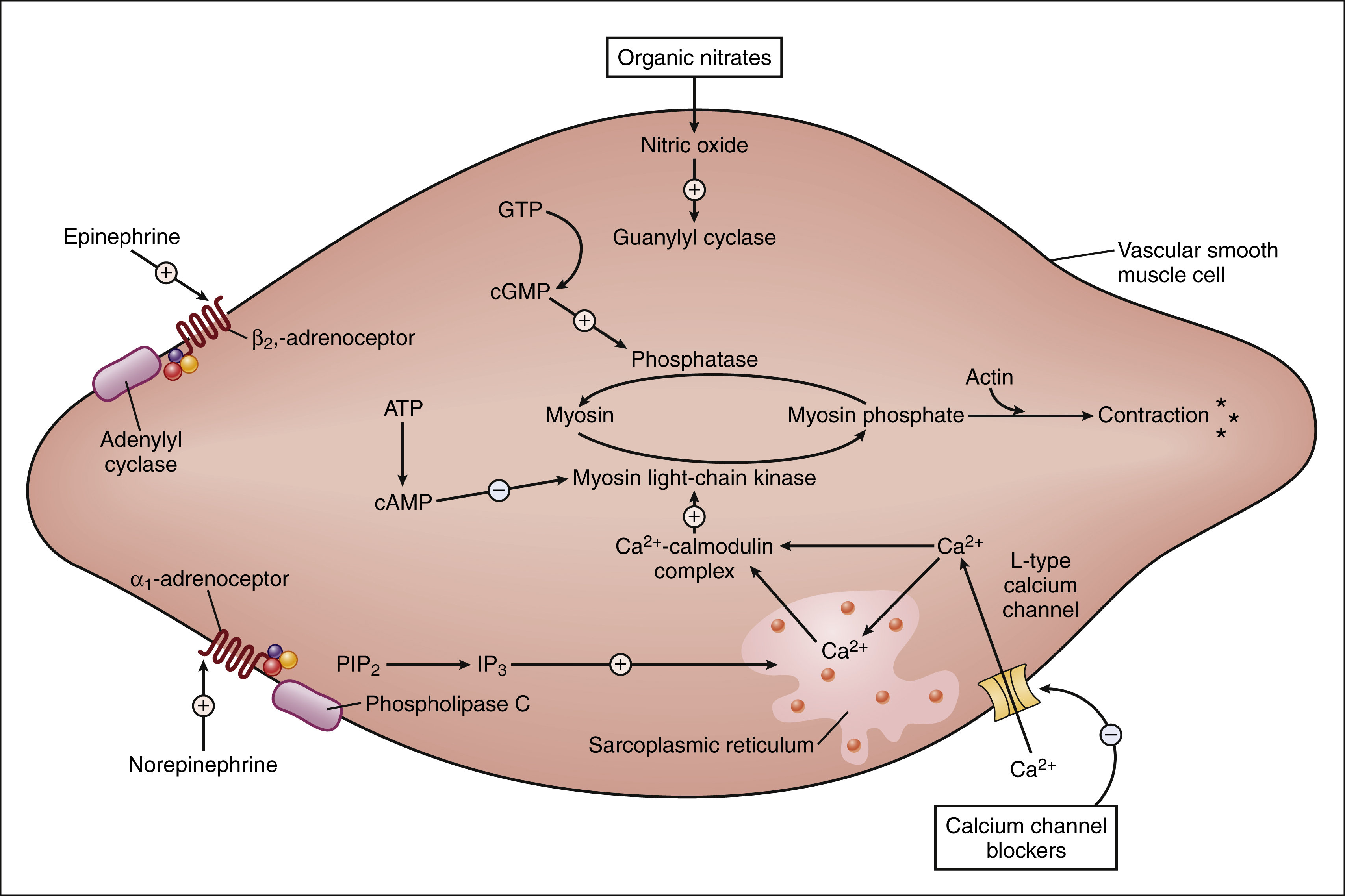
Figure 11–3 Regulation of vascular smooth muscle contraction. Vascular smooth muscle contraction occurs when calcium (Ca2+) enters smooth muscle via L-type calcium channels, binds to calmodulin, and activates myosin light-chain kinase. This leads to formation of myosin phosphate, which interacts with actin to cause muscle contraction. Calcium influx is inhibited by CCBs, leading to muscle relaxation. Organic nitrates release nitric oxide, which activates guanylyl cyclase and increases formation of cGMP. Investigators believe that cGMP causes smooth muscle relaxation by activating kinases that increase myosin phosphatase activity and decrease myosin phosphate levels. α1-adrenoceptor agonists activate phospholipase C (PLC), which increases formation of inositol triphosphate (IP3) from phosphatidylinositol bisphosphate (PIP2), leading to increased release of calcium from the sarcoplasmic reticulum. β2-adrenoceptor agonists increase formation of cAMP, which activates kinases that inhibit myosin light-chain kinase.
Nitric oxide is a gas that activates guanylyl cyclase, forming cyclic guanosine monophosphate (cGMP). Cyclic GMP activates cGMP-dependent kinases that appear to cause relaxation of vascular smooth muscle by phosphorylating proteins that decrease intracellular calcium mobilization and decrease phosphorylation of myosin light chains by increasing activity of myosin light-chain phosphatase (an enzyme that removes phosphate; Fig. 11–3).
The organic nitrates preferentially relax venous smooth muscle and have a relatively smaller effect on arteriolar smooth muscle. This leads to venous pooling of blood, a decrease in venous blood return to the heart, and a decrease in ventricular volume, pressure, and wall tension. By these mechanisms, the nitrates reduce cardiac work and oxygen demand and thereby relieve or prevent angina pectoris. By reducing cardiac preload, the nitrates also reduce cardiac output and thereby contribute to a reduction in blood pressure. If blood pressure falls sufficiently, reflex tachycardia can be invoked. The nitrates do not have any direct effects on myocardial tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree