Figure 9–1 Competitive and noncompetitive blockade of epinephrine-induced aortic smooth muscle contraction by phentolamine and phenoxybenzamine. Three dose-response curves are compared. A is the curve of epinephrine alone. B is the curve of epinephrine in the presence of phentolamine. Because phentolamine is a competitive α-adrenoceptor antagonist, epinephrine can surmount its effect. C is the curve of epinephrine in the presence of phenoxybenzamine. Because phenoxybenzamine is a noncompetitive antagonist, it reduces the maximal effect of epinephrine.
PHARMACOKINETICS
When phenoxybenzamine is administered orally, it exhibits a gradual onset of action. This is because time is needed to form the active intermediate and bond covalently with α-adrenoceptors. The drug has a duration of action of 3 to 4 days because of its stable covalent bonding with α-adrenoceptors.
EFFECTS AND INDICATIONS
Phenoxybenzamine decreases vascular resistance and lowers both the supine and the standing blood pressure.
As shown in Table 9–1, phenoxybenzamine is used to treat hypertensive episodes in patients with pheochromocytoma. Because this tumor of the adrenal medulla secretes huge amounts of catecholamines, patients have extremely high blood pressure. Phenoxybenzamine has been used to control hypertension until surgery can be performed to remove the tumor (Box 9-1).
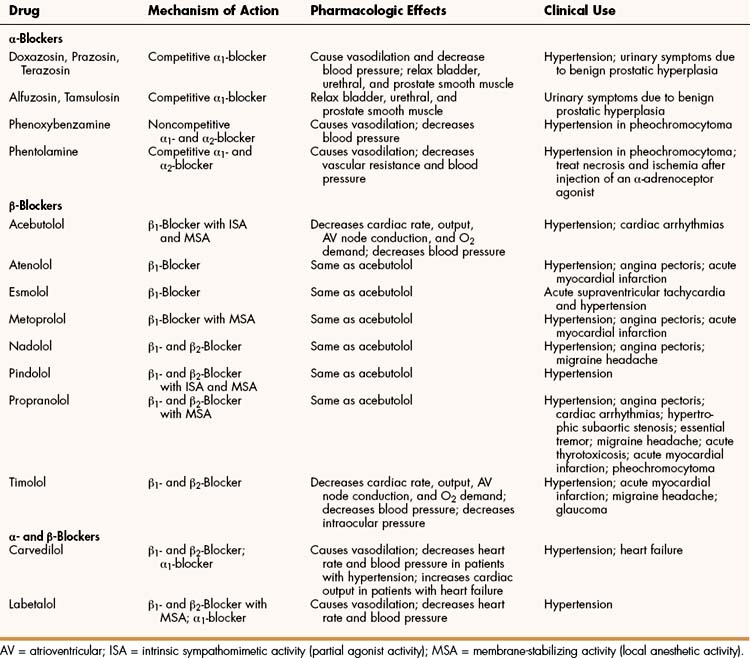
TABLE 9–1 Mechanisms, Pharmacologic Effects, and Clinical Uses of Selected Adrenoceptor Antagonists∗
BOX 9–1 A CASE OF HEADACHE, ANXIETY, AND A RACING HEART
CASE PRESENTATION:
A 38-year-old man complains of the recent onset of episodes of headache, nervousness, sweating, a racing heart, and rapid breathing. The episodes last from a few minutes to over an hour and occur several times a day. On physical examination his pulse is 86 beats/min, his respiration rate is 24/min, and his blood pressure is 210/110 mm Hg. The patient has no history of hypertension and is taking no medications. He is given oxygen and intravenous labetalol to gradually reduce heart rate and blood pressure. His 24-hour urinary vanillylmandelic acid concentration is 10.8 mg (normal <7 mg/24 h), his epinephrine is elevated at 186 μg (normal <22 μg/24 h), and norepinephrine is 135 μg (normal 12–85 μg/24 h). A computed tomography image shows a 1.7 × 2.1 cm soft tissue density in the left suprarenal area but no other abnormalities, and he is placed on metoprolol and phenoxybenzamine to control high blood pressure until surgery. His blood pressure is gradually reduced to 118/65 mm Hg, and he is started on a high-salt diet to maintain plasma volume. A week later he undergoes laparoscopic left adrenalectomy and his medications are gradually withdrawn. His blood pressure stabilizes at 120/70 mm Hg, and he is discharged after an uneventful recovery on no medication.
CASE DISCUSSION:
Pheochromocytoma is a rare tumor of the adrenal medulla that secretes huge quantities of epinephrine and norepinephrine. The peak age of onset is 40 years. Symptoms may be intermittent or continuous and include headache, anxiety, sweating, rapid breathing, and tachycardia. The diagnosis is established by abdominal imaging and measurement of urinary catecholamines and vanillylmandelic acid. If the tumor has not metastasized, it can be surgically removed with no sequelae. Blood pressure should be controlled until surgery with adrenoceptor antagonists, and phenoxybenzamine is often used for this purpose along with a β-blocker to reduce cardiac stimulation and prevent arrhythmias and cardiac ischemia. Patients are usually given a high-sodium diet (>5000 mg daily) to counteract catecholamine-induced volume contraction and the orthostatic hypotension caused by α-receptor blockade. If the tumor is unilateral, replacement of corticosteroids is not necessary after adrenalectomy.
Phentolamine
CHEMISTRY AND PHARMACOKINETICS
Phentolamine is an imidazoline compound that is structurally related to oxymetazoline and other agents in the imidazoline class of adrenoceptor agonists. After intravenous administration of phentolamine, the onset of action is immediate, and the duration of action is 10 to 15 minutes. After intramuscular or subcutaneous administration, the onset of action is 15 to 20 minutes, and the duration is 3 to 4 hours. The drug is metabolized chiefly in the liver before excretion in the urine.
MECHANISMS, EFFECTS, AND INDICATIONS
Phentolamine is a competitive adrenoceptor antagonist (see Fig. 9–1) that produces vasodilation, decreases peripheral vascular resistance, and decreases blood pressure. It is used in the treatment of hypertensive episodes caused by α-adrenoceptor agonists. In addition, it is used to treat dermal necrosis and ischemia caused by extravasation or accidental injection of epinephrine or other vasopressor amines. For example, if a patient who carries an epinephrine auto-injector for use in treating acute allergic reactions were to accidentally inject his or her finger and thereby cause ischemia, the patient could be treated by injecting phentolamine into the same site where epinephrine was injected. The phentolamine would competitively block the α-adrenoceptor stimulation and vasoconstriction produced by the epinephrine.
Phentolamine and other nonselective α-blockers are not useful in treating hypertension, partly because they evoke reflex tachycardia and cause dizziness, headache, and nasal congestion.
Selective α1-Antagonists
Agents that selectively antagonize α1-adrenoceptors include alfuzosin, doxazosin, prazosin, tamsulosin, and terazosin. Prazosin, the original drug in this class, was developed to treat hypertension. These drugs have also been used to treat urinary symptoms in men with benign prostatic hyperplasia.
General Properties
PHARMACOKINETICS
The selective α1-adrenoceptor antagonists are administered orally and undergo varying amounts of first-pass and systemic metabolism. The drugs are highly bound to plasma proteins and they are excreted in the bile, urine, and feces.
MECHANISMS, EFFECTS, AND INDICATIONS
The selective αl-blockers relax vascular and other smooth muscles, including those of the urinary bladder, urethra, and prostate. Because they produce vasodilation and decrease blood pressure, they are used to treat essential (primary) hypertension. The cardiovascular effects of α- and β-blockers in patients with hypertension are depicted in Figure 9–2.
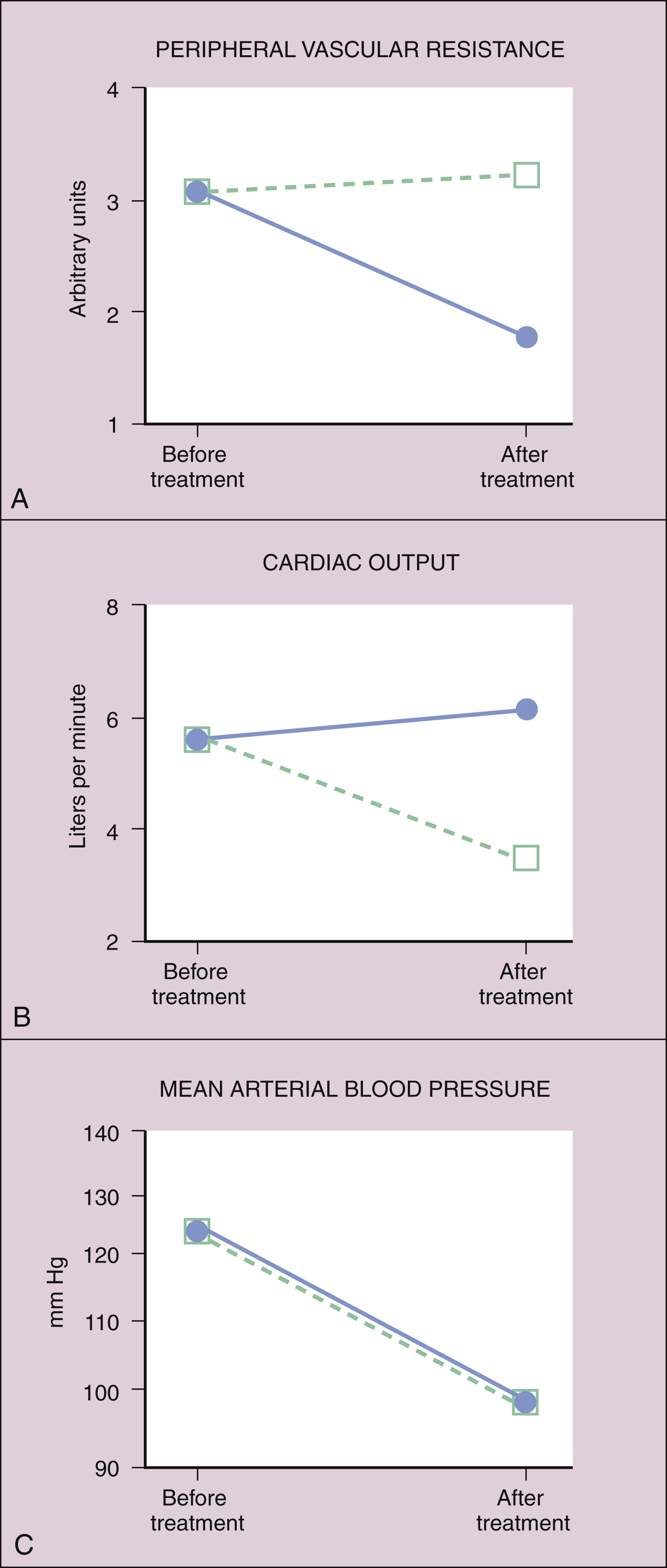
Figure 9–2 Cardiovascular effects of α1-adrenoceptor antagonists (solid line) and β1-adrenoceptor antagonists (dotted line) in patients with hypertension. (A) The α1-blockers reduce peripheral vascular resistance. The β1-blockers can cause a slight increase in peripheral vascular resistance, owing to reflex mechanisms. (B) The β1-blockers reduce cardiac output. The α1-blockers can increase cardiac output by decreasing cardiac afterload and aortic impedance to ventricular ejection of blood. (C) Both α1-blockers and β1-blockers reduce mean arterial blood pressure.
The selective α1-blockers do not cause as much reflex tachycardia as do phentolamine and other agents that nonselectively block both α1– and α2-adrenoceptors. This is because blockade of α2-adrenoceptors on sympathetic neurons prevents feedback inhibition of norepinephrine release and thereby leads to increased activation of cardiac β1-adrenoceptors and tachycardia (Fig. 9–3). The use of prazosin and other selective α1-blockers to treat hypertension is discussed in greater detail in Chapter 10.
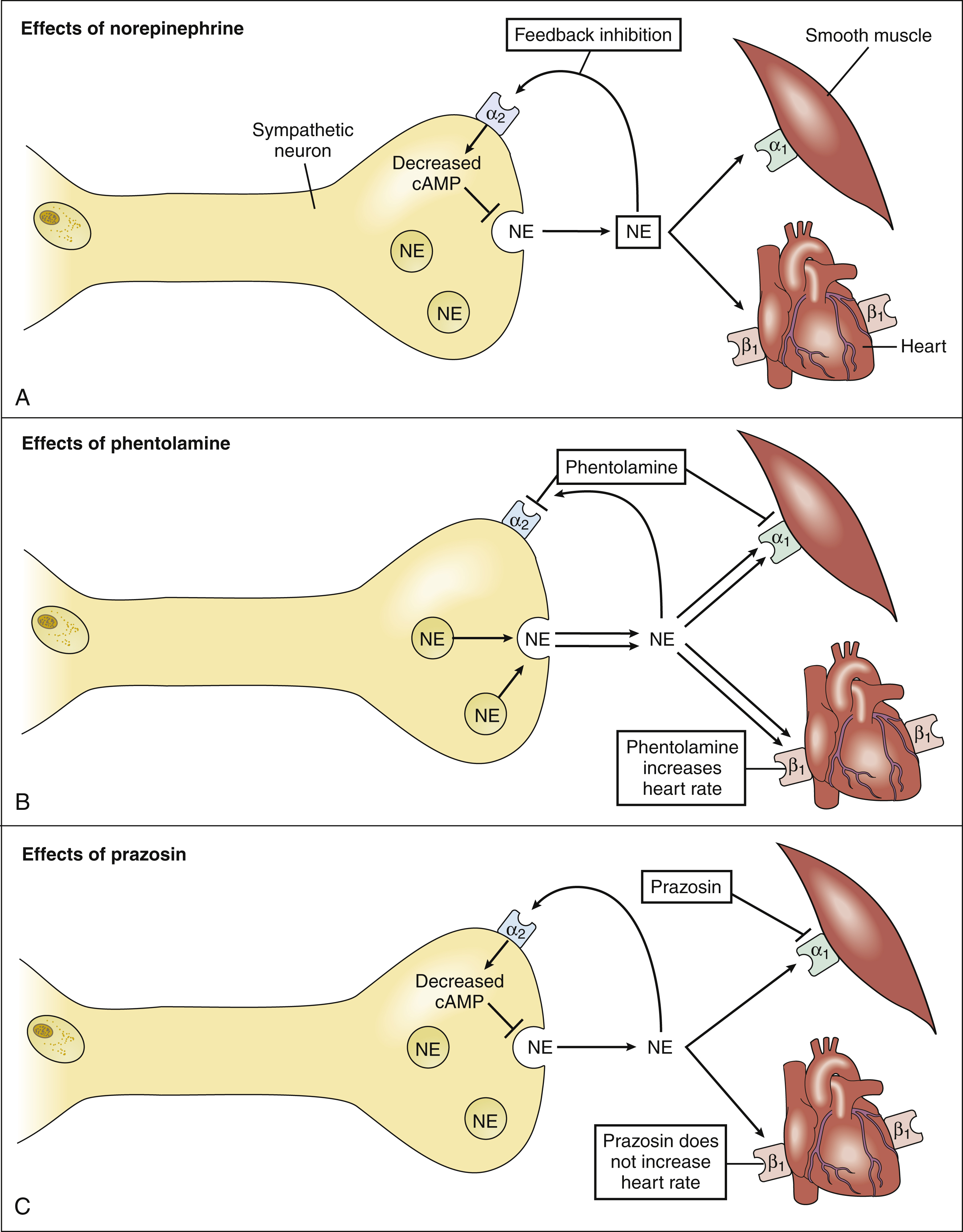
Figure 9–3 A comparison of the effects of norepinephrine, phentolamine, and prazosin on heart rate. (A) Norepinephrine (NE) activates presynaptic α2-adrenoceptors (α2), and this inhibits the formation of cyclic adenosine monophosphate (cAMP) and decreases the release of NE. (B) Phentolamine blocks α2-adrenoceptor–mediated inhibition of NE release. This increases the stimulation of cardiac β1-adrenoceptors (β1) and results in tachycardia. (C) Prazosin, a selective α1-blocker, does not block α2-adrenoceptor–mediated inhibition of norepinephrine release. Therefore, prazosin causes less tachycardia than does phentolamine. α1 = α1-adrenoceptors.
The selective α1-blockers are quite useful in treating lower urinary tract symptoms associated with benign prostatic hyperplasia and other conditions. Men with these conditions complain of urinary frequency, urgency, and nocturia (need to urinate more frequently at night). Prostatic enlargement may contribute to urinary outflow obstruction in these men and the beneficial effects of α1-blockers have been assumed to be due to relaxation of prostatic and urethral smooth muscle (Fig. 9–4). However, the weak correlation between lower urinary tract symptoms and prostatic enlargement has shifted the focus to the role of α1-adrenoceptors in the bladder, urethra, and the nervous system in causing lower urinary tract symptoms. Blockade of α1-receptors in these tissues is believed to contribute to the therapeutic effects of α1-adrenoceptor antagonists in the relief of lower urinary tract symptoms.
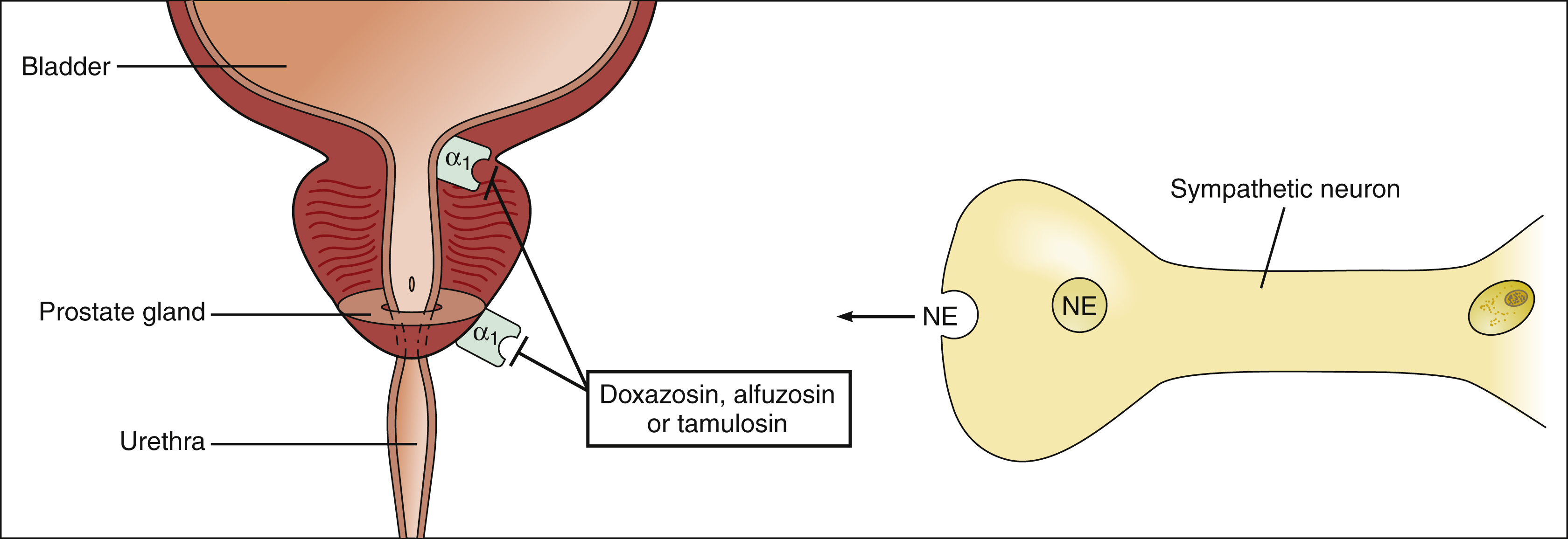
Figure 9–4 Effects of α1-adrenoceptor antagonists on the urinary bladder. Prostatic hyperplasia leads to obstruction of urine outflow from the bladder through the urethra. An α1-blocker (e.g., doxazosin, alfuzosin, or tamsulosin) will relax smooth muscle in the bladder, urethra, and prostate and thereby facilitate micturition in patients with prostatic hyperplasia. α1 = α1-adrenoceptors; NE = norepinephrine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


