OUTLINE
Compounding Facilities and Equipment
Storage Conditions for Drug Products and Ingredients
Safe Handling of Drugs and Chemicals in the Pharmacy
I. COMPOUNDING FACILITIES AND EQUIPMENT
A. Legal requirements
The minimum requirements for equipment and facilities for pharmacies are usually set by state pharmacy practice acts. At one time, these acts had very specific requirements, such as minimum number of square feet in the pharmacy; number and types of mixing, measuring, and weighing equipment; types and even titles of mandated reference books; and so on. Now most state laws follow the guidelines of the NABP Model Rules for the Practice of Pharmacy with more general statements, such as a compounding area of “sufficient size” to allow for safe and proper compounding, and “The Pharmacy shall carry and utilize the equipment and supplies necessary to conduct a Pharmacy in a manner that is in the best interest of the patients served” (1). Consult your state statutes for applicable information for your practice site.
B. Professional standards for nonsterile compounding equipment and facilities
USP Chapter 〈795〉 Pharmaceutical Compounding—Nonsterile Preparations and Chapter 〈1075〉 Good Compounding Practices have sections on compounding equipment and facilities for nonsterile compounding. These chapters do not distinguish between compounding done in pharmacies and that done in medical offices, clinics, or hospitals. Though they do not give lists of specific required equipment (e.g., balances, mortars, graduated cylinders), they address both facilities and equipment in more general ways (2,3). The ASHP Technical Assistance Bulletin on Compounding Nonsterile Products in Pharmacies has a similar section devoted to facilities and equipment for nonsterile compounding (4).
a. The compounding area should be of adequate size and design for the type of compounding done in the facility. If possible, the area should be separated from other activities of the pharmacy or professional practice. Both of the USP chapters and the ASHP Technical Assistance Bulletin place special emphasis on ensuring that the location and amount of space is sufficient for storage, compounding, packaging, and labeling so as to minimize dust and particulate matter and prevent cross-contamination and mix-ups of ingredients or preparations during compounding.
b. The facility, including the storage area, is to be kept in a clean, sanitary, and orderly condition with regular and proper disposal of waste and trash.
c. It should have appropriate lighting, ventilation, and temperature control so that the area meets storage conditions as set forth in USP monographs and FDA and manufacturer recommendations for drugs and chemicals stored and used in the facility.
d. The facility should have a sink with hot and cold tap (potable) water, hand-soap and dish detergent, and air dryer or single-use towels to be used for washing hands and for washing glassware and other compounding equipment.
(1) The potable water should meet the requirements of the Environmental Protection Agency’s (EPA) National Primary Drinking Water Regulations, as given in 40 CFR Part 141.
(2) Potable water is acceptable for washing hands, glassware, and compounding equipment, but it is not to be used as an ingredient in making drug preparations. Purified water USP is to be used as the water ingredient for nonsterile preparations and for rinsing compounding equipment. For water requirements for sterile products, see Chapter 15 in this book and USP water monographs.
2. Compounding equipment (2–4)
a. Compounding equipment is to be of the appropriate type, design, and size for the intended use.
b. Equipment surfaces that come in contact with ingredients or compounded preparations should not be reactive, additive, or sorptive so that the purity of preparations is not compromised during compounding and packaging.
c. All equipment used in compounding (including analytical devices used to verify the strength and properties of ingredients and finished preparations) should be routinely inspected, cleaned, maintained, and checked for expected performance. All equipment should be used in conformance with manufacturer’s recommendations. Devices that are used for measurement or analysis should be calibrated on a regularly scheduled basis, and records should be kept of these activities. It is highly recommended that standard operating procedures (SOPs) be written and used for all compounding and analytical equipment.
d. Equipment should be stored appropriately so as to maintain it in a clean condition, free from contamination. Just before use, it should be inspected, and immediately after use it should be carefully cleaned.
C. Recommendations and requirements for sterile compounding
Standards for equipment and facilities for compounding sterile products are much more specific. For information on this subject, see Chapter 32 of this book and USP Chapter 〈797〉.

D. The following is a modest list of equipment that will serve most nonsterile compounding needs. Where appropriate, descriptions, uses, and limitations are given. The CD that accompanies this book has an excellent audio-visual slideshow on the use of balances and much of the compounding equipment described here.
1. Balances
For detailed descriptions of balances, their specifications, and proper care and use, see Chapter 14, Selection and Use of Weighing and Measuring Equipment, and the CD with this book.
2. Volumetric apparatus
For specifications and descriptions of graduated cylinders and other volumetric apparatus, see Chapter 14 and the CD with this book.
3. Mortars and pestles
a. Wedgwood mortars are heavy-duty, durable mortars available in various sizes: 2 oz, 4 oz, 8 oz, 16 oz, and 32 oz. They are made with abradant interior surfaces, making them ideal for particle size reduction and for making emulsions, where efficient shear is desirable. Because of their porous interiors, Wedgwood mortars should not be used for drugs that stain, for drugs present in small quantities, or for very potent or hazardous drugs; and particular care must be taken with cleaning Wedgwood mortars so as to avoid cross-contamination of future preparations. The rough surfaces of Wedgwood mortars do become smooth with continued use. When this occurs, some pharmacists triturate washed sand or emery in the mortar in an effort to re-roughen the surfaces, but this procedure has limited success.

MORTARS AND PESTLES (GLASS, WEDGWOOD, AND CERAMIC).
b. Porcelain mortars are available in the same sizes as Wedgwood mortars. They have a more attractive white, glazed surface but provide less shearing efficiency than Wedgwood mortars and are somewhat less durable.
c. Ceramic mortars are similar to Wedgwood mortars; they have abradant interior working surfaces and therefore have similar uses and precautions. They are available in sizes ranging from 2 oz to 32 oz. Like porcelain mortars, they are less durable than Wedgwood mortars.
d. Clear glass mortars have smooth, nonporous interior surfaces, making them useful for triturating drugs that stain. Because of their smooth sides, glass mortars are not as efficient as Wedgwood or ceramic mortars in reducing particle size of powders and especially hard crystals, but they are useful for making solutions and suspensions and for diluting creams to lotions. They are not efficient for making emulsions because adequate shear is difficult to achieve with a glass mortar and pestle. They are preferred for triturating highly potent drugs and should always be used if it is necessary to triturate a hazardous drug. Like Wedgwood mortars, they are available in sizes ranging from 2 oz to 32 oz.
e. For maximum efficiency, use pestles that are matched with respect to size and type with the corresponding mortar.
4. Spatulas

SPATULAS.
a. Stainless steel spatulas with wooden or hard plastic handles are available in various sizes, with blades from 3 to 12 inches in length. It is important to use the appropriate size and type for the task.
(1) The small sizes are used for handling dry chemicals, for scraping materials from other spatulas and from the sides of small mortars and pestles, and for levigating small quantities of drugs and chemicals on ointment pads or slabs.
(2) The larger sizes are used for handling larger quantities of materials. Spatulas with 8- to 12-inch blades are preferred for levigating moderate-to-large quantities of drugs and for mixing or spatulating ointments.
(3) Special spatulas of this type with angled blades are also available.
b. Small, double-bladed, nickel–stainless steel spatulas, sometimes called micro spatulas, are useful for withdrawing small amounts of chemicals and drugs from their containers. They are not used for levigation.
c. Hard rubber or Teflon-coated stainless steel spatulas, 4 and 6 inches, are special purpose only: They are used in handling drugs and chemicals, such as iodine, that react with metal. In general, they lack the flexibility needed for levigating and spatulating ointments.
d. Flexible, rubber spatulas, sometimes called rubber policemen or rubber scrapers, have broad, rectangular, flexible rubber, silicone, or plastic scrapers with wooden or plastic handles. These spatulas are very useful for scraping material from the inside surface of mortars when transferring a preparation from the mortar to a packaging container.
5. Funnels are available in both glass and plastic and come in a wide range of capacities and with different stem lengths and diameters.
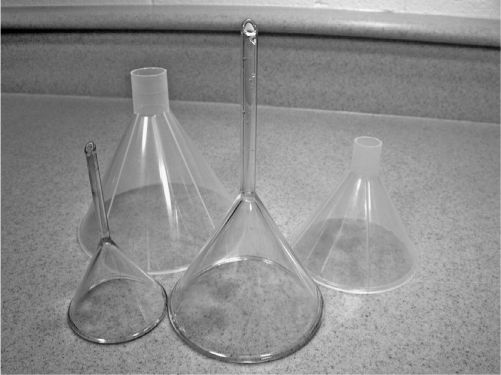
GLASS AND PLASTIC FUNNELS.
a. Funnels with narrow stem diameters are used for transferring solutions from one vessel or bottle to another. These are also used with filter papers in filtering solutions. Do not try to use them for transferring thick suspensions or emulsions from a mixing vessel to a prescription bottle—the bore on the glass stem will generally get clogged, and you will have a mess!
b. Powder funnels have short, larger diameter stems. These are useful for transferring powders from mortars and other mixing vessels to dispensing and stock bottles. Depending on the viscosity of the liquid, these may also be used to transfer suspensions and emulsions from mixing vessel to dispensing container.
c. When transferring large quantities of powders or liquids, so-called canning funnels can be useful.
6. Ointment slabs and pads
a. Ointment slabs
(1) Though ointment slabs are called ointment slabs because of their use as a surface for levigation and spatulation in compounding ointments, an ointment slab may also be used as a clean, hard surface for holding powders when punching capsules and as a surface for rolling semi-solid materials when marking hand-rolled suppositories or lozenges.
(2) Some ointment slabs have a rough surface on one side to facilitate particle size reduction when levigating powders for ointments. Care must be exercised to avoid getting water-insoluble materials (dyes, tars, etc.) in the pores on this rough side because this surface is difficult to clean and residues may contaminate future preparations.
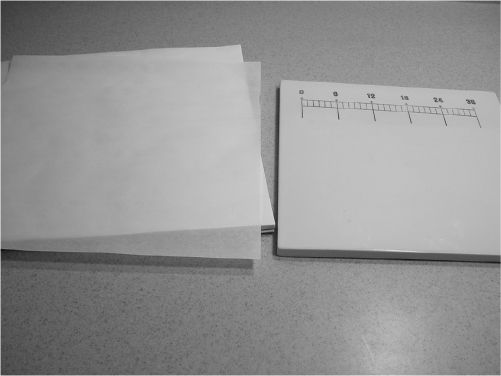
OINTMENT PAD AND OINTMENT SLAB.
b. Ointment pads
(1) Ointment pads are convenient because the top sheet is used and then torn off and discarded when the job is completed—a great time-saver.
(2) They do have some limitations. They soak up liquids, including the water phase of creams, aqueous solutions to be incorporated into ointment bases, and even thick tarlike ingredients; ointment slabs are preferred over pads in these situations.
7. Glass stirring rods are useful for stirring liquid preparations. Spatulas are not to be used as stirring rods.
8. Pyrex or other heat-resistant beakers come in many sizes, from 10 mL to 4 L. The most common sizes used in compounding are 50 mL, 100 mL, 150 mL, 250 mL, 400 mL, 600 mL, and 1,000 mL. These are described in Chapter 14.
9. Pyrex or other heat-resistant Erlenmeyer flasks also come in various sizes, from 25 mL to 6 L. These are useful when making solutions because the contents of the flask can easily be mixed by swirling and there is less danger of spillage than when using a beaker. On the other hand, it is more difficult to add ingredients to an Erlenmeyer flask because of the small flask orifice.
10. Crucibles and evaporating dishes are handy for heating suppository and ointment bases. They can also be used as the water vessel for a simple, improvised hot-water bath.
11. Suppository and troche molds
a. Aluminum and plastic disposable suppository molds are needed for making suppositories by fusion. These are described and pictured in Chapter 31, Suppositories.
b. Plastic disposable troche molds are described and pictured in Chapter 26, Capsules, Lozenges, and Other Solid Oral Dosage Forms.
12. Personnel protective equipment (PPE), including lab coats or gowns, safety glasses, and disposable gloves, should be available and used as needed when compounding. When handling some drugs and chemicals, the use of particulate respirators is recommended. These are facemasks that protect personnel from inhalation exposure. They are available in a variety of models, which provide varying degrees of protection and user comfort; some provide protection from aerosols. Select a model or models that are approved by the National Institute for Occupational Safety and Health (NIOSH); a surgical mask does not afford the necessary protection (5).
13. Paper or test strips for measuring pH: These are available in various pH ranges at a nominal price; they are essential for quality control monitoring of preparations containing water.
14. Filter papers, various sizes
15. Cutting devices, such as scissor and single-edge razor blades
16. Wax or other marking pen
17. Brushes of various sizes and shapes for cleaning graduates and funnels
18. Thermometers
a. A laboratory thermometer is needed for monitoring and adjusting the temperatures of water baths and of liquids and molten semisolids when this is required during compounding.
b. Ambient temperature thermometers are required for monitoring the temperature in dispensing, compounding, and drug storage areas, including refrigerators and freezers. Models that are available also measure relative humidity, and some have memory features that store minimum and maximum temperatures during specified periods. Some models have chart recorders that make a hardcopy tracing of the temperature on an ongoing basis.
19. Heating devices
a. Microwave oven
(1) As a heating device, a microwave oven is convenient, safe, and fast.
(2) Because microwave ovens work on the principle of alternating polarity, they do not heat non-polar substances, such as white petrolatum and some waxes and oils. This disadvantage can be overcome by using the microwave oven to heat water in a crucible or beaker; this may then be used as a hot water bath for heating or melting nonpolar items.
(3) Microwave ovens can develop “hot spots” that may cause overheating and degradation of ingredients.
b. Hot plate

HOT PLATE WITH MAGNETIC STIRRER.
(1) Hot plates offer fast and direct sources of heat, but they require careful monitoring to avoid overheating or scorching of ingredients. When heating a preparation that must have a carefully controlled temperature and the desired temperature is 100°C or less, a hot-water bath may be the preferred heating device.
(2) Some hot plates are available with magnetic stirring devices, which can be very handy.
c. Hot-water bath
A hot-water bath can be improvised by using two heat-resistant beakers or similar vessels of different sizes. Water is added to the larger vessel, and this is heated either on a hot plate or in a microwave oven. The material to be melted or heated is placed in the smaller vessel and this is then floated in the hot water contained in the larger vessel.
20. Refrigerator (including a freezing compartment) that will maintain temperatures as specified in the USP.
21. If sterile products are compounded, special equipment (such as a laminar airflow hood) is required. The equipment and the specialized environment needed for this sort of practice are discussed in Chapter 32, General Principles of Sterile Dosage Form Preparation and in USP Chapter 〈797〉.
22. A wide variety of other useful pieces of equipment are available. Decisions on the purchase and use of particular equipment depend on the amount and type of compounding performed and economic circumstances of the professional practice. Examples of other types of equipment are listed here.
a. Sieves, both individual and as sets with various mesh sizes, which are available at a modest cost. These are useful when powders of a particular size are needed for product uniformity or comfort.
b. A magnetic stirring device. A combination hot plate–magnetic stirrer is more versatile but also more expensive.
c. Thermostatically controlled hot-water baths, which offer great convenience, especially if formulations that are made require carefully controlled constant temperatures.
THERMOSTATICALLY CONTROLLED HOT-WATER BATH.
d. A source of homogenization, such as a hand-homogenizer or a blender.
e. Electric mixer.
f. Electronic mortar and pestles systems, such as the Topitec Electric Ointment Mixer and the Unguator Mixing System. These systems are designed to mix suspensions, ointments, and gels directly in special dispensing jars. Because these are closed systems, the compounder is protected from exposure to the ingredients during the mixing process.
g. A pH meter. This offers both convenience and accuracy but is considerably more expensive than pH paper or strips. Meters are available in both stationary and portable models; some also measure temperature in degrees Celsius.
h. Ductless containment hoods, glove boxes, and laboratory fume hoods. These provide protection from exposure to compounding ingredients, including powders and particulates, fumes, and vapors. Depending on the amount and type of compounding done, equipment of this type may be required for a compounding facility. Biological safety cabinets are used for protection from hazardous drugs when compounding sterile products. These are discussed in Chapter 32.
i. Capsule-filling machines, ranging from very simple devices at approximately $20 to motorized machines for more than $5,000. These can be purchased from pharmacy supply vendors.
j. Ointment mills, which make very fine ointments. This piece of equipment is quite expensive, usually several thousand dollars, so you need to make a lot of ointments for this sort of equipment to make economic sense.
k. For pharmacies that want to do in-house analysis of their bulk chemicals or drugs or of finished preparations, various kinds of analytical equipment, from melting-point instruments to spectrophotometers.
II. COMPOUNDING INGREDIENTS
A. Definitions and ingredient grade abbreviations
1. The definitions given next are quoted from the NABP Model State Pharmacy Act (6). USP Chapter 〈795〉 and federal law 21 CFR 210.3(b)(7)–(8) have similar definitions.
a.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree