17 Alimentary system
ANTERIOR ABDOMINAL WALL
Muscles of the anterior abdominal wall
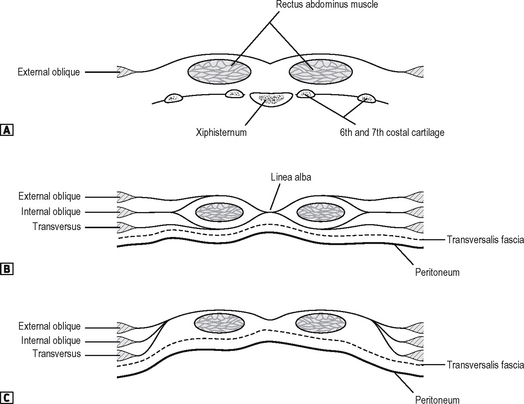
A knowledge of the anatomy of the muscles of the abdominal wall (Fig. 17.1) is a prerequisite to understanding the basis of abdominal incisions. The abdominal wall consists principally of three sheets of muscle which are fleshy laterally, and aponeurotic in front and behind. As the aponeuroses pass forward they ensheath the rectus abdominis muscle.
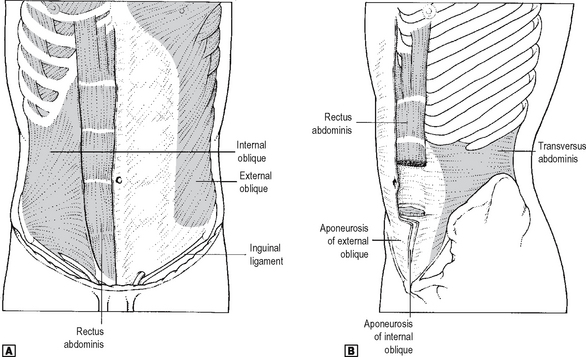
Fig. 17.1 The muscles of the anterior abdominal wall. ![]() anterior view.
anterior view. ![]() oblique view.
oblique view.
Source: Rogers A W, Textbook of anatomy; Churchill Livingstone, Edinburgh (1992).
Transversus abdominis
This arises from the deep surface of the lower six costal cartilages (interdigitating with the diaphragm), the lumbar fascia, the anterior two-thirds of the iliac crest, and the lateral third of the inguinal ligament. It is inserted into the linea alba and into the pubic crest by the conjoint tendon.
Rectus sheath
The rectus sheath (Fig. 17.2) is composed largely of the aponeuroses of the lateral abdominal muscles. It is deficient in certain areas, as follows:
ANATOMY OF ABDOMINAL INCISIONS
The anatomy of the common abdominal incisions only will be described.
Midline incision
This is made through the linea alba skirting the umbilicus. It is an excellent incision for both routine and rapid access to the peritoneal cavity, the linea alba being almost a bloodless line. Structures encountered include skin, subcutaneous fat, linea alba, extraperitoneal fat and peritoneum.
Paramedian incision
The use of this incision is declining. It is placed about 2.5 cm lateral to, and parallel to, the midline. The anterior rectus sheath is opened, the rectus displaced laterally, and the posterior sheath together with the peritoneum is incised. The anterior rectus sheath adheres to the muscle at the tendinous intersections, and the sheath requires to be dissected off at this point. Bleeding will be encountered in doing this, as the segmental vessels enter at these points. The rectus is not attached to the posterior sheath. The upper posterior rectus sheath is a thick, well-defined structure, but below a point half way between the umbilicus and pubic symphysis it is composed of transversalis fascia only and is relatively thin. The inferior epigastric vessels anastomosing with the superior epigastric vessels, may be seen posterior to the muscle and may require dividing in a lower paramedian incision.
INGUINAL CANAL
The inguinal canal (Fig. 17.3) is an oblique passage in the lower part of the abdominal wall which transmits the spermatic cord and ilio-inguinal nerve in the male, and the round ligament of the uterus and the ilio-inguinal nerve in the female. It is approximately 4 cm long and passes downwards and medially from the deep inguinal ring to the superficial inguinal ring lying above and parallel to the inguinal ligament.
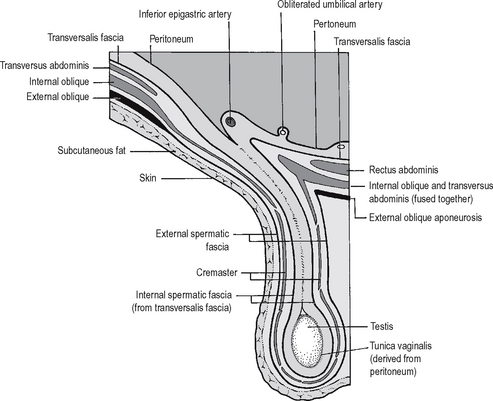
Fig. 17.3 The schematic diagram of the inguinal canal, and the coverings of the testis and spermatic cord.
Source: Rogers op. cit.
Relations
Spermatic cord
As it passes through the canal, the spermatic cord obtains three coverings: (i) the external spermatic fascia from the external oblique aponeurosis at the superficial inguinal ring; (ii) the cremasteric fascia from the internal oblique containing the cremaster muscle; (iii) the internal spermatic fascia from the transversalis fascia. The cord contains the testicular artery, the pampiniform plexus of veins, and the vas deferens. Other structures include the cremasteric artery, the artery to the vas, the nerve to cremaster, sympathetic nerve fibres and lymphatics. The ilio-inguinal nerve lies on the cord but is not part of it.
FEMORAL CANAL
PERITONEAL CAVITY
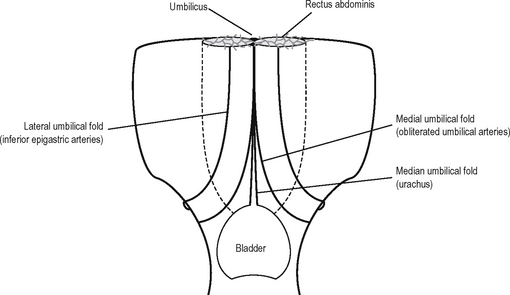
The attachments of the peritoneum are complicated. It is convenient to start at the umbilicus and work down. Below the level of the umbilicus, the parietal peritoneum is smooth apart from some folds (Fig. 17.4). These are the median umbilical fold onthe median umbilical ligament (which is due tothe obliterated urachus passing from the bladder to the umbilicus), the medial umbilical folds on the obliterated umbilical arteries, and the lateral umbilical folds which are further lateral and contain the inferior epigastric arteries. The peritoneum of the pelvis is continuous with that of the abdominal cavity. It completely encloses the sigmoid colon, forming the pelvic mesocolon. It is applied to the front and side of the upper third of the rectum and to the front only of the middle third of the rectum. It is then reflected in the male onto the base and upper part of the bladder, forming the rectovesical pouch. In the female the peritoneum is reflected from the side and front of the rectum, to the upper part of the posterior wall of the vagina and then over the posterior upper and anterior surface of the uterus to the bladder. Between the uterus and the rectum is the recto-uterine pouch (of Douglas). The peritoneum passes off the lateral margins of the uterus to the pelvic wall, forming the broad ligaments, the upper borders of which contain the uterine tubes. The free upper margins of the broad ligament lateral to the uterine tubes form the infundibulopelvic fold.
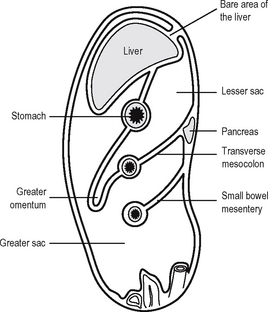
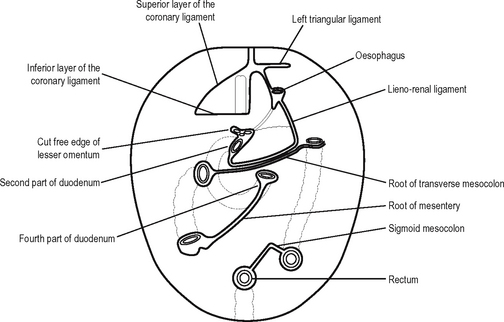
Returning to the umbilicus, the falciform ligament, the sickle-shaped fold of peritoneum, passes upwards and slightly to the right of the midline to the liver. It contains the ligamentum teres, i.e. the obliterated umbilical vein, in its free edge, and this passes into the groove between the quadrate lobe and left lobe of the liver. Traced superiorly the two layers of the falciform ligament diverge from each other, the right limb joins the upper layer of the coronary ligament while the left layer passes to the left to form the anterior layer of the left triangular ligament. Elsewhere on the anterior abdominal wall, above the umbilicus, the peritoneum sweeps upwards and over the inferior aspect of the diaphragm to be reflected onto the liver and onto the right margin of the abdominal oesophagus. Details of the peritoneal reflections of the liver are described in the section on the liver. After enclosing the liver the peritoneum descends from the porta hepatis as a double layer, i.e. the lesser omentum, and then this separates to enclose the stomach. It reforms again at the greater curve and then loops downwards, again turning upwards and attaching to the length of the transverse colon, forming the greater omentum (Fig. 17.5).
The lower leaf of the greater omentum then continues upwards, enclosing the transverse colon within the peritoneum, and then passes upwards and backwards as the transverse mesocolon, a double layer of peritoneum, to the posterior abdominal wall, where it attaches along the anterior aspect of the pancreas. At the base of the transverse mesocolon, this double layer of peritoneum divides once again, the upper leaf passing upwards over the posterior abdominal wall to reflect onto the liver, while the lower leaf passes over the lower part of the posterior abdominal wall to cover the pelvic viscera and to join with the peritoneum of the anterior abdominal wall. However, the peritoneum of the posterior abdominal wall is interrupted as it is reflected along the small bowel from the duodenal jejunal flexures to the ileocaecal junction, forming the mesentery of the small intestine. The lines of peritoneal reflection on the posterior abdominal wall are shown in Fig. 17.6.
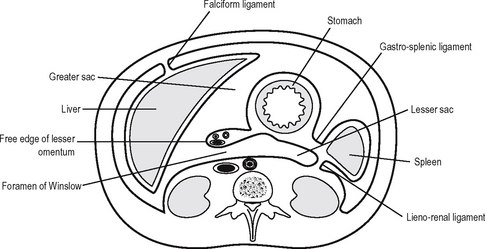
The lesser sac (Fig. 17.7) is entered via the epiploic foramen or foramen of Winslow. The lesser sac is a potential space lying behind the lesser omentum and stomach and projecting downwards to the transverse mesocolon. Superiorly is the superior recess, whose anterior border is the caudate lobe of the liver. The left wall of the lesser sac is formed by the spleen and the gastrosplenic and lienorenal ligaments. To the right the sac opens into the main peritoneal cavity via the epiploic foramen.
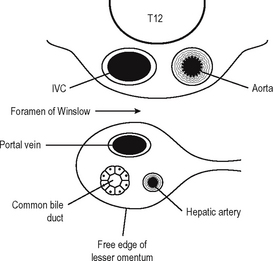
The epiploic foramen has the following boundaries (Fig. 17.8).
Subphrenic spaces
There are a number of potential spaces below the diaphragm in relation to the liver which may become the site of abscess formation (a subphrenic abscess). Abscesses may arise from such lesions as perforated peptic ulcers, perforated appendicitis, or perforated diverticulitis. Only two of the spaces are in fact directly subphrenic, the other two being subhepatic. The right and left subphrenic spaces lie between the diaphragm and the liver and are separated from one another by the falciform ligament. The right subhepatic space (pouch of Rutherford Morrison) is bounded by the posterior abdominal wall behind and by the liver above. The gall bladder, duodenum and right kidney are immediate relations. The left subhepatic space is the lesser sac itself. It may distend with fluid as a result of a perforated posterior gastric ulcer or as a result of acute pancreatitis (pseudocyst of the pancreas). At the present time most subphrenic abscesses are drained percutaneously under ultrasound control. However, the occasional one still requires open surgery and may be accessed if they are posteriorly placed by an incision below or through the bed of the twelfth rib. If they are placed anteriorly they can be drained through an incision below and parallel to the costal margin.
OESOPHAGUS
The oesophagus (Fig. 17.9) extends from the lower border of the cricoid cartilage to the cardiac orifice of the stomach. It is about 25 cm long. It has three parts: cervical, thoracic and abdominal.
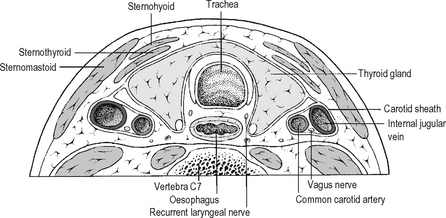
Cervical
(See Fig. 17.10.) The oesophagus passes downwards and slightly to the left. Anteriorly lie the trachea and thyroid gland. Posteriorly lie the lower cervical vertebrae and the prevertebral fascia; to the left lie the left common carotid artery, the left inferior thyroid artery, the left subclavian artery and the thoracic duct; to the right, the right common carotid artery. The recurrent laryngeal nerves lie on either side in the groove between the trachea and the oesophagus.
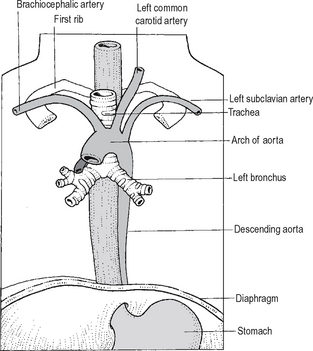
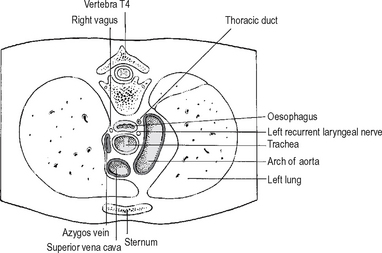
Thoracic
(See Fig. 17.11.) The oesophagus passes down through the superior and posterior mediastinum, passing initially to the right to reach the midline opposite T5. It then passes downwards, forwards, and to the left to reach the oesophageal opening in the diaphragm at T10. The two vagus nerves form a plexus on the surface of the oesophagus in the posterior mediastinum, the left nerve being anterior and the right posterior.
Anteriorly lie the left common carotid artery, the trachea, the left main bronchus which constricts it, thepericardium separating it from the left atrium andthe diaphragm. Posteriorly lie the thoracic vertebrae, the thoracic duct, the hemiazygos vein, and below, the descending aorta.
STOMACH
Relations of the stomach
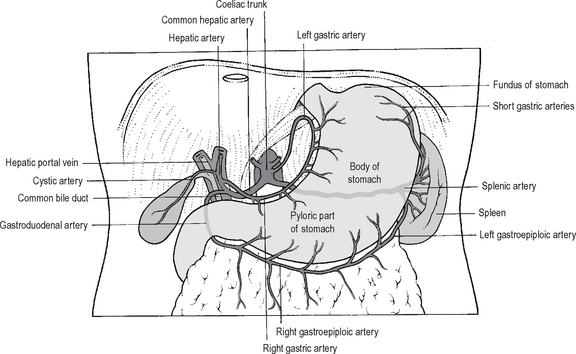
Blood supply
Blood supply (Fig. 17.12) is via:
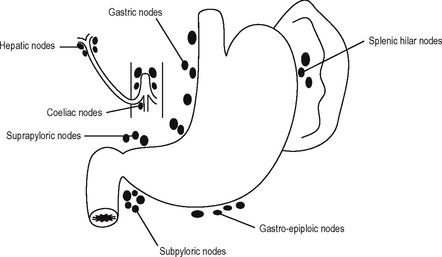
Lymphatic drainage
The arrangements of lymph nodes in relation to the stomach is shown in Fig. 17.13. The lymphatic drainage of the stomach accompanies its blood vessels. The area of the stomach supplied by the splenic artery drains via lymphatics accompanying that artery to the lymph nodes of the hilum of the spleen, then to those situated along the upper border of the pancreas and eventually to the coeliac nodes. The cardiac area of the stomach drains along the left gastric artery to reach the coeliac nodes. The remainder of the stomach drains as follows: via branches of the hepatic artery through nodes along the lesser curve to the coeliac nodes and along the right gastroepiploic vessels to the subpyloric nodes and then to the coeliac nodes. Retrograde spread may occur into the hepatic lymph nodes at the porta hepatis. Enlargements of these nodes may cause external compression of the bile ducts to produce obstruct-ive jaundice. The extensive and complex lymphatic drainage of the stomach creates problems in dealing with gastric cancer. Involvement of the nodes around the coeliac axis may render the growth incurable.
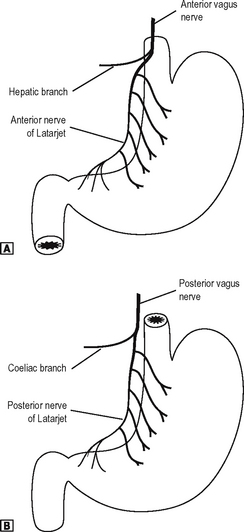
Nerve supply
The clinically important nerve supply (Fig. 17.14) of the stomach is the vagus nerves. The anterior and posterior vagus nerves enter the abdomen through the oesophageal hiatus. The anterior vagus nerve liesclose to the wall of the oesophagus and upper part of the stomach, but the posterior nerve is at a little distance from it. The anterior vagus runs caudally and supplies the anterior surface and lesser curve of the stomach. Before it reaches the stomach, it gives off a hepatic branch which passes in the lesser omentum to the liver and gall bladder and the pyloric branch to the pyloric sphincter. The posterior vagus nerve gives off a coeliac branch which passes to the coeliac plexus before sending a gastric branch to the posterior surface of the stomach. The gastric divisions of both anterior and posterior vagi reach the stomach at the cardia and descend along the lesser curve between the anterior and posterior peritoneal attachments of the lesser omentum. These nerves are referred to as the anterior and posterior nerves of Latarjet.
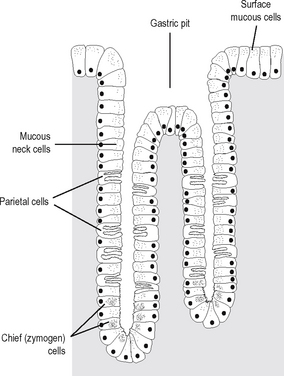
Structure of the gastric mucosa
The surface of the gastric mucosa is covered by columnar epithelial cells that secrete mucus and alkaline fluid that protects the epithelium from mechanical injury and from gastric acid. The surface of the mucosa is studded with gastric pits, each pit being the opening of a duct into which the gastric glands empty. The gastric mucosa can be divided into three areas. The cardiac gland area is the small segment located near the gastro-oesophageal junction. Histologically it contains principally mucus-secreting cells, although occasionally a few parietal (oxyntic) cells are present. The remainder of the stomach is divided into the acid-secreting region (oxyntic gland area) and the pyloric gland area. The oxyntic gland area is the portion containing the parietal (oxyntic cells) and the chief (zymogen) cells. The pyloric end area constitutes the distal 30% of the stomach and contains G cells that produce gastrin. In this region there are few oxyntic and peptic cells, mucus-secreting cells predominating. As in the rest of the gastrointestinal tract the muscular wall of the stomach is composed of an inner circular layer and an outer longitudinal layer. However, in addition there is an incomplete inner layer of obliquely situated fibres which is more prominent near the lesser curvature. Figure 17.15 shows the histological featuresof the mucosa in the oxyntic gland area. Each gastricpit drains between three and seven tubular gastric glands. The neck of the gland contains many mucus cells, oxyntic cells being most numerous in the midportion of the glands and chief cells predominating in the basal portion.
DUODENUM
Second part
This descends in a curve around the head of the pancreas. It is approximately 7.5 cm long. The bile ducts and main pancreatic ducts enter the second part of the duodenum together at the duodenal papilla on its posteromedial side. The point of entry marks the junction of the foregut and midgut. The accessory pancreatic duct (of Santorini) opens into the duodenum a little above the papilla. The second part of the duodenum is crossed by the transverse colon and lies anteriorly to the right kidney and ureter.
SMALL INTESTINE
LARGE INTESTINE
The ascending colon extends from the caecum to the undersurface of the liver where, at the hepatic flexure, it turns left to become the transverse colon. It is covered on its anterior and lateral aspect by peritoneum. Posterior relations include iliacus, quadratus lumborum, and the perirenal fascia over the lateral aspect of the kidney.
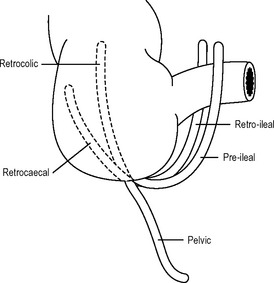
APPENDIX
The appendix is attached to the posteromedial aspect of the caecum below the ileocaecal valve. Its length varies considerably from one subject to another but usually is within the range 5–10 cm. It can be as small as 2.5 cm or as long as 25 cm. The position of the appendix is variable. In 75% of cases the appendix lies behind the caecum or colon, i.e. retrocaecal or retrocolic. In 20% of cases it hangs down into the pelvis, and in 5% of cases it is either pre-ileal or retro-ileal (Fig. 17.16). The appendix bears a mesentery containing the appendicular artery, which is a branch of the ileocolic artery. The mesentery of the appendix descends behind the ileum as a triangular fold containing the appendicular artery in its free border. The appendicular artery is functionally an end artery, and, therefore, in acute appendicitis, if it thromboses, there is a consequent rapid development of gangrene and perforation of the appendix.
RECTUM
The relations of the rectum are important in the understanding of a digital rectal examination and also in the spread of rectal cancer. Anteriorly in the male lies the rectovesical pouch, the base of the bladder, seminal vesicles and the prostate. A layer of fascia (of Denonvilliers) lies in front of the rectum, separating it from the anterior structures, and this is the plane of dissection which must be sought during abdominoperineal excision of the rectum. In the female lies the recto-uterine pouch (of Douglas) and the posterior wall of the vagina. The upper two-thirds of the rectum is covered with peritoneum anteriorly and related to coils of small bowel and the sigmoid colon in the rectovesical or recto-uterine pouch. Posteriorly lie the sacrum, coccyx and middle sacral artery. The lower sacral nerves also lie posteriorly and may be invaded by rectal cancer spreading posteriorly and resulting in sciatic pain. Laterally, below the peritoneal reflection, lie the levator ani and coccygeus.
Blood supply of the large intestine
The arterial blood supply of the large intestine is shown in Fig. 17.17. The large intestine is supplied by both branches of the superior and inferior mesenteric artery. The branches of the superior mesenteric artery are as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree