The M2 and M4 receptors are coupled with Gαi proteins and their activation decreases cyclic adenosine monophosphate (cyclic AMP, or cAMP) levels, by inhibiting adenylate cyclase, or increases potassium efflux. The effects produced by activation of muscarinic receptors are summarized in Table 6–1.
The acetylcholine receptor agonists that are currently available for clinical use do not selectively activate subtypes of muscarinic receptors, but an M1 selective antagonist, pirenzepine, has been developed (see Chapter 7).
Nicotinic Receptors
Nicotinic receptors are found at all autonomic ganglia, at somatic neuromuscular junctions, and in the central nervous system. These receptors are acetylcholine-gated sodium channels whose activation leads to sodium influx and membrane depolarization. At autonomic ganglia, activation of nicotinic receptors produces excitation of postganglionic neurons leading to the release of neurotransmitters at postganglionic neuroeffector junctions. At junctions of somatic nerves and skeletal muscle, activation of nicotinic receptors depolarizes the motor end plate and leads both to the release of calcium from the sarcoplasmic reticulum and to the contraction of muscles. In the brain, activation of nicotinic receptors causes excitation of presynaptic and postsynaptic neurons.
Nicotinic receptors are pentamers formed by the assembly of five transmembrane polypeptide subunits (Fig. 6–1). These subunits are divided into classes (alpha [α] through epsilon [ε]) according to their molecular structure. Each type of nicotinic receptor (muscle, ganglionic, brain) is composed of a unique combination of these subunits. All subunits appear to participate in the formation of acetylcholine-binding sites and influence the functional properties of the receptors, but a clear understanding of the unique roles of the different classes of subunits has not yet been obtained.
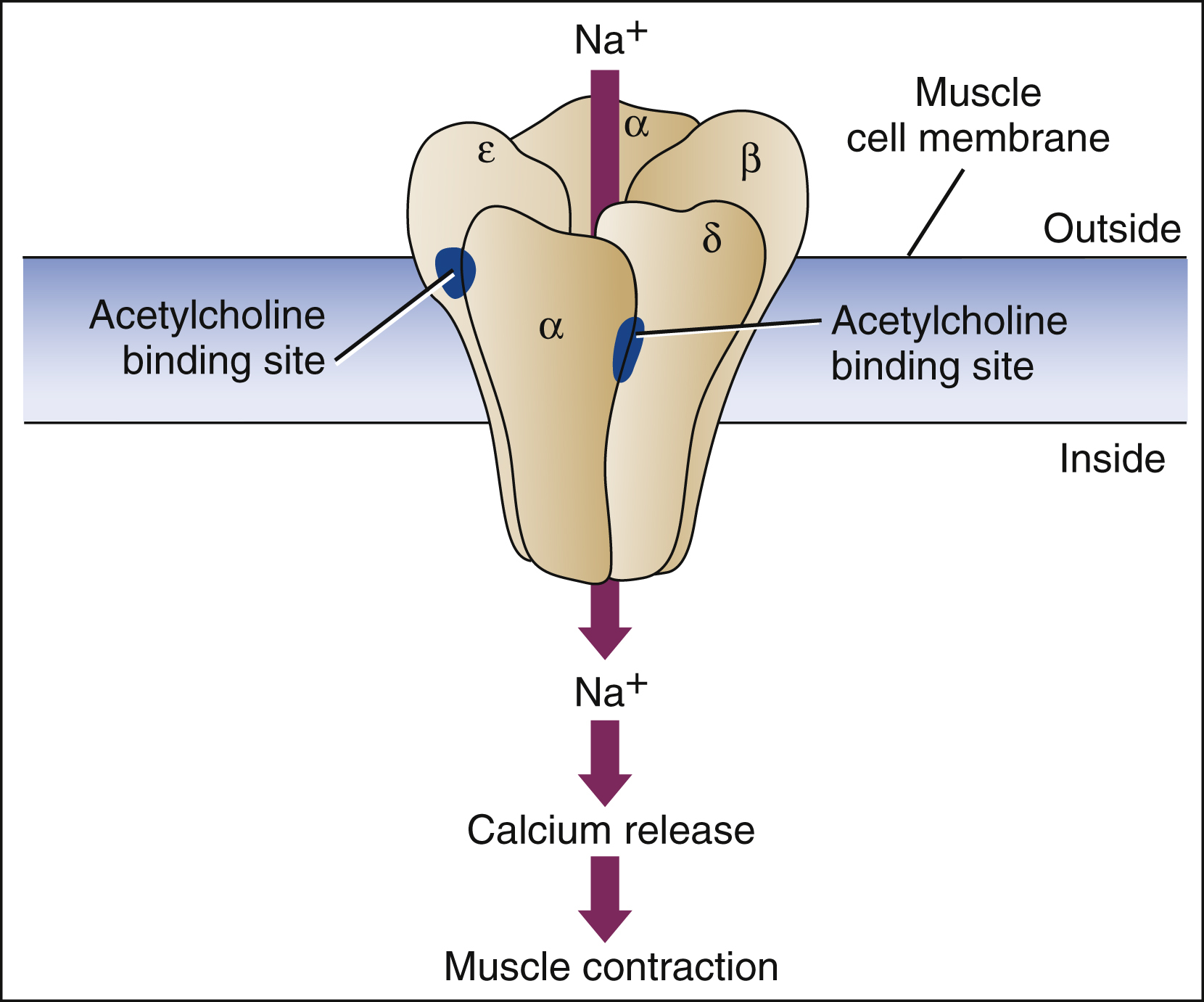
Figure 6–1 The nicotinic receptor is an acetylcholine-gated sodium channel. The channel is a polypeptide pentamer composed of varying combinations of α, β, δ, and ε subunits. In the muscle type of nicotinic receptor shown here, acetylcholine-binding sites are formed by pockets at the interface of the α and δ subunits and the α and ε subunits. Acetylcholine binding to the receptor causes sodium influx, membrane depolarization, release of calcium from the sarcoplasmic reticulum, and muscle contraction. Nicotinic receptors at autonomic ganglia and in the brain have a different subunit composition.
Classification of Acetylcholine Receptor Agonists
The acetylcholine receptor agonists can be classified as direct acting or indirect acting. The direct-acting agonists bind and activate acetylcholine receptors. Most indirect-acting agonists increase the synaptic concentration of acetylcholine by inhibiting cholinesterase, whereas others augment acetylcholine signal transduction.
DIRECT-ACTING ACETYLCHOLINE RECEPTOR AGONISTS
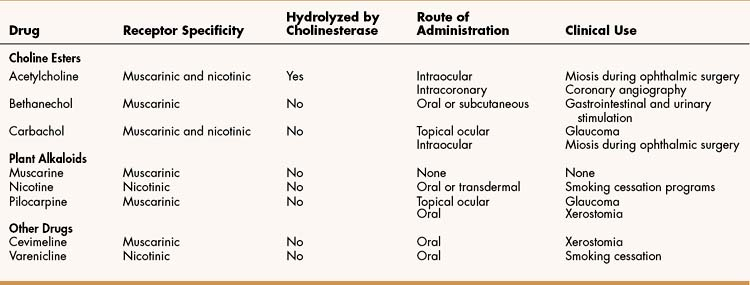
The direct-acting agonists include the choline esters, the plant alkaloids, and newer synthetic drugs called cevimeline and varenicline. These drugs all bind and activate acetylcholine receptors, but they differ with respect to their affinity for muscarinic and nicotinic receptors and their susceptibility to hydrolysis by cholinesterase (Table 6–2).
Choline Esters
The choline esters include acetylcholine and synthetic acetylcholine analogues, such as bethanechol and carbachol.
General Properties
The choline esters are positively charged quaternary ammonium compounds that are poorly absorbed from the gastrointestinal tract and are not distributed to the central nervous system. Acetylcholine and carbachol activate both muscarinic and nicotinic receptors, whereas bethanechol activates only muscarinic receptors. Because of their lack of specificity for muscarinic receptor subtypes, the muscarinic receptor agonists cause a wide range of effects on many organ systems.
OCULAR EFFECTS
Muscarinic receptor agonists increase lacrimal gland secretion and stimulate contraction of the iris sphincter muscle and the ciliary muscles. Contraction of the iris sphincter muscle produces pupillary constriction (miosis), whereas contraction of the ciliary muscles enables accommodation of the lens to focus on close objects (Fig. 6–2).
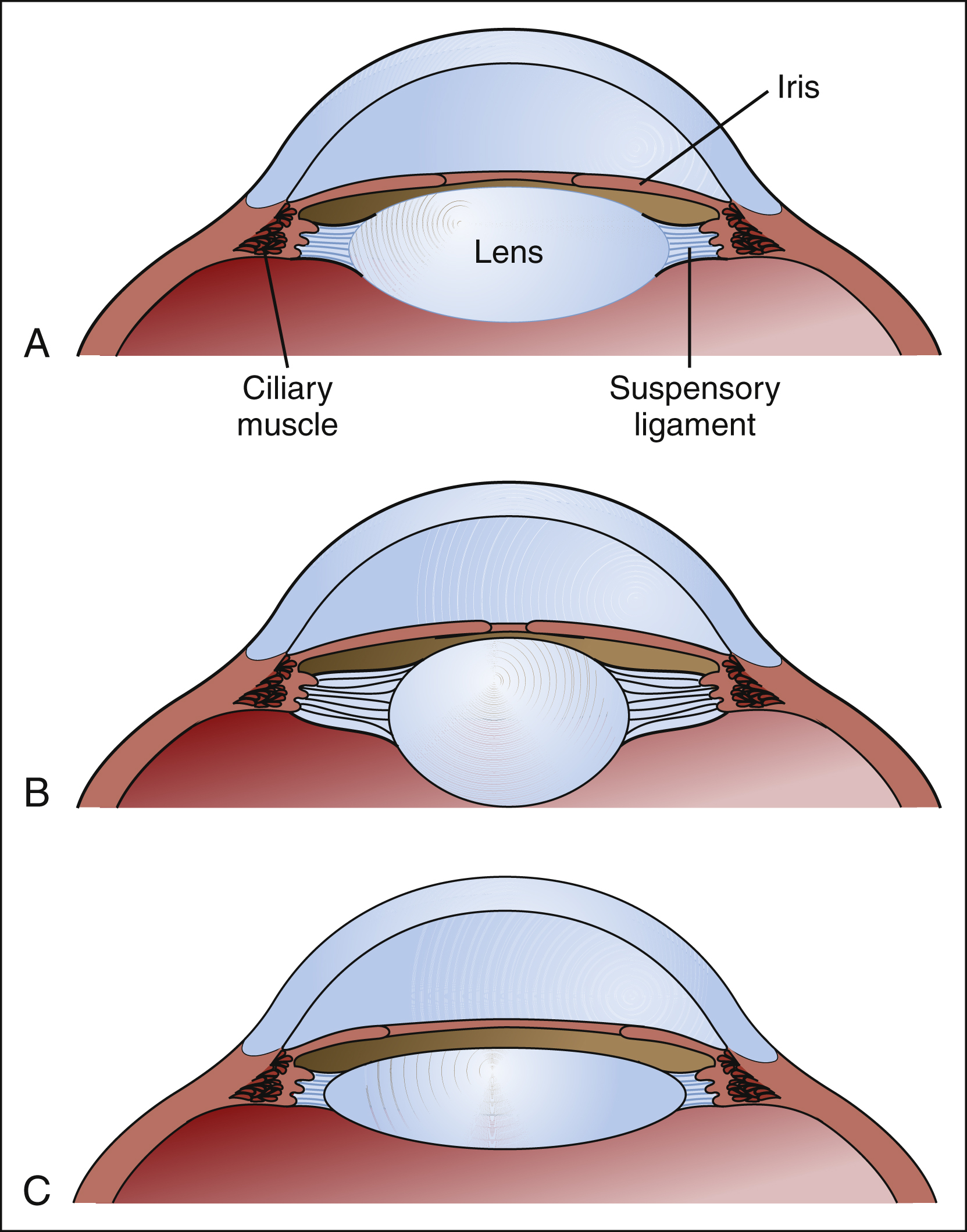
Figure 6–2 Effects of pilocarpine and atropine on the eye. (A) The relationship between the iris sphincter and ciliary muscle is shown in the normal eye. (B) When pilocarpine, a muscarinic receptor agonist, is administered, contraction of the iris sphincter produces pupillary constriction (miosis). Contraction of the ciliary muscle causes the muscle to be displaced centrally. This relaxes the suspensory ligaments connected to the lens, and the internal elasticity of the lens allows it to increase in thickness. As the lens thickens, its refractive power increases so that it focuses on close objects. (C) When atropine, a muscarinic receptor antagonist, is administered, the iris sphincter and ciliary muscles relax. This produces pupillary dilatation (mydriasis) and increases the tension on the suspensory ligaments so that the lens becomes thinner and focuses on distant objects.
RESPIRATORY TRACT EFFECTS
Stimulation of muscarinic receptors increases bronchial muscle contraction and causes an increase in the secretion of mucus throughout the respiratory tract. Because muscarinic receptor agonists can cause bronchoconstriction, they should be avoided or used with extreme caution in patients with asthma and other forms of obstructive lung disease.
CARDIAC EFFECTS
Muscarinic receptor agonists decrease impulse formation in the sinoatrial node by reducing the rate of diastolic depolarization. As a result, they slow the heart rate. In addition, they slow conduction of the cardiac action potential through the atrioventricular node, and this leads to an increased PR interval (time between the beginning of the P wave to the beginning of the QRS complex) on the electrocardiogram.
VASCULAR EFFECTS
Acetylcholine typically causes vasodilation, though vasoconstriction may occur under some conditions (see below). The vasodilative effect of acetylcholine is mediated by muscarinic M3 receptors located in vascular endothelial cells, where muscarinic stimulation causes activation of nitric oxide synthetase and the formation of nitric oxide. Nitric oxide is a gas that diffuses into vascular smooth muscle cells and activates guanylyl cyclase to increase the formation of cyclic guanosine monophosphate (cyclic GMP), leading to vascular smooth muscle relaxation and vasodilation.
GASTROINTESTINAL AND URINARY TRACT EFFECTS
When muscarinic receptor agonists are taken, they stimulate salivary, gastric, and other secretions in the gastrointestinal tract. They also increase contraction of gastrointestinal smooth muscle (except sphincters) by stimulating the enteric nervous system located in the gut wall. This, in turn, increases gastrointestinal motility. Whereas muscarinic receptor agonists stimulate the bladder detrusor muscle, they relax the internal sphincter of the bladder, and these effects promote emptying of the bladder (micturition). Higher doses of these agonists, therefore, can produce excessive salivation and cause diarrhea, intestinal cramps, and urinary incontinence (the “all faucets turned on” syndrome).
Acetylcholine
CHEMISTRY AND PHARMACOKINETICS
Acetylcholine is the choline ester of acetic acid. It is rapidly hydrolyzed by cholinesterase and has an extremely short duration of action.
EFFECTS AND INDICATIONS
Because of its limited absorption, short duration of action, and lack of specificity for muscarinic or nicotinic receptors, acetylcholine has limited clinical applications.
An ophthalmic solution of acetylcholine available for intraocular use during cataract surgery produces miosis after extraction of the lens. The solution also can be used in other types of ophthalmic surgery that require rapid and complete miosis. Topical ocular administration of acetylcholine is not effective, because acetylcholine is hydrolyzed by corneal cholinesterase before it can penetrate to the iris and ciliary muscle.
In patients having diagnostic coronary angiography, acetylcholine can be administered by direct intracoronary injection to provoke coronary artery spasm. The vasospastic effect of acetylcholine is caused by stimulation of muscarinic M3 receptors located on vascular smooth muscle that mediate smooth muscle contraction. In most situations, the vasodilative effect of acetylcholine is more pronounced than the vasoconstrictive effect. In patients with vasospastic angina pectoris, however, intracoronary injection of acetylcholine can provoke a localized vasoconstrictive response, and this helps establish the diagnosis of vasospastic angina.
Bethanechol and Carbachol
CHEMISTRY AND PHARMACOKINETICS
Bethanechol and carbachol are choline esters of carbamic acid. They are resistant to hydrolysis by cholinesterase, and their duration of action is relatively short, lasting for several hours after topical ocular or systemic administration.
EFFECTS AND INDICATIONS
Bethanechol selectively activates muscarinic receptors and can be used to stimulate bladder or gastrointestinal muscle without significantly affecting heart rate or blood pressure. Although it generally has been replaced by more effective treatments, bethanechol has been given postoperatively or postpartum to increase bladder muscle tone in patients who suffer from nonobstructive, neurogenic urinary retention after receiving anesthetics or other drugs administered during childbirth or surgery. Therapeutic doses of bethanechol given orally or subcutaneously have little effect on blood pressure, but the drug should never be administered intravenously, because this can cause hypotension and bradycardia.
Carbachol is effective in the treatment of chronic open-angle glaucoma, but it is usually used in cases in which a patient does not respond adequately to pilocarpine (see “Pilocarpine”). Carbachol can also be used to produce miosis during ophthalmic surgery.
Muscarine and Nicotine
SOURCE AND EFFECTS
Muscarine is found in mushrooms of the genera Inocybe and Clitocybe, and the consumption of these poisonous mushrooms can cause diarrhea, sweating, salivation, and lacrimation. Muscarine is also found in trace amounts in Amanita muscaria, the original source of muscarine, but the toxicity of this mushroom is largely due to its content of ibotenic acid. Nicotine is derived from Nicotiana plants and is contained in cigarettes and other tobacco products. The effects of nicotine dependence are discussed in Chapter 25.
Pilocarpine
CHEMISTRY AND PHARMACOKINETICS
Pilocarpine is a tertiary amine alkaloid that is obtained from Pilocarpus, a small shrub. The drug is well absorbed after topical ocular and oral administration.
EFFECTS AND INDICATIONS
Pilocarpine, which has greater affinity for muscarinic receptors than for nicotinic receptors, can produce all of the effects of muscarinic receptor stimulation.
Pilocarpine is a second-line drug for the treatment of chronic open-angle glaucoma, in which it lowers intraocular pressure by increasing the outflow of aqueous humor (Box 6-1). It is also used in the treatment of acute angle-closure glaucoma, a medical emergency in which blindness can result if the intraocular pressure is not lowered immediately. The main side effects of ocular pilocarpine administration are decreased night vision, which is caused by miosis, and difficulty in focusing on distant objects, which occurs because the lens is accommodated for close vision.
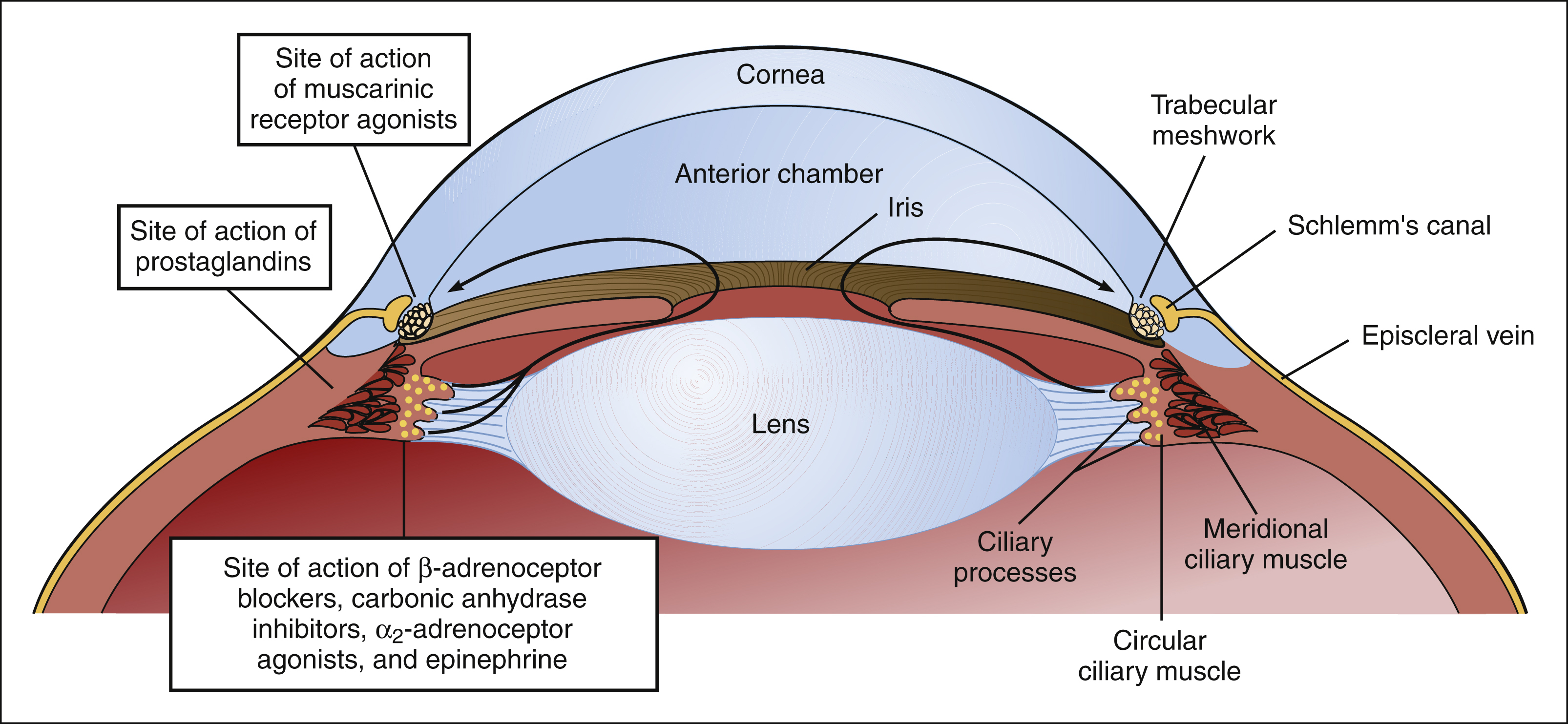
BOX 6–1 TREATMENT OF CHRONIC OPEN-ANGLE GLAUCOMA
In the normal eye, aqueous humor is secreted by the ciliary processes and flows through the pupillary aperture of the iris and into the anterior chamber. It then drains through the trabecular meshwork in Schlemm’s canal. In patients with open-angle glaucoma, persistently elevated intraocular pressure is associated with narrowing of the anterior chamber angle, a decrease in the rate of aqueous outflow, and the gradual loss of peripheral vision. Various types of drugs can be used to reduce intraocular pressure before irreversible optic nerve damage occurs. The sites of action of these drugs are shown below.
Some types of drugs act by enhancing the drainage of aqueous humor. Muscarinic receptor agonists (e.g., pilocarpine) stimulate the contraction of meridional ciliary muscle fibers that insert near the trabecular meshwork. Contraction of these fibers opens the trabecular spaces so that aqueous humor drains more easily. Prostaglandins (e.g., latanoprost) increase aqueous drainage through an alternative pathway known as the uveoscleral route. In this pathway, aqueous humor flows through the ciliary muscles into the suprachoroidal space.
Other types of drugs act by reducing the amount of aqueous humor produced by the ciliary processes. The β-adrenoceptor blockers (e.g., timolol) and the α2-adrenoceptor agonists (e.g., apraclonidine) reduce the formation of cyclic AMP, a substance that stimulates aqueous humor production. Carbonic anhydrase inhibitors (e.g., dorzolamide) block the formation of bicarbonate by carbonic anhydrase, an enzyme that is required for aqueous humor secretion. Epinephrine probably acts by reducing blood flow in the ciliary processes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree