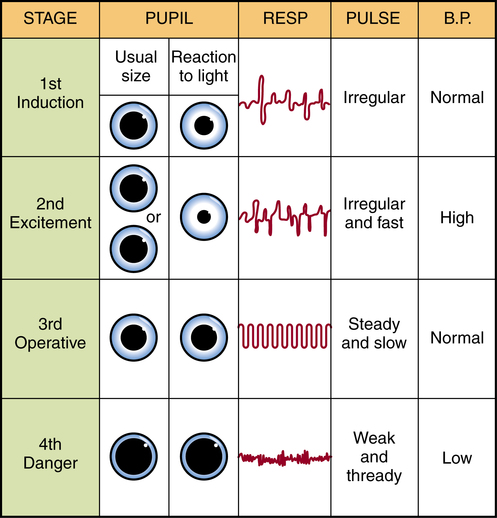
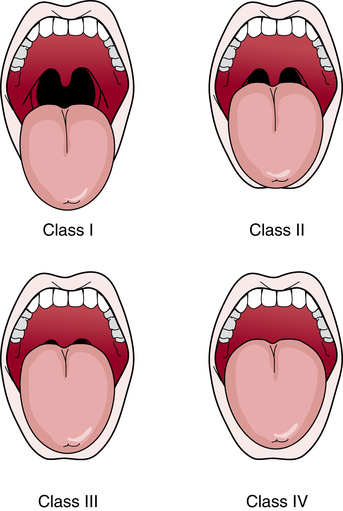
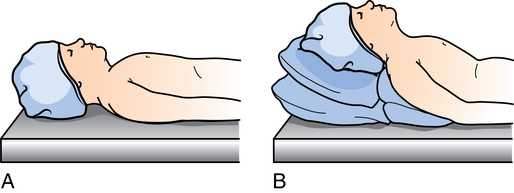
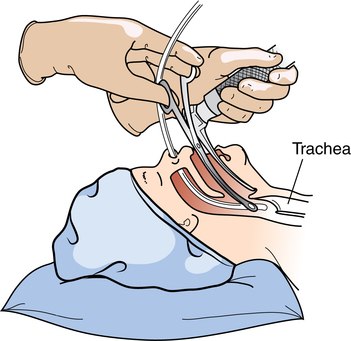
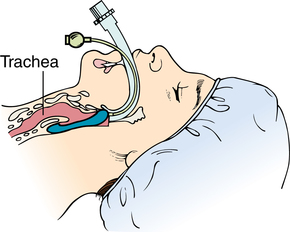
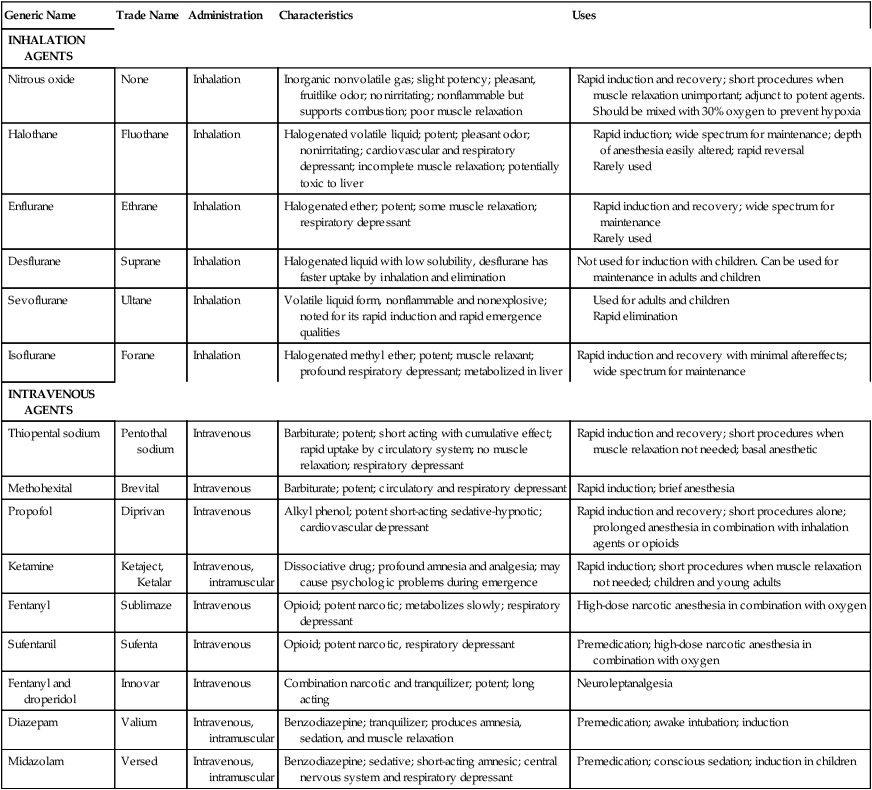
Chapter 24 After studying this chapter, the learner will be able to: • Identify three methods of general anesthesia. • Describe the physiologic effects of general anesthesia. • Discuss the purpose for cricoid pressure. • Differentiate between general and regional anesthesia. • List key points in providing safety for the anesthetized patient. The purpose of this chapter is to acquaint the surgical team with several processes associated with the delivery and maintenance of anesthesia and how the team works together to provide a safe surgical procedure for the patient. All perioperative team members should be readily available to assist the anesthesia provider as needed. Continuing education is advised for the entire team. (Internet websites included with links to educational information, such as Gas Net, http://anestit.unipa.it/HomePage.htmland The Virtual Anesthesia Machine http://vam.anest.ufl.edu, are excellent free resources.) Links on the Virtual Anesthesia Machine website offer other forms of simulated learning such as difficult airway management for a signup fee. • Provide maximum safety for the patient • Provide optimal operating conditions for the surgeon • Have a low index of toxicity • Provide potent, predictable analgesia extending into the postoperative period • Produce adequate muscle relaxation • Have a rapid onset and easy reversibility • Age, size, and weight of the patient • Physical, mental, and emotional status of the patient • Presence of complicating systemic disease or concurrent drug therapy • Presence of infection at the site of the surgical procedure • Previous anesthesia experience • Position required for the procedure • Type and expected length of the procedure • Local or systemic toxicity of the agent • Expertise of the anesthesia provider The brain represents approximately 2% of body weight but receives about 15% of cardiac output. Various factors cause alterations in cerebral blood flow and are of considerable importance in anesthesia.8 These factors are oxygen, carbon dioxide, temperature, arterial blood pressure, drugs, the age of the patient, anesthetic techniques, and neurogenic factors.8 The anesthesia state involves control of motor, sensory, mental, and reflex functions. The anesthesia provider constantly assesses the patient’s response to stimuli to evaluate specific anesthetic requirements. Specific drugs are used to achieve the desired results: amnesia, analgesia, and muscle relaxation. ASA and AANA have established guidelines and standards for safely administering and monitoring anesthesia care. ASA also developed the taxonomy for classifying patients by physical status from class I, the lowest risk, to class VI, the highest risk (Box 24-1). Being responsible for vital functions of the patient, the anesthesia provider must know physical and chemical properties of all gases and liquids used in anesthesia. These properties determine how agents are supplied, their stability, systems used for their administration, and their uptake and distribution in the body.5 Important factors are diffusion, solubility in body fluids, and relationships of pressure, volume, and temperature. The synthesized general anesthetic agents are nonflammable, in contrast with the older agents. 1. Minimal or light sedation (anxiolysis): A drug-induced state during which patients respond normally to verbal command. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected. 2. Moderate sedation/analgesia (formerly known as conscious sedation): A drug-induced depression of consciousness during which patients can respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. 3. Deep sedation/analgesia: A drug-induced depression of consciousness during which patients cannot be easily aroused but respond purposefully after repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance to maintain a patent airway, and spontaneous ventilation may be inadequate.5 4. Full anesthesia: General anesthesia and regional anesthesia. General anesthesia is a drug-induced loss of consciousness during which patients cannot be roused, even by painful stimulation. The ability to independently maintain ventilatory function is often impaired. Patients often require assistance to maintain a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function. Cardiovascular function may be impaired. Anesthesia may be produced in a number of ways: • General anesthesia: Pain is controlled by general insensibility. Basic elements include loss of consciousness, analgesia, interference with undesirable reflexes, and muscle relaxation. • Balanced anesthesia: The properties of general anesthesia (i.e., hypnosis, analgesia, and muscle relaxation) are produced, in varying degrees, by a combination of agents. Each agent has a specific purpose. This often is referred to as neuroleptanesthesia. • Local or regional block anesthesia: Pain is controlled without loss of consciousness. The sensory nerves in one area or region of the body are anesthetized. This is sometimes called conduction anesthesia. Acupuncture is sometimes used. • Spinal or epidural anesthesia: Sensation of pain is blocked at a level below the diaphragm without loss of consciousness. The agent is injected in the spinal canal. Most anesthetic agents are potentially lethal. The anesthesia provider must constantly observe the body’s reflex responses to stimuli and other guides to determine the degree of CNS, respiratory, and circulatory depression during induction and the surgical procedure. No one clinical sign can be used as a reliable indication of anesthesia depth. Continuous watching and appraisal of all clinical signs, in addition to other available objective measurements, are necessary. In this way the anesthesia provider judges the level of anesthesia, referred to as light, moderate, or deep, and provides the patient with optimal care (Table 24-1). TABLE 24-1 Induction involves putting the patient safely into a state of unconsciousness. Figure 24-1 depicts the levels of unconsciousness associated with general anesthesia. A patent airway and adequate ventilation must be ensured. If one is not already running, an intravenous (IV) infusion is started. The anesthesia provider should wear gloves for venipuncture. A nasogastric tube may be inserted to decompress the gastrointestinal tract and evacuate stomach contents. A patent airway must be established to provide adequate oxygenation and control breathing of the unconscious patient. The patient’s tongue and secretions can obstruct respiration in the absence of protective reflexes. The anesthesia provider evaluates the airway for the risk of difficult intubation using the Mallampati classification chart (Fig. 24-2). Other measurements include thyromental distance, neck flexion/extension range, and the ability to prognath (protrude the mandible). An oropharyngeal airway, nasopharyngeal airway, laryngeal mask, endotracheal tube, or endobronchial tube (for lung procedures) may be inserted. Physiologic indicators of a difficult airway include the following: • Inability to open the mouth. Patients with previous jaw surgery may have jaw wires in place. Wire cutters should be immediately available in the event of a return to surgery. • Immobility of the cervical spine. Patients with vertebral disease or injury may not have full range of motion necessary for intubation. • Chin or jaw deformities. Patients with small jaws or chin may have a difficult airway. Edentulous patients commonly have some bone loss that alters facial contours. • Dentition can be an issue if the patient has loose teeth or periodontal disease. A tooth can be aspirated during the airway maintenance process. Children between the ages of 6 and 8 commonly have loose baby teeth. • Short neck or morbid obesity (Fig. 24-3). • Pathology of the head and neck such as tumors or deformity. An enlarged tongue can be an obstruction to a full view of the glottis. • Previous tracheostomy scar, which can cause a stricture. Intubation is insertion of an endotracheal tube between vocal cords, usually with an oral tube by direct laryngoscopy. A nasotracheal tube may be inserted by blind intubation or with a direct approach using Magill forceps to guide the tube through the pharynx (Fig. 24-4). Epistaxis can be a complication of nasal airway use. This method is contraindicated in anticoagulated patients. Tubes may be made of metal, plastic, silicone, or rubber. Most styles for adult sizes have a built-in cuff that is inflated with a measured amount of air, water, or saline after insertion, to completely occlude the trachea. Aspiration is also a hazard, particularly in a patient with a full stomach or with increased intraabdominal or intracranial pressure. Any patient who arrives in the OR unconscious or who is a victim of trauma should be treated as though he or she has a full stomach.12 Pregnant and obese patients should also be considered in this category because of increased intraabdominal pressure in the supine position and possible decreased gastric motility. The circulating nurse may be asked to apply pressure to the cricoid cartilage to occlude the esophagus and immobilize the trachea. Referred to as the Sellick’s maneuver, this action prevents regurgitation and aspiration of stomach contents. The cricoid cartilage forms a complete ring around the inferior wall of the larynx below the thyroid cartilage prominence. Exerting pressure with one or two fingers to compress the cricoid cartilage against the body of the sixth cervical vertebra obstructs the esophagus (Fig. 24-5). Awake intubation can be performed with a fiberoptic or rigid laryngoscope for direct visualization of vocal cords after the administration of IV sedation and application of a topical spray anesthetic to the posterior pharynx.1 The anesthesia provider may inject a local anesthetic around the laryngeal nerve to suppress the patient’s gag and cough reflex. Usually two anesthesia providers work together during awake intubation. 1. The circulating nurse should remain at the patient’s side during induction to provide physical protection and emotional support, assist the anesthesia provider as needed, and closely observe the monitors. 2. Although induction is quiet and uneventful for most patients, untoward occurrences are possible. Excitement, coughing, breath holding, retching, vomiting, irregular respiratory patterns, or laryngospasm can lead to hypoxia. Secretions in air passages from irritation by the anesthetic can cause obstruction and dysrhythmias. Induction is gentle and not so rapid as to cause physiologic insult. To prevent these events, the patient must not be stimulated. (Avoid venting steam from the sterilizer in the adjacent substerile room, clattering instruments, or opening paper wrappers. Do not move or begin prepping the patient until the anesthesia provider says it is safe to do so.) 3. Precautions to be taken during induction include continuous electrocardiogram (ECG) monitoring, use of a precordial chest stethoscope, and having resuscitative equipment, including a defibrillator, readily available. 4. Induction is individualized. For example, an obese or pregnant patient may be induced with the head raised slightly to avoid pressure of the abdominal viscera against the diaphragm. The patient is placed flat, however, if the blood pressure begins to drop. 5. Small children need gentle handling. The circulating nurse can help the anesthesia provider make the induction period less frightening by staying close to the child. Sometimes a drop of artificial flavoring (e.g., orange, peppermint) put inside the facemask facilitates the child’s acceptance of it. Parents are often allowed in for induction according to the institution’s policy. After induction, the parent is escorted back to the waiting area. 6. The speed of induction depends on the potency of the agent, administration technique, partial pressure administered, and the rate at which the anesthetic is taken up by blood and tissues. 1. Oxygenation: Tissues, especially the brain, must be continuously perfused with oxygenated blood. The color of the blood, amount and kind of bleeding, and pulse oximetry are indicators of the adequacy of oxygenation. Controls on the anesthesia machine and monitors of vital functions keep the anesthesia provider aware of the patient’s condition. 2. Unconsciousness: The patient remains asleep and unaware of the environment during the surgical procedure. 3. Analgesia: The patient must be free of pain during the surgical procedure. 4. Muscle relaxation: Muscle relaxation must be constantly assessed to provide necessary amounts of drugs that cause skeletal muscles to relax. Less tissue manipulation is required when muscles are relaxed. 5. Control of autonomic reflexes: Anesthetic agents affect cardiovascular and respiratory systems. Tissue manipulations and systemic reactions to them may be altered by drugs that control the autonomic nervous system. All anesthesia machines have the following features (Fig. 24-6): 1. Sources of oxygen and compressed gases (Fig. 24-7). These may come from piped-in systems, but mounted oxygen tanks are necessary in the event of failure of systems. 2. Means for measuring (flowmeters) and controlling (reservoir bag) delivery of gases. 3. Means to volatilize liquid (vaporizer) and deliver (breathing tubes) anesthetic vapor or gas. 4. Device for disposal of carbon dioxide (carbon dioxide absorption canister). The elimination of waste gas, vented through an exhaust valve into a waste gas scavenger system, controls pollution of the room air.13 Nitrous oxide and halogenated agents can escape into room air if they are not directed through the scavenger system. Substantial amounts may be an occupational health hazard to OR team members. Prolonged exposure to high concentrations of waste gases (1000 ppm) can cause reproductive abnormalities.12 Halogenated waste gases should be lower than 2 ppm and nitrous oxide (N2O) waste gas should be lower than 25 ppm according to safety regulations set by OSHA.12 The method for administration of inhalation anesthetics through the anesthesia machine can be classified as semiclosed, closed, semiopen, or open (Fig. 24-8): • Semiclosed system: The most widely used system, a semiclosed system permits exhaled gases to pass into the atmosphere so that they will not mix with fresh gases and be rebreathed. A chemical absorber for carbon dioxide is placed in the breathing circuit. This reduces carbon dioxide accumulation in blood. Induction is slower but with less loss of heat and water vapor than with open methods. • Closed system: A closed system allows complete rebreathing of expired gases. Exhaled carbon dioxide is absorbed by soda lime or a mixture of barium and calcium hydroxide (Baralyme) in the absorber on the machine. The body’s metabolic demand for oxygen is met by adding oxygen to the inspired mixture of gases or vapors. This system provides maximal conservation of heat and moisture. It reduces the amount and therefore the cost of agents and reduces environmental contamination. • Semiopen system: With the semiopen system some exhaled gas can pass into surrounding air but some returns to the inspiratory part of the circuit for rebreathing. The degree of rebreathing is determined by the volume of flow of fresh gas. Expired carbon dioxide is not chemically absorbed. • Open system: In an open system, valves direct expired gases into the lower portion of the canister, where they are removed by vacuum. The patient inhales only the anesthetic mixture delivered by the anesthesia machine. The composition of the inspired mixture can be accurately determined. However, anesthetic gases are not confined to the breathing system. High flows of gases are necessary, because resistance to breathing varies. Water vapor and heat are lost. Inspired gases should be humidified for respiratory mucosa to function properly, especially for children and during long surgical procedures. An airway can be maintained by inserting a laryngeal mask airway (LMA) into the larynx. This flexible tube has an inflatable silicone ring and cuff. When the cuff is inflated, the mask fills the space around and behind the larynx to form a seal between the tube and the trachea.9 All types do not protect against regurgitation and aspiration. Newer types (i.e., ProSeal) have a passage for gastric tube placement which provides better protection against regurgitation. Adult and pediatric styles are available and can be useful when intubation and mask ventilation are complex.9 Reusable and disposable styles are commercially available (Fig. 24-9). The mask is selected for use by size of the patient as follows: • It ensures a patent airway and control of respiration. Secretions are easily removed from the trachea by suctioning. Positive pressure can be given immediately by pressing the reservoir bag on the machine without danger of dilating the stomach. • It protects the lungs from aspiration of blood, vomitus of gastric contents, or foreign material. • It preserves the airway regardless of the patient’s position during the surgical procedure. • It interferes minimally with the surgical field during head and neck procedures. • It helps minimize the escape of vapors or gases into the room atmosphere. • Trauma to the teeth, pharynx, vocal cords, or trachea: Postoperatively the patient may experience sore throat, hoarseness, laryngitis, and/or tracheitis. Laryngeal edema is more common in children than in adults. Ulceration of the tracheal mucosa or vocal cords may cause granuloma. • Cardiac dysrhythmias: Cardiac dysrhythmias may occur in light anesthesia or be caused by suctioning through the endotracheal tube. • Hypoxia and hypoxemia: Hypoxia is a common complication during intubation and extubation. Endotracheal tube suctioning can cause hypoxemia. • Accidental esophageal or endobronchial intubation: The latter results in ventilation of only one lung. • Aspiration of gastrointestinal contents: This is a hazard in a patient with a full stomach or a patient who has increased intraabdominal or intracranial pressure. It can also occur in a patient with intestinal obstruction who is extubated before protective reflexes return. • It provides for optimal ventilation. • It allows for selective lung deflation for thoracic procedures. • It provides access to deep regions of the thorax and upper abdomen. • It permits deliberate production of apnea to facilitate surgical manipulation below the diaphragm, ligation of deep vessels, or obtaining radiographic films. In inhalation anesthesia, the aim is to establish balance between the content of the anesthetic vapor or gas inhaled and that of body tissues. The blood and lungs function as the transport system. Anesthesia is produced by the development of an anesthetizing concentration of anesthetic in the brain. The depth of anesthesia is related to concentration and biotransformation (see Table 24-1). 1. Transfer of anesthetic from alveoli to blood: The rate of transfer is determined by the solubility of the agent in the blood, the rate of pulmonary blood flow (related to cardiac output), and the partial pressure of the anesthetic in arterial and mixed venous blood. 2. Transfer of anesthetic from blood to tissues: Factors influencing uptake by individual tissues are similar to those for uptake by blood. They are the solubility of the gas in tissues, the tissue volume relative to the blood flow (flow rate), and the partial pressure of the anesthetic in arterial blood and tissues. Tissues differ; thus uptake of the anesthetic differs. Highly perfused tissues (heart) equilibrate more rapidly with arterial tension than does poorly perfused tissue (fat), which has a slow rise to equilibrium and retains anesthetic longer. The most important factors influencing safe administration of any anesthetic are the knowledge and skill of the anesthesia provider. A perfect agent has not been found, and no agent is entirely safe. Commonly used agents are listed in Table 24-2. Advantages and disadvantages are relative. TABLE 24-2 Most Commonly Used General Anesthetic Agents Because its metabolites have a possible effect as a hepatotoxin, some anesthesia providers avoid repeated administration within an arbitrary time (e.g., 3 months) in adults. Recent jaundice and known or suspected liver disease (past or present) are usually contraindications to its use. It is a trigger and contraindicated in patients who are susceptible to malignant hyperthermia. Malignant hyperthermia is covered in depth in Chapter 31. Isoflurane is used for induction and maintenance in a wide spectrum of procedures except routine obstetrics. Isoflurane produces uterine relaxation. Safety to the mother and fetus has not been established.10 Because the drug is metabolized in the liver, it may be given to patients with minimal renal disease. Oxygen is always given during IV and inhalation anesthesia. A barbiturate, dissociative agent, or narcotic may be given (see Table 24-2). Each has advantages, disadvantages, and contraindications. They may be supplemented with other drugs.
Anesthesia: techniques and agents
The art and science of anesthesia
Choice of anesthesia
Anesthesia state
Knowledge of anesthetics
Types of anesthesia
General anesthesia
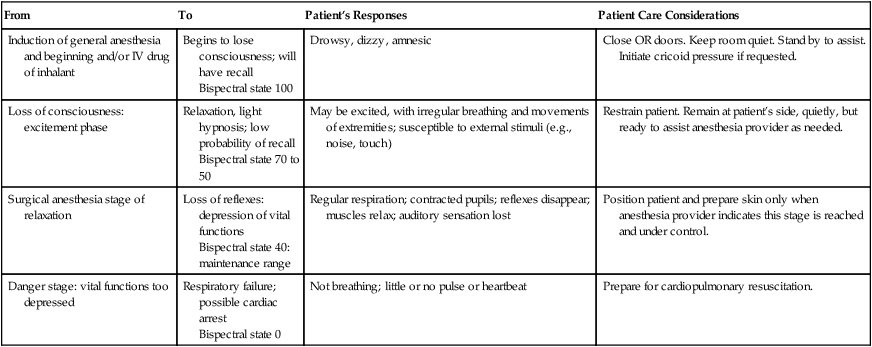
From
To
Patient’s Responses
Patient Care Considerations
Induction of general anesthesia and beginning and/or IV drug of inhalant
Begins to lose consciousness; will have recall
Bispectral state 100
Drowsy, dizzy, amnesic
Close OR doors. Keep room quiet. Stand by to assist. Initiate cricoid pressure if requested.
Loss of consciousness: excitement phase
Relaxation, light hypnosis; low probability of recall
Bispectral state 70 to 50
May be excited, with irregular breathing and movements of extremities; susceptible to external stimuli (e.g., noise, touch)
Restrain patient. Remain at patient’s side, quietly, but ready to assist anesthesia provider as needed.
Surgical anesthesia stage of relaxation
Loss of reflexes: depression of vital functions
Bispectral state 40: maintenance range
Regular respiration; contracted pupils; reflexes disappear; muscles relax; auditory sensation lost
Position patient and prepare skin only when anesthesia provider indicates this stage is reached and under control.
Danger stage: vital functions too depressed
Respiratory failure; possible cardiac arrest
Bispectral state 0
Not breathing; little or no pulse or heartbeat
Prepare for cardiopulmonary resuscitation.
Induction of general anesthesia
Intubation.
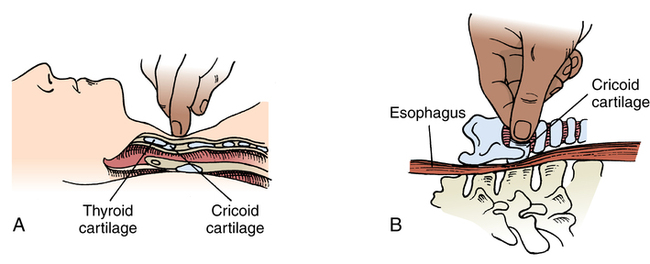
Cricoid pressure.
Awake intubation.
Key points during induction.
Maintenance of general anesthesia
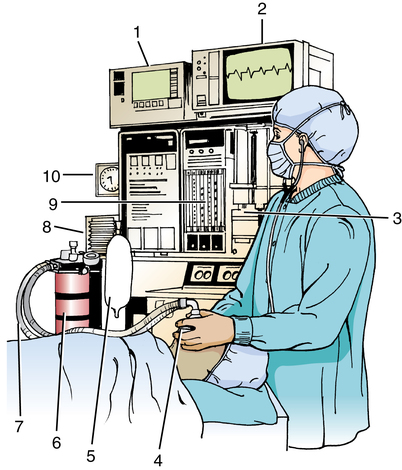
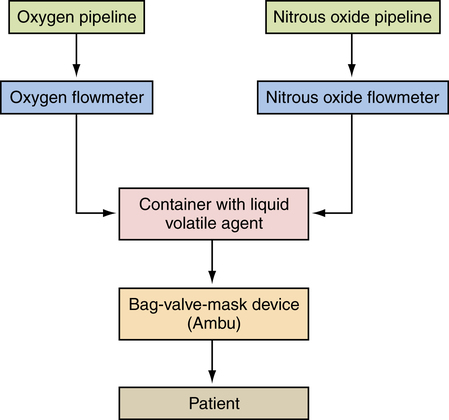
Anesthesia machine.
Waste gases.
Inhalation systems.
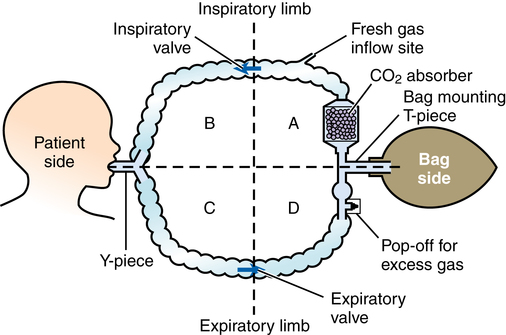
Administration techniques.
Controlled respiration.
Inhalation anesthetic agents
Generic Name
Trade Name
Administration
Characteristics
Uses
INHALATION AGENTS
Nitrous oxide
None
Inhalation
Inorganic nonvolatile gas; slight potency; pleasant, fruitlike odor; nonirritating; nonflammable but supports combustion; poor muscle relaxation
Rapid induction and recovery; short procedures when muscle relaxation unimportant; adjunct to potent agents. Should be mixed with 30% oxygen to prevent hypoxia
Halothane
Fluothane
Inhalation
Halogenated volatile liquid; potent; pleasant odor; nonirritating; cardiovascular and respiratory depressant; incomplete muscle relaxation; potentially toxic to liver
Enflurane
Ethrane
Inhalation
Halogenated ether; potent; some muscle relaxation; respiratory depressant
Desflurane
Suprane
Inhalation
Halogenated liquid with low solubility, desflurane has faster uptake by inhalation and elimination
Not used for induction with children. Can be used for maintenance in adults and children
Sevoflurane
Ultane
Inhalation
Volatile liquid form, nonflammable and nonexplosive; noted for its rapid induction and rapid emergence qualities
Isoflurane
Forane
Inhalation
Halogenated methyl ether; potent; muscle relaxant; profound respiratory depressant; metabolized in liver
Rapid induction and recovery with minimal aftereffects; wide spectrum for maintenance
INTRAVENOUS AGENTS
Thiopental sodium
Pentothal sodium
Intravenous
Barbiturate; potent; short acting with cumulative effect; rapid uptake by circulatory system; no muscle relaxation; respiratory depressant
Rapid induction and recovery; short procedures when muscle relaxation not needed; basal anesthetic
Methohexital
Brevital
Intravenous
Barbiturate; potent; circulatory and respiratory depressant
Rapid induction; brief anesthesia
Propofol
Diprivan
Intravenous
Alkyl phenol; potent short-acting sedative-hypnotic; cardiovascular depressant
Rapid induction and recovery; short procedures alone; prolonged anesthesia in combination with inhalation agents or opioids
Ketamine
Ketaject, Ketalar
Intravenous, intramuscular
Dissociative drug; profound amnesia and analgesia; may cause psychologic problems during emergence
Rapid induction; short procedures when muscle relaxation not needed; children and young adults
Fentanyl
Sublimaze
Intravenous
Opioid; potent narcotic; metabolizes slowly; respiratory depressant
High-dose narcotic anesthesia in combination with oxygen
Sufentanil
Sufenta
Intravenous
Opioid; potent narcotic, respiratory depressant
Premedication; high-dose narcotic anesthesia in combination with oxygen
Fentanyl and droperidol
Innovar
Intravenous
Combination narcotic and tranquilizer; potent; long acting
Neuroleptanalgesia
Diazepam
Valium
Intravenous, intramuscular
Benzodiazepine; tranquilizer; produces amnesia, sedation, and muscle relaxation
Premedication; awake intubation; induction
Midazolam
Versed
Intravenous, intramuscular
Benzodiazepine; sedative; short-acting amnesic; central nervous system and respiratory depressant
Premedication; conscious sedation; induction in children
Halothane (fluothane).
Isoflurane (forane).
Intravenous anesthetic agents

 Website
Website