Adenomatoid Tumor
Steven S. Shen, MD, PhD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Benign paratesticular tumor of mesothelial cell origin, which has a variety of growth patterns, including glands, cysts, tubules, cords, or isolated cells
Clinical Issues
Most common tumor of testicular adnexa (32%)
Usually asymptomatic, small and solid intrascrotal/extratesticular adnexal mass
Most commonly in epididymis, also in tunica vaginalis, albuginea, and rete testis
Macroscopic Features
Small well-circumscribed white tan, homogeneous firm mass
< 5 cm (majority < 2 cm)
Microscopic Pathology
Well-circumscribed, nonencapsulated tumor mass
Channels, gland-like or irregular cystic spaces, and nests and cords
Cuboidal to flat or ovoid cells with round nuclei, abundant dense cytoplasm with vacuoles
May show signet ring cell appearance
Intervening fibrous stroma ± smooth muscle
Lymphoid aggregates may be prominent within or at periphery of tumor
Ancillary Tests
Positive for cytokeratin, calretinin, Podoplanin(D2-40), CK5/6, thrombomodulin, WT1
Negative for CEA, CD15, FXVIIIAg, S100, CD31, CD34, FLI-1(vascular markers)
TERMINOLOGY
Definitions
Benign paratesticular tumor of mesothelial cell origin, which has a variety of growth patterns, including glands, cysts, tubules, cords, or isolated cells
CLINICAL ISSUES
Epidemiology
Incidence
Most common tumor of testicular adnexa
Age
Range: 18-79 years (average: 36 years)
Presentation
Usually asymptomatic, small and solid intrascrotal mass
Most commonly occurs in head of epididymis, although it may occur in tunica vaginalis, albuginea, and rete testis
Tumors may rarely be intratesticular and involve parietal tunica or spermatic cord
Treatment
Surgical approaches
Surgical excision is curative
Prognosis
Benign clinical course
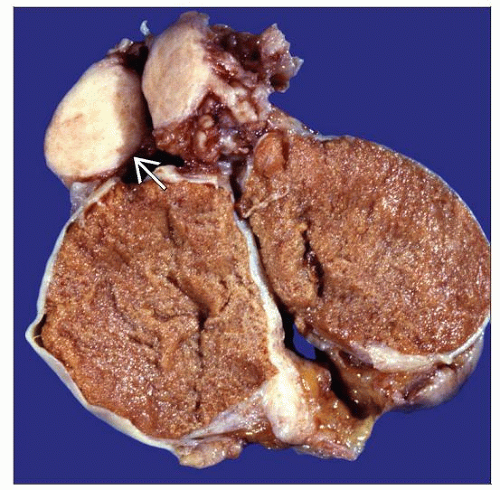
MACROSCOPIC FEATURES
General Features
Small, well-circumscribed, white-tan, homogeneous, firm mass
No hemorrhage or necrosis
Size
< 5 cm (majority < 2 cm)
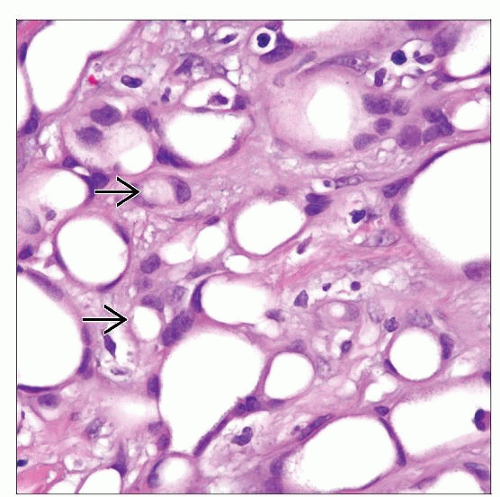
MICROSCOPIC PATHOLOGY
Histologic Features
Well-circumscribed, unencapsulated mass
Tubules; gland-like, irregular cystic spaces or channels
Nests and cords; true solid pattern rare
Cuboidal, flat, or ovoid cells with round nuclei and abundant dense cytoplasm with vacuoles
May show signet ring cell appearance
May be cellular or infarcted
Intervening fibrous stroma ± smooth muscle fibers
Lymphoid aggregates may be prominent within or at periphery of tumor
Rare tumors may be infarcted
Surrounding inflammation and reactive myofibroblastic proliferation may simulate invasion
Cytologic Features
Eosinophilic, vacuolated, signet ring
Predominant Pattern/Injury Type
Nests, cords, gland-like, tubular, cystic, and plexiform
Predominant Cell/Compartment Type
Cuboidal to flat to ovoid with uniform cytology
ANCILLARY TESTS
Histochemistry
PAS-diastase
Reactivity: Negative
Mucicarmine
Reactivity: Negative
Immunohistochemistry
Positive for cytokeratin, calretinin, Podoplanin(D2-40), CK5/6, thrombomodulin, WT1
Negative for CEA, CD15, MOC-31, EpCAM/BER-EP4/CD326, FXVIIIAg, S100, CD31, CD34, FLI-1
DIFFERENTIAL DIAGNOSIS
Sex Cord Stromal Tumor
Usually intraparenchymal tumor
Positive for inhibin and Melan-A(MART-1)
Negative for cytokeratin
Malignant Mesothelioma
Larger tumor, destructive and infiltrative growth
Greater cytologic atypia
Metastatic Signet Ring Cell Carcinoma
Clinical history and older age
Infiltrative growth, greater cytologic atypia, frequent mitoses
Positive for CEA, CD15, EpCAM/BER-EP4/CD326, and MOC-31; negative for calretinin and Podoplanin(D2-40)
Epithelioid Hemangioma/Hemangioendothelioma
Vasoformative lesion composed of vacuolated cells
Positive for vascular markers (CD31, CD34, FLI-1); negative or weakly/focally positive for cytokeratin
Germ Cell Tumors (Particularly Yolk Sac Tumor)
Intraparenchymal mass with heterogeneous appearance
Obvious malignant cytologic features
Positive for Oct3/4, SALL4, and CD30(BerH2); negative for calretinin
Leiomyosarcoma or Leiomyoma (vs. Leiomyomatous Adenomatoid Tumor)
More compact cellular spindle cell proliferation with cytologic atypia and increased mitoses
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree