DRUG CLASSES
Local anesthetics
Preanesthetics
General anesthetic agents
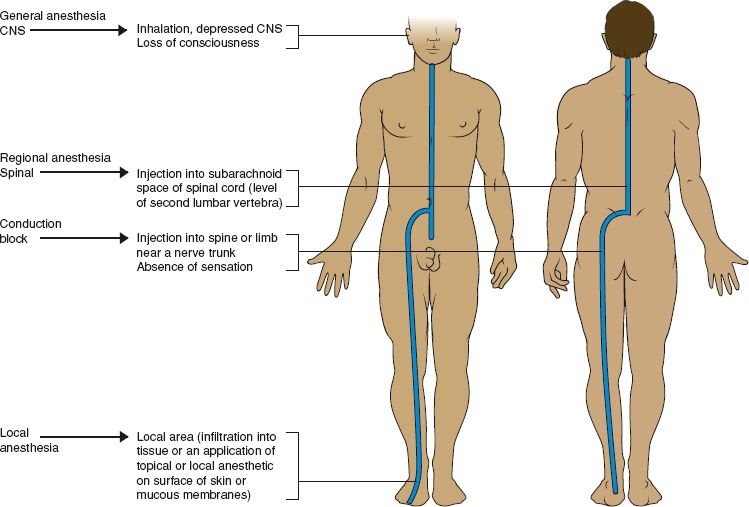
Anesthesia is a loss of feeling or sensation. Anesthesia may be induced by various drugs that can bring about partial or complete loss of sensation. There are two types of anesthesia: local anesthesia and general anesthesia. Local anesthesia, as the term implies, is the provision of a sensation-free state in a specific area (or region). With a local anesthetic, the patient is fully awake but does not feel pain in the area that has been anesthetized. However, some procedures performed under local anesthesia may require the patient to be sedated. Although not fully awake, sedated patients may still hear what is going on around them. General anesthesia is the provision of a sensation-free state for the entire body. When a general anesthetic is given, the patient loses consciousness and feels no pain. Reflexes, such as the swallowing and gag reflexes, are lost during deep general anesthesia (Fig. 17.1). Anesthetic drugs are included here because they eliminate the sensation of pain, which completes the spectrum of pain management in this unit.
Both physicians and nurses administer anesthesia. An anesthesiologist is a physician with special training in administering anesthesia. A nurse anesthetist is a nurse with at least a master’s degree and special training who is qualified to administer anesthetics.
PHARMACOLOGY IN PRACTICE

Lillian Chase has asked her primary health care provider to remove a mole on her arm. You are asked to draw up into a syringe the medication to numb the area. After reading this chapter, see if you can make the appropriate selection.
LOCAL ANESTHESIA
The various methods of administering a local anesthetic include topical application, local infiltration, and regional anesthesia.
Topical Anesthesia
Topical anesthesia involves the application of the anesthetic to the surface of the skin, open area, or mucous membrane. The anesthetic may be applied with a cotton swab or sprayed on the area. This type of anesthesia may be used to desensitize the skin or mucous membrane to the injection of a deeper local anesthetic. In some instances, topical anesthetics are dispensed in a transdermal form for chronic pain relief.
Local Infiltration Anesthesia
Local infiltration anesthesia is the injection of a local anesthetic drug into tissues. This type of anesthesia may be used for dental procedures, the suturing of small wounds, or making an incision into a small area, such as that required for removing a superficial piece of tissue for biopsy.
Regional Anesthesia
Regional anesthesia is the injection of a local anesthetic around nerves so that the area supplied by these nerves will not send pain signals to the brain. The anesthetized area is usually larger than the area affected by local infiltration anesthesia. Spinal anesthesia and conduction blocks are two types of regional anesthesia.
Spinal Anesthesia
Spinal anesthesia is a type of regional anesthesia that involves the injection of a local anesthetic drug into the subarachnoid space of the spinal cord, usually at the level of the second lumbar vertebra. There is a loss of feeling (anesthesia) and movement in the lower extremities, lower abdomen, and perineum.
Conduction Blocks
A conduction block is a type of regional anesthesia produced by injection of a local anesthetic drug into or near a nerve trunk. Examples of a conduction block include an epidural block (injection of a local anesthetic into the space surrounding the dura of the spinal cord), a transsacral (caudal) block (injection of a local anesthetic into the epidural space at the level of the sacrococcygeal notch), and a brachial plexus block (injection of a local anesthetic into the brachial plexus). Epidural—especially—and transsacral blocks are often used in obstetrics. A brachial plexus block may be used for surgery of the arm or hand.
The placement of the needle or a catheter requires strict aseptic technique by a skilled physician. Drug injected through the catheter spreads freely throughout the tissues in the space, interrupting pain conduction at the points where sensory nerve fibers exit from the spinal cord.
A catheter may be placed to give intermittent injections to maintain anesthesia over time such as the immediate postoperative period.
Preparing the Patient for Local Anesthesia
Depending on the procedure performed, preparing the patient for local anesthesia may or may not be similar to preparing the patient for general anesthesia. For example, administering a local anesthetic for dental surgery or for suturing a small wound may require that you explain to the patient how the anesthetic will be administered, take the patient’s allergy history, and, when applicable, prepare the area to be anesthetized, which may involve cleaning the area with an antiseptic or shaving the area. Other local anesthetic procedures may require the patient to be fasting (taking in nothing by mouth), because a sedative may also be administered. This conscious sedation would include administering an intravenous (IV) sedative, such as the central nervous system (CNS) depressant drug midazolam, during some local anesthetic procedures, such as cataract surgery or a colonoscopy.
Administering Local Anesthesia
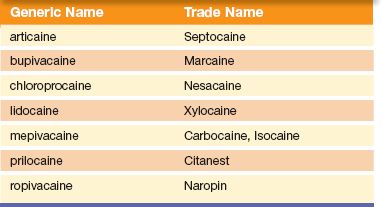
The physician or dentist administers a local injectable anesthetic. These drugs may be mixed with epinephrine to cause local vasoconstriction. The drug stays in the tissue longer when epinephrine is used. This is contraindicated, however, when the local anesthetic is used on an extremity. When preparing these medications, you should proceed cautiously and be aware of when epinephrine is to be used and when it should not be used. Table 17.1 lists the more commonly used local anesthetics.
Nursing Responsibilities
When caring for a patient receiving local anesthesia, you may be responsible for applying a dressing to the surgical area if appropriate. Typically, when using local anesthesia, you will instruct the family or caregiver how to observe the area for bleeding, oozing, or other problems after the administration of the anesthetic and when to contact the primary health care provider.
Table 17.1 Example of Local Anesthetics
PREANESTHETIC DRUGS
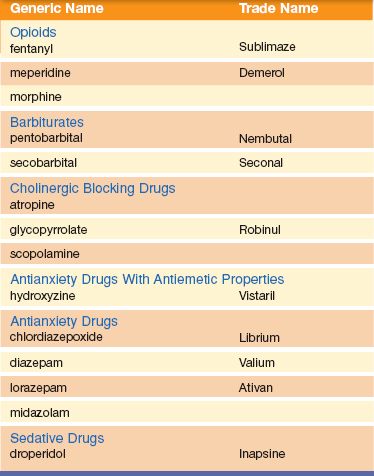
A preanesthetic drug is one given before the administration of anesthesia. These drugs are to relax or sedate the patient for the surgical procedure. They may be taken at home by the patient, given by a nurse in the preanesthesia unit, or administered right before general anesthesia. The preanesthetic agent may consist of one drug or a combination of drugs.
Uses of Preanesthetic Drugs
The general purpose, or use, of the preanesthetic drug is to prepare the patient for anesthesia. The more specific purposes of these drugs include the following:
• Opioid or antianxiety drug—to decrease anxiety and apprehension immediately before surgery. The patient who is calm and relaxed can be anesthetized more quickly, usually requires a smaller dose of an induction drug, may require less anesthesia during surgery, and may have a smoother recovery from the anesthesia period (awakening from anesthesia).
• Cholinergic blocking drug—to decrease secretions of the upper respiratory tract. Some anesthetic gases and volatile liquids are irritating to the lining of the respiratory tract and thereby increase mucous secretions. The cough and swallowing reflexes are lost during general anesthesia, and excessive secretions can pool in the lungs, resulting in pneumonia or atelectasis (lung collapse) during the postoperative period. The administration of a cholinergic blocking drug, such as glycopyrrolate (Robinul), dries up secretions of the upper respiratory tract and decreases the possibility of excessive mucus production.
• Antiemetic—to decrease the incidence of nausea and vomiting during the immediate postoperative recovery period
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Preanesthetic drugs may be omitted in patients who are 60 years or older because many of the medical disorders for which these drugs are contraindicated are seen in older individuals. For example, atropine and glycopyrrolate, drugs that can be used to decrease secretions of the upper respiratory tract, are contraindicated in certain medical disorders, such as prostatic hypertrophy, glaucoma, and myocardial ischemia. Other preanesthetic drugs that depress the CNS, such as opioids, barbiturates, and antianxiety drugs, with or without antiemetic properties, may be contraindicated in the older individual.
Selection of Preanesthetic Drugs
The preanesthetic drug is usually selected by the anesthesiologist and may consist of one or more drugs (Table 17.2). An opioid (see Chapter 16) or antianxiety drug (see Chapter 20) may be given to relax or sedate the patient. A cholinergic blocking drug (see Chapter 27) is given to dry secretions in the upper respiratory tract. Scopolamine and glycopyrrolate also have mild sedative properties, and atropine may or may not produce some sedation. Antianxiety drugs have sedative action; when combined with an opioid, they allow a lowering of the opioid dosage because they also have the ability to potentiate (increase the effect of) the sedative action of the opioid. Diazepam (Valium), an antianxiety drug, is one of the more commonly used drugs for preoperative sedation.
Table 17.2 Examples of Preanesthetic Drugs
Nursing Responsibilities
When caring for a patient receiving a preanesthetic drug, assess the patient’s physical status and give an explanation of the anesthesia. In some hospitals, the anesthesiologist examines the patient at an outpatient visit, a few days or a week before surgery, although this may not be possible in emergency situations. Some hospitals use operating room or postanesthesia care unit (PACU) staff members to visit the patient before surgery to explain certain facts, such as the time of surgery, the effects of the preanesthetic drug, preparations for surgery, and the PACU. Proper explanation of anesthesia, the surgery itself, and the events that may occur in preparation for surgery, as well as care after surgery, requires a team approach. As the nurse on the team, your responsibilities include the following:
• Describe or explain the preparations for surgery ordered by the physician. Examples of preoperative preparations include fasting from midnight (or the time specified by the physician), enema, shaving of the operative site, use of a hypnotic for sleep the night before, and the preoperative injection about 30 minutes before surgery.
• Describe or explain immediate postoperative care, such as that given in the PACU (also called the recovery room) or a special postoperative surgical unit, and the activities of the health care team during this period. Explain that the patient’s vital signs will be monitored frequently and that other equipment, such as IV lines and fluids and hemodynamic (cardiac) monitors, may be used.
• Demonstrate, describe, and explain postoperative patient activities, such as deep breathing, coughing, and leg exercises.
• Emphasize the importance of pain control, and make sure the patient understands that relieving pain early on is better than trying to hold out, not take the medicine, and later attempt to relieve the pain. Teach the patient how to use the patient-controlled analgesia (PCA) pump.
• Tailor the preoperative explanations to fit the type of surgery scheduled. Not all of these teaching points may require inclusion in every explanation.
• Provide written instructions in the language of preference for the patient to take home and read to reinforce the teachings.
GENERAL ANESTHESIA
The administration of general anesthesia requires the use of one or more drugs. The choice of anesthetic drug depends on many factors, including:
• General physical condition of the patient
• Area, organ, or system being operated on
• Anticipated length of the surgical procedure
The anesthesiologist selects the anesthetic drugs that will produce safe anesthesia, analgesia (absence of pain), and, in some surgeries, effective skeletal muscle relaxation. General anesthesia is most commonly achieved when the anesthetic vapors are inhaled or administered IV. Volatile liquid anesthetics produce anesthesia when their vapors are inhaled. Volatile liquids are liquids that evaporate on exposure to air. Examples of volatile liquids include halothane, desflurane, and enflurane. Gas anesthetics are combined with oxygen and administered by inhalation. Examples of gas anesthetics are nitrous oxide and cyclopropane.
Drugs Used for General Anesthesia
Barbiturates and Similar Agents
Methohexital (Brevital), which is an ultrashort-acting barbiturate, is used for the following:
• Induction of anesthesia
• Short surgical procedures with minimal painful stimuli
• In conjunction with or as a supplement to other anesthetics
These types of drugs have a rapid onset and a short duration of action. They depress the CNS to produce hypnosis and anesthesia but do not produce analgesia. Recovery after a small dose is rapid.
Etomidate, a nonbarbiturate, is used for induction of anesthesia. Etomidate also may be used to supplement other anesthetics, such as nitrous oxide, for short surgical procedures. It is a hypnotic without analgesic activity.
Propofol (Diprivan) is used for induction and maintenance of anesthesia. It also may be used for sedation during diagnostic procedures and procedures that use a local anesthetic. This drug also is used for continuous sedation of intubated or respiratory-controlled patients in intensive care units.
Benzodiazepines
Midazolam, a short-acting benzodiazepine CNS depressant, is used as a preanesthetic drug to relieve anxiety; for induction of anesthesia; for conscious sedation before minor procedures, such as endoscopy; and to supplement nitrous oxide and oxygen for short surgical procedures. When the drug is used for induction anesthesia, the patient gradually loses consciousness over a period of 1 to 2 minutes.
Ketamine
Ketamine (Ketalar) is a rapid-acting general anesthetic. It produces an anesthetic state characterized by profound analgesia, cardiovascular and respiratory stimulation, normal or enhanced skeletal muscle tone, and occasionally mild respiratory depression. Ketamine is used for diagnostic and surgical procedures that do not require relaxation of skeletal muscles, for induction of anesthesia before the administration of other anesthetic drugs, and as a supplement to other anesthetic drugs.
Gases and Volatile Liquids
Nitrous oxide is the most commonly used anesthetic gas. It is a weak anesthetic and is usually used in combination with other anesthetic drugs. It does not cause skeletal muscle relaxation. The chief danger in the use of nitrous oxide is hypoxemia. Nitrous oxide is nonexplosive and is supplied in blue cylinders (oxygen tanks are green).
Enflurane (Ethrane) is a volatile liquid anesthetic that is delivered by inhalation. Induction and recovery from anesthesia are rapid. Muscle relaxation for abdominal surgery is adequate, but greater relaxation may be necessary and may require the use of a skeletal muscle relaxant. Enflurane may produce mild stimulation of respiratory and bronchial secretions when used alone. Hypotension may occur when anesthesia deepens.
Isoflurane (Forane) is a volatile liquid given by inhalation. It is used for induction and maintenance of anesthesia.
Desflurane (Suprane), a volatile liquid, is used for induction and maintenance of anesthesia. A special vaporizer is used to deliver this anesthetic, because delivery by mask results in irritation of the respiratory tract.
Sevoflurane (Ultane) is an inhalational analgesic. It is used for induction and maintenance of general anesthesia in adult and pediatric patients for both inpatient and outpatient surgical procedures.
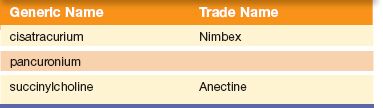
Table 17.3 Examples of Muscle Relaxants Used During General Anesthesia
Opioids
The opioid analgesic fentanyl (Sublimaze) and the neuroleptic drug (major tranquilizer) droperidol (Inapsine) may be used together. The combination of these two drugs results in neuroleptanalgesia, which is characterized by general quietness, reduced motor activity, and profound analgesia. Complete loss of consciousness may not occur unless other anesthetic drugs are used. A combination of fentanyl and droperidol may be used for the tranquilizing effect and analgesia for surgical and diagnostic procedures. It may also be used as a preanesthetic for the induction of anesthesia and in the maintenance of general anesthesia.
The use of droperidol as a tranquilizer, as an antiemetic to reduce nausea and vomiting during the immediate postanesthesia period, as an induction drug, and as an adjunct to general anesthesia has decreased because of its association with fatal cardiac dysrhythmias. Fentanyl may be used alone as a supplement to general or regional anesthesia. It may also be administered alone or with other drugs as a preoperative drug and as an analgesic during the immediate postoperative period.
Remifentanil (Ultiva) is used for induction and maintenance of general anesthesia and for continued analgesia during the immediate postoperative period. This drug is used cautiously in patients with a history of hypersensitivity to fentanyl.
Skeletal Muscle Relaxants
The various skeletal muscle relaxants that may be used during general anesthesia are listed in Table 17.3. These drugs are administered to produce relaxation of the skeletal muscles during certain types of surgeries, such as those involving the chest or abdomen. They may also be used to facilitate the insertion of an endotracheal tube. Their onset of action is usually rapid (45 seconds to a few minutes), and their duration of action is 30 minutes or more.
Stages of General Anesthesia
General surgical anesthesia is divided into the following stages:
• Stage I—analgesia
• Stage II—delirium
• Stage III—surgical analgesia
• Stage IV—respiratory paralysis
Display 17.1 describes the stages of general anesthesia more completely. With newer drugs and techniques, the stages of anesthesia may not be as prominent as those described in Display 17.1. In addition, movement through the first two stages is usually very rapid.
Display 17.1 Stages of General Anesthesia
Stage I
Induction is a part of stage I anesthesia. It begins with the administration of an anesthetic drug and lasts until consciousness is lost. With some induction drugs, such as the short-acting barbiturates, this stage may last only 5 to 10 seconds.
Stage II
Stage II is the stage of delirium and excitement. This stage is also brief. During this stage, the patient may move about and mumble incoherently. The muscles are somewhat rigid, and the patient is unconscious and cannot feel pain. During this stage, noises are exaggerated and even quiet sounds may seem extremely loud to the patient. If surgery were attempted at this stage, there would be a physical reaction to painful stimuli, yet the patient would not remember sensing pain. During these first two stages of anesthesia, you should avoid any unnecessary noise or motion in the room.
Stage III
Stage III is the stage of surgical analgesia and is divided into four parts, planes, or substages. The anesthesiologist differentiates these planes by the character of the respirations, eye movements, certain reflexes, pupil size, and other factors. The levels of the planes range from plane 1 (light) to plane 4 (deep). At plane 2 or 3, the patient is usually ready for the surgical procedure.
Stage IV
Stage IV is the stage of respiratory paralysis and is a rare and dangerous stage of anesthesia. At this stage, respiratory arrest and cessation of all vital signs may occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree