Alterations in Function of the Gallbladder and Exocrine Pancreas
Jeffrey S. Sartin
Key Questions
• How is bile produced, stored, and secreted?
• How is pancreatic enzyme secretion regulated?
• What factors predispose to formation of cholesterol gallstones?
• What is the relationship between cholecystitis and cholelithiasis?
• What clinical and laboratory findings are indicative of acute pancreatitis?
• What serious complications may result from acute pancreatitis?
• What are the signs, symptoms, and treatment for pancreatic cancer?
![]()
http://evolve.elsevier.com/Copstead/
Stones have been discovered in the gallbladders of Egyptian and Chinese mummies, suggesting that gallbladder disease has been present in humans for thousands of years. More than 700,000 operations to remove the gallbladder (cholecystectomy) are performed annually in the United States, and the incidence of new gallstones is 1 million to 2 million cases per year.1,2 The incidence of acute pancreatitis varies according to geographic area but has been reported to range from 5 to 24 per 100,000 population in the United States and Europe.1 Many health care professionals will encounter diseases of the pancreaticobiliary system frequently and need an in-depth understanding of the mechanisms that promote them. This chapter describes the pathophysiology of diseases of the gallbladder, the biliary tree, and the exocrine pancreas, and summarizes current treatments. Cancers of the pancreas and biliary tree will be discussed briefly.
Structure and Function of the Pancreaticobiliary System
The pancreaticobiliary system is composed of the gallbladder and cystic duct; the intrahepatic, hepatic, and common bile ducts; and the endocrine and exocrine pancreas. The extrahepatic biliary tree and the gallbladder form a controlled system for delivering bile to the intestinal tract. (For additional background, refer to Chapter 35, which describes the physiology of digestion in the gastrointestinal lumen.)
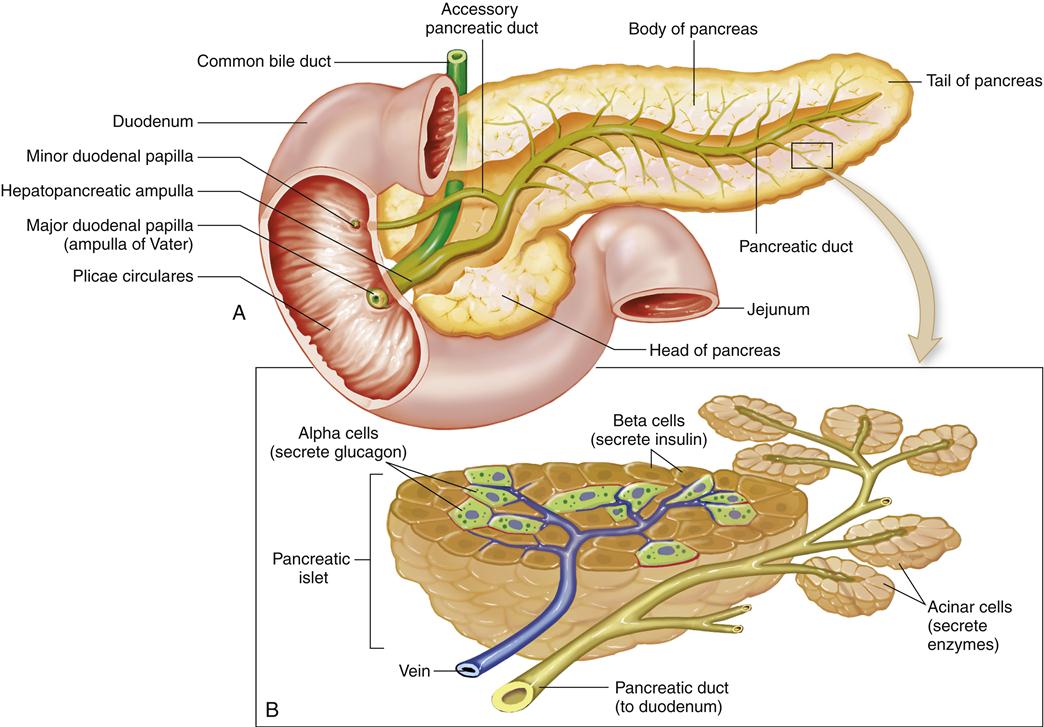
The gallbladder is a distensible sack of about 30- to 50-ml capacity that connects via the cystic duct with the common hepatic duct to form the common bile duct. The common bile duct, which is about 3 inches long, extends behind the duodenum to terminate at the ampulla of Vater, a complex structure that also forms the terminating point of the main pancreatic duct. The pancreatic duct travels proximally in the pancreas and branches off dorsally to drain the tail of the pancreas. Thus, the ampulla of Vater forms the major aqueduct through which important digestive secretions enter the intestinal tract (Figure 37-1).
Embryology of the Pancreaticobiliary System
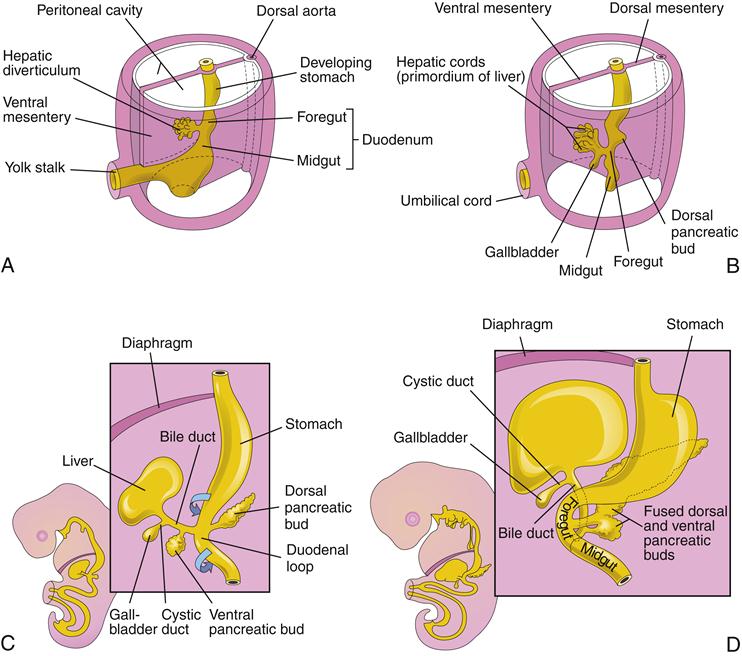
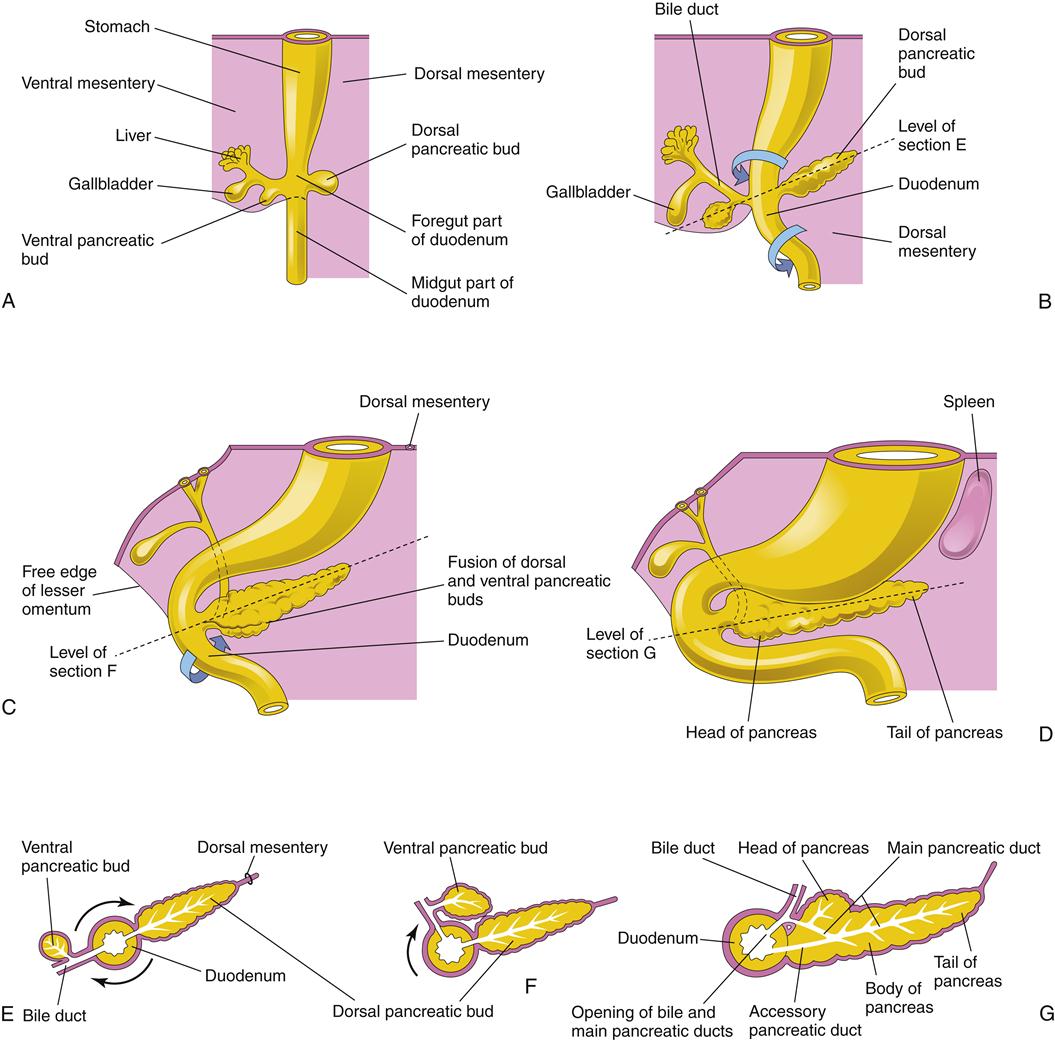
In about the third or fourth week of gestation, the hepatic diverticulum forms from the primitive foregut.3,4 It is composed of specialized progenitor liver cells that will eventually develop into the entire liver, biliary tree, and ventral pancreas. The dorsal pancreas forms from a separate outcropping of cells lying on the opposite side of the primitive foregut.
At 5 weeks of gestation, three buds can be seen in the hepatic diverticulum. The cranial bud contains specialized liver cells (hepatoblasts), which will form the liver. The liver sinusoids develop and feed into the developing bile canaliculi, which drain into intralobular ductules and then into interlobular ducts. The caudal bud develops into the gallbladder, which joins the common hepatic duct via the developing cystic duct to form the common bile duct. The gallbladder and the hepatic ducts are initially hollow, but they solidify with development and become solid cords. With further differentiation, they become hollow once again to become the tubes and reservoir for bile flow. During the second trimester, the fetus produces bile, which gives color to the fetal meconium. Finally, the basal bud transforms into the ventral pancreas (Figure 37-2).3,4
Physiology of Bile
Normal bile is composed primarily of water, electrolytes, and organic solutes. It has a low protein content, containing mainly bile acids, pigment, cholesterol, and phospholipids.1 Bile acids consist mostly of primary bile salts (cholic and chenodeoxycholic acids) and secondary bile salts (deoxycholic, ursodeoxycholic, and lithocholic acids). Bile is formed in the liver and then modified and stored in the gallbladder and bile ducts before secretion into the intestinal tract. The major functions of bile are to aid in the digestion of lipids in the diet and to transport waste products (particularly bilirubin), immunoglobulins (IgA), toxins, and cholesterol into the intestine for eventual disposal or reabsorption. After secretion into the bile canaliculi, bile flows through the canals of Hering, ductules, interlobular ducts, septal ducts, and right and left lobar ducts, and into the common bile duct (see Figure 37-1).5
The principal function of the gallbladder is the concentration and storage of bile. During the fasting state, the muscular sphincter at the ampulla of Vater is contracted, promoting flow of bile into the gallbladder. Only about half of the bile is stored during this time; the remainder flows into the duodenum. At the same time that bile is moving into the gallbladder, absorption is also occurring so that within 4 hours up to 90% of water in bile can be removed, leaving a very concentrated mixture of sodium, bile salts, and other electrolytes.5
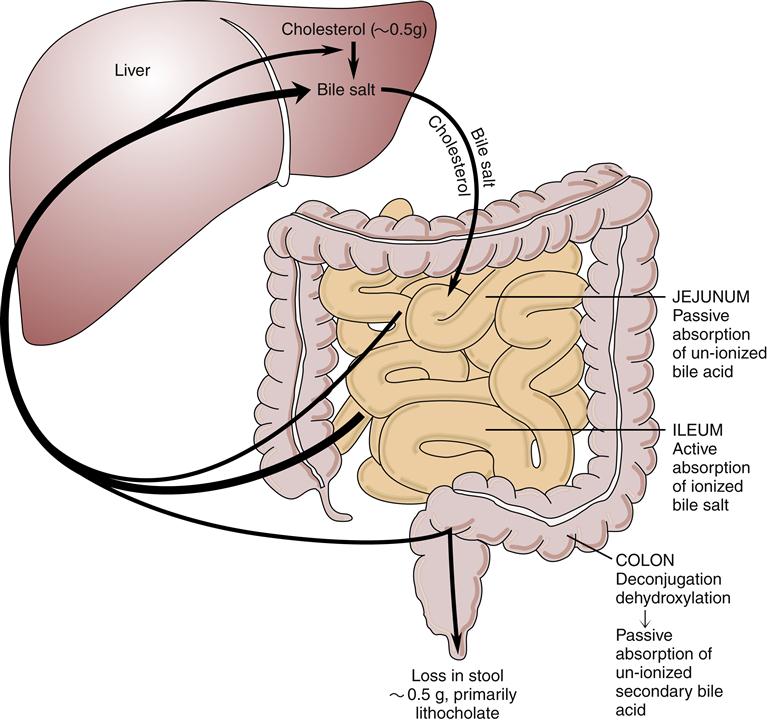
With the first morning meal, a hormonally and neurally regulated contraction of the gallbladder occurs, releasing the concentrated bile into the duodenum. Bile acids eventually will be absorbed again in the terminal ileum and travel by the portal circulation to be secreted again into the bile. (Bile acids are reabsorbed on average two or three times daily.) A small amount of the bile acid pool (less than 5%) enters the colon, where primary bile salts undergo bacterial transformation into secondary bile salts (Figure 37-3).6
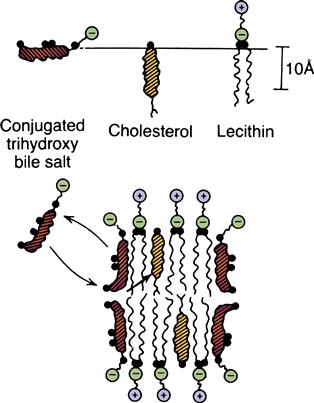
After secretion into the bile, bile salts have dual properties, being hydrophilic (soluble in water) at one end and hydrophobic (insoluble in water) at the other. Thus, these molecules tend to aggregate into clusters called micelles, which surround lipids such as cholesterol and allow them to solubilize (Figure 37-4). Micelles are not good stabilizers of cholesterol alone, but another molecule, lecithin, also secreted in large amounts in the bile, is readily incorporated in the core of the micelle to greatly enhance the solubility of cholesterol. In this way, bile keeps cholesterol partly solubilized. Precipitation of cholesterol from bile occurs at high concentrations, predisposing to formation of gallstones.6
Functional Anatomy of the Pancreas
The pancreas is really two organs in one: it functions as both an endocrine and an exocrine organ. On the one hand, hormones such as insulin, glucagon, and somatostatin are produced and secreted into the vascular system (characteristic of an endocrine organ). On the other hand, every 24 hours the pancreas secretes more than 1 L of digestive juice into the digestive tract (characteristic of an exocrine organ).5
Embryologically, the pancreas is composed of two fused organs: a dorsal and a ventral pancreas (Figure 37-5). Microscopically, the pancreas is somewhat lobular and arranged into exocrine glands. The pancreatic juices are secreted into the glandular acini, which eventually drain into the main pancreatic duct and then enter the intestinal tract. The juices themselves are composed of both active digestive enzymes (e.g., amylase, lipase) and precursor or proenzymes (e.g., trypsinogen). Their release during a meal is controlled by hormones secreted from the small intestinal mucosa: cholecystokinin (CCK) and secretin. When this regulation is deranged, enzymes may be released within the gland and produce acute pancreatitis.
Disorders of the Gallbladder
Pathophysiology of Cholesterol Gallstone Formation
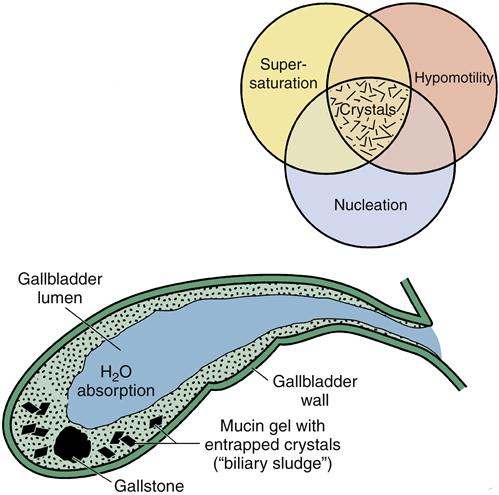
The majority of gallstones among patients in the United States are cholesterol stones.1 In general, the formation of cholesterol stones in the gallbladder (cholelithiasis) can be broken down into three phases: (1) supersaturation of bile with cholesterol; (2) nucleation of crystals; and (3) hypomotility allowing stone growth (Figure 37-6).
As described previously, cholesterol eventually precipitates from supersaturated bile. If conditions are right for the formation of cholesterol gallstones, nucleation occurs in which the cholesterol crystals aggregate together. Continued growth of the crystals then depends upon the balance between cholesterol growth–promoting factors and factors that tend to cause stone dissolution. A significant factor that promotes the continued growth of stones is hypomotility or stasis of bile within the gallbladder. Patients with high spinal cord injuries, patients receiving total parenteral nutrition, and persons who undergo prolonged fasting or rapid weight loss have impaired emptying and are at particular risk for development of cholesterol gallstones. Other risk factors for cholelithiasis include pregnancy, oral contraceptives, obesity, diabetes mellitus, and octreotide (somatostatin analogue) therapy.1
About 25% of gallstones in Western countries are due to pigment stones, which contain a mixture of pigment polymers and calcium salts. “Black” pigment stones are most common and may be idiopathic or associated with cirrhosis or hemolysis. “Brown” pigment stones differ in their composition and are much more common in developing countries, where they are associated with biliary parasitosis and bacterial colonization and infection.1
Cholelithiasis and Cholecystitis
Currently, about 20 million people in the United States have gallstones (cholelithiasis). The incidence of gallstones is related to age, gender, and a variety of medical factors. Gallstones are twice as common in women as in men. Native Americans, particularly the Pima Indians of North America, are markedly susceptible to gallstones, and American Caucasians somewhat less so. European Caucasians are intermediate in prevalence, and persons of Asian descent are at the lowest risk. Obesity correlates with the development of gallstones, but so does rapid weight loss in an obese individual. However, the presence of gallstones does not necessarily mean that an individual will have any symptoms. In many individuals, gallstones are completely asymptomatic and require no treatment. Cholelithiasis in children is usually associated with an underlying systemic disease such as cystic fibrosis or sickle cell disease. It is often symptomatic and requires treatment by gallbladder removal.
The term cholecystitis refers to inflammation of the gallbladder wall. The continued presence of gallstones in the gallbladder ultimately promotes inflammatory changes in the gallbladder wall, with fibrosis and thickening.7 Cholecystitis is classified as acute or chronic, according to its clinical manifestations. The clinical manifestations of each are described, followed by diagnostic and treatment methods.
Chronic Cholelithiasis
Clinical manifestations
The chief complication of chronic cholelithiasis is intermittent biliary colic, a persistent epigastric or right upper abdominal pain. Often the pain radiates to the back and is accompanied by nausea, vomiting, sweating, and flatus. A typical episode lasts several hours. Biliary colic is typically caused by periodic obstruction of the cystic duct by a gallstone (Figure 37-7), although rarely spasm of the sphincter of Oddi may be etiologic.
Symptoms may be precipitated by a meal, but they often occur spontaneously and may manifest at night. The pain often increases steadily for 15 minutes and persists for 1 hour or more, and then slowly decreases. Attacks may recur on a frequent or infrequent schedule. Patients often describe additional symptoms, including fatty food intolerance, belching, flatus, bloating, and epigastric burning.1,7
Diagnosis and treatment
The diagnosis of chronic cholelithiasis depends on imaging studies, particularly ultrasonography, and is essentially the same as that described for acute cholecystitis.
In cases of chronic cholelithiasis with no or very few recurrent symptoms, “watchful waiting” may be considered.1,7 However, patients with significant recurrences of biliary colic are candidates for one of the three current modes of treatment for cholecystitis: cholecystectomy (surgical removal of the gallbladder), chemical dissolution of gallstones, or lithotripsy (mechanical breaking up of gallstones within the gallbladder). These will be discussed in more detail in the Acute Cholecystitis section.
Acute Cholecystitis
Clinical manifestations
Acute cholecystitis is defined as acute inflammation of the gallbladder wall. It is characterized by severe right upper abdominal pain that may radiate to the back. Abdominal tenderness and fever are often present. Cholelithiasis is present in about 90% of patients. Obstruction of the cystic duct occurs in almost all cases, suggesting that stasis of bile in the gallbladder is important in the pathogenesis of the disease. Bacterial infection commonly accompanies acute cholecystitis, although it is not thought to be the direct cause of the inflammatory process. Laboratory evaluation may reveal leukocytosis, mild elevations in the levels of bilirubin and serum transaminases, and, less often, elevated amylase levels.7
If left untreated, the inflammatory process often escalates, and gangrene of the gallbladder wall with rupture may occur. This can lead to peritonitis and septic shock, a localized abscess (empyema), or a cholecystoenteric fistula (fistula between the gallbladder and gastrointestinal tract).
Acalculous cholecystitis is an important subgroup of acute cholecystitis. As the name implies, it occurs in patients without preexisting gallstones. It tends to occur in the setting of major surgery, critical illness, trauma, or burn-related injury. Patients tend to be predominantly male and older than 50 years, and total parenteral nutrition (TPN) is a common cofactor. It carries a somewhat more serious implication than stone-associated cholecystitis, in part because of the associated medical conditions. In fact, gangrene of the gallbladder wall and perforation, emphysematous cholecystitis, and empyema all develop more rapidly than in calculous cholecystitis.1
Diagnosis
Evaluation for possible cholecystitis includes an appropriate history and physical examination, laboratory studies, and imaging studies designed to evaluate the gallbladder and biliary tree. Ultrasound of the abdomen is the procedure of choice early in the diagnostic evaluation. Typically, the ultrasound scan reveals the presence of stones, occasionally in the cystic duct, as well as thickening of the gallbladder wall and distention of the lumen. It may also point to another diagnosis of right upper quadrant pain, such as a liver neoplasm or renal lesions. The sensitivity and specificity of ultrasound for stones larger than 2 mm in diameter approach 95%.7 Sensitivity rates for acalculous cholecystitis are somewhat lower.
However, the presence of cholelithiasis and a thickened gallbladder wall may not be diagnostic, and other diagnostic tests are used on occasion. Hepatobiliary scintigraphy (or cholescintigraphy) by hydroxyiminodiacetic acid (HIDA) scanning provides a good functional assessment of gallbladder excretion, which is markedly impaired with cholecystitis. Computed tomography (CT), magnetic resonance cholangiography (MRCA), and endoscopic retrograde cholangiopancreatography (ERCP) are useful for selected cases. The latter carries a risk of perforation and pancreatitis, and so is reserved for cases requiring intervention (stent placement, biopsy, or special contrast studies).
Treatment
Treatment for cholecystitis depends on the severity of symptoms and the patient’s clinical status. Acute cholecystitis may necessitate intervention, but surgeons generally prefer to allow a “hot” gallbladder to “cool down” before performing surgery, particularly if the patient is considered a high surgical risk.7 The benefit of antibiotics for uncomplicated cholecystitis remains unclear, but broad-spectrum antibiotics are generally administered in the setting of acute cholecystitis. Percutaneous catheter drainage or endoscopic drainage with stent placement may be performed to relieve obstruction, particularly if infection is involved. If the patient’s condition precludes surgery, these may be the main treatments, and drains can be left in place indefinitely. Advanced acute cholecystitis complicated by empyema, gangrene, or emphysematous change is considered a surgical emergency.
Laparoscopic cholecystectomy was first performed in 1987 and has benefited from rapid improvements in video laparoscopy and instrumentation. Laparoscopic cholecystectomy is now the treatment of choice for symptomatic gallstones. The procedure is usually performed with four small incisions through which instruments are inserted. The gallbladder is freed either by electrosurgical or laser excision and is then withdrawn through one of the small incisions. Advantages of the laparoscopic technique include minimal scarring, less postoperative pain than after laparotomy, shortened hospital stays, and a rapid return to daily activities.7
Open cholecystectomy was first performed in the nineteenth century and remains an extremely safe operation with low morbidity and mortality. However, the length of the incision and accompanying postoperative pain render many patients immobile after the procedure. Altered anatomy or scarring from previous surgery or the presence of common bile duct stones may necessitate a traditional cholecystectomy. A laparoscopic procedure may be converted to an open one intraoperatively if necessary (e.g., upon finding a malignant tumor in the vicinity of the gallbladder). Complications of cholecystectomy (either laparoscopic or open) can include infection, inadvertent transection of the common bile duct, and the rare but debilitating syndrome of recurrent sclerosing cholangitis.
Some patients, such as elderly or debilitated persons, may be poor surgical risks and cannot undergo the stress of surgery. Nonoperative methods to manage gallstones, such as chemodissolution with a variety of bile acids or organic solvents and lithotripsy, have been tried as alternatives to surgery. Chemodissolution is the use of chemical substances, such as bile acids or organic solvents, to dissolve gallstones. Such agents as ursodeoxycholic acid (UDCA) and chenodeoxycholic acid (CDCA) are administered orally.7 However, this approach has several major drawbacks, including diarrhea in about 50% of patients and a low overall efficacy. CDCA is also quite expensive. Extracorporeal shock wave lithotripsy (ESWL), which involves the breaking up of gallstones using shock waves, is another nonsurgical approach. The objective is to fragment stones into pieces small enough to be passed through the cystic duct, or small enough to allow dissolving agents to function. ESWL is safe and relatively effective, under proper circumstances. The disadvantages include strict selection criteria (e.g., stones less than 2 cm in diameter), resulting in a low percentage of eligible patients. The gallbladder also is left in place, allowing for possible recurrence of gallstones and necessitating the concurrent use of dissolving agents such as UDCA or CDCA to prevent new stone formation.
For the most part, in the near future the management of gallstone disease is likely to remain surgical, with traditional or laparoscopic cholecystectomy being the major forms of intervention.
Chronic Cholecystitis
Clinical manifestations
Chronic cholecystitis is defined as chronic inflammation of the gallbladder wall attributable to persistent low-grade irritation from gallstones or to recurrent attacks of acute cholecystitis. Diabetes mellitus and obesity are important predisposing factors. Although many patients suffer from intermittent biliary colic or have symptomatic acute attacks, a surprising number of patients experience no symptoms.
Chronic cholecystitis may lead to many of the complications described earlier for acute cholecystitis, including biliary sepsis, as well as a specific type of scarring known as a calcified or porcelain gallbladder, which is associated with a higher risk of cancer.1
Biliary Malignancy
Cancers of the biliary system are relatively rare; in the United States it accounts for only 1 to 2 cases per 100,000 per year.8–10 Unfortunately, they tend to be asymptomatic and progress insidiously until well advanced. Chronic cholecystitis predisposes sufferers to the very uncommon gallbladder cancer, but is only a minor risk factor for cancer of the biliary tract. Primary sclerosing cholangitis is a significant risk factor, and among immigrants from endemic countries infestation with liver flukes such as Clonorchis species can lead to biliary cancer. Typical symptoms at presentation include right upper quadrant pain and jaundice associated with biliary obstruction.
Surgery for cure is a treatment option in fewer than 10% of cases. Chemotherapy and radiation therapy are indicted for palliation, and certain patients may benefit from stenting and other procedures to alleviate biliary obstruction.