Cardiovascular System Disorders
Learning Objectives
After studying this chapter, the student is expected to:
1. Describe the common diagnostic tests for cardiovascular function.
3. Explain the role of cholesterol and lipoproteins in the development of atheromas.
4. Explain the significance of metabolic syndrome in the development of cardiovascular disease.
5. State the factors predisposing to atherosclerosis.
6. Compare angina and myocardial infarction.
7. Describe the common arrhythmias and cardiac arrest.
9. Explain the changes in blood flow and their effects in common congenital heart defects.
10. Discuss the development of rheumatic fever and rheumatic heart disease.
11. Describe the etiology and pathophysiology of infectious endocarditis and pericarditis.
12. Explain the development and possible effects of essential hypertension.
13. Compare the arterial peripheral vascular diseases atherosclerosis and aneurysms.
15. Discuss the types of shock and the initial and progressive effects of shock on the body.
Key Terms
adrenergic
anastomoses
angioplasty
auscultation
autoregulation
baroreceptors
bradycardia
cardiomegaly
depolarization
ectopic
electrodes
endarterectomy
hemoptysis
microcirculation
murmurs
orthopnea
sulcus
syncope
synergistic
tachycardia
Review of the Cardiovascular System
Heart
Anatomy
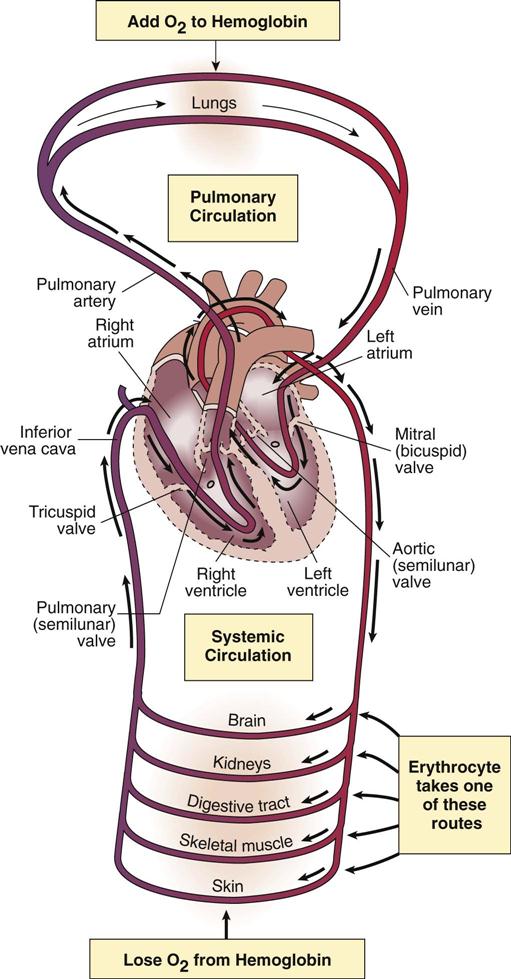
The heart functions as the pump for the circulating blood in both the pulmonary and systemic circulations. The path of a specific component of the blood, such as a red blood cell, through the heart and circulation is illustrated in Figure 12-1.
The heart is located in the mediastinum between the lungs and is enclosed in the double-walled pericardial sac (see Fig. 12-29). The outer fibrous pericardium anchors the heart to the diaphragm. The visceral pericardium, also called the epicardium, consists of a serous membrane that provides a small amount of lubricating fluid within the pericardial cavity between the two pericardial membranes to facilitate heart movements. The middle layer of the heart is the myocardium, composed of specialized cardiac muscle cells that contract rhythmically and forcefully to pump blood throughout the organs. The left ventricular wall is thicker because it must eject blood into the extensive systemic circulation. The inner layer of the heart is the endocardium, which also forms the four heart valves that separate the chambers of the heart and ensure one-way flow of blood.
The atrioventricular (AV) valves separate the atria from the ventricles; they comprise, on the right side, the tricuspid valve with three leaflets or cusps, and on the left side, the mitral or bicuspid valve with two leaflets. The semilunar valves, each with three cusps, include the aortic and pulmonary valves located at the exits to the large arteries from the ventricles. The septum separates the left and right sides of the heart.
Conduction System
Impulses to initiate cardiac contractions are conducted along specialized myocardial (cardiac muscle) fibers. No nerves are present within the cardiac muscle. The unique characteristics of cardiac muscle include the presence of intercalated disks at the junctions between fibers. These disks contain desmosomes, connections to prevent muscle cells from separating during contraction; and gap junctions, which permit ions to pass from cell to cell, facilitating rapid transmission of impulses. These specialized structures ensure that all muscle fibers of the two atria normally contract together, followed shortly by the two ventricles. This coordinated effort results in a rhythmic and efficient filling and emptying of the atria and ventricles that has sufficient force to sustain the flow of blood through the body.
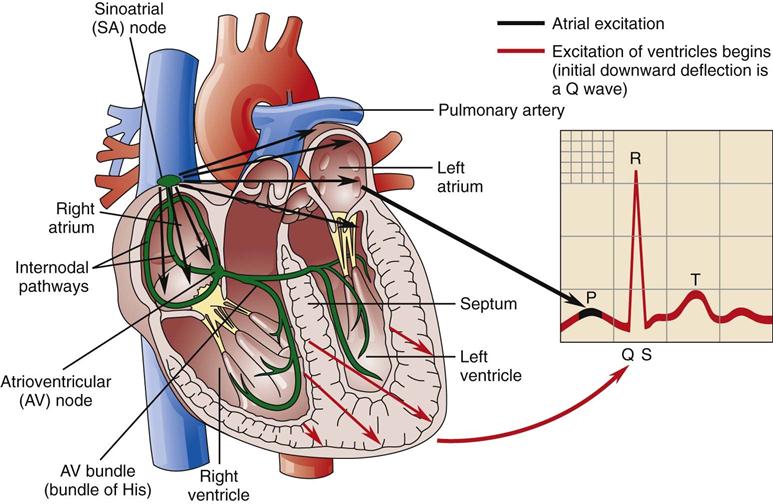
The pathway for impulses in the cardiac conduction system is as follows:
Conduction of impulses produces a change in electrical activity that can be picked up by electrodes attached to the skin at various points on the body surface, producing the electrocardiogram (ECG) (see Fig. 12-2). The atrial contraction is represented by the depolarization in the P wave, and the ventricular contraction is shown by the large wave of depolarization in the ventricles (QRS). This wave masks the effect of atrial repolarization, but the third wave (T wave) represents the repolarization of the ventricles, or recovery phase. Abnormal variations in the ECG known as arrhythmias or dysrhythmias may indicate acute problems, such as an infarction, or systemic problems, such as electrolyte imbalances (for example, potassium deficiency [see Fig. 2-8]).
Control of the Heart
Heart rate and force of contraction are controlled by the cardiac control center in the medulla of the brain. The baroreceptors in the walls of the aorta and internal carotid arteries detect changes in blood pressure and the cardiac center then responds through stimulation of the sympathetic nervous system (SNS) or the parasympathetic nervous system to alter the rate and force of cardiac contractions as required. Sympathetic innervation increases heart rate (tachycardia) and contractility, whereas parasympathetic stimulation by the vagus nerve slows the heart rate (bradycardia). The sympathetic or beta1–adrenergic receptors in the heart (see Chapter 14) are an important site of action for some drugs, such as beta-blockers. Because beta-blockers fit the receptors and prevent normal SNS stimulation, they are used to block any increases in rate and force of contractions after the heart has been damaged.
Factors that increase heart rate include:
• Elevated body temperature, such as in fever
• Increased environmental temperatures, especially if humidity is high
• Exertion or exercise, notably when beginning, followed by a leveling off
• Pain
Any stimulation of the SNS, as with stress, increases the secretion of epinephrine, which in turn stimulates beta-receptors and increases both the heart rate and contractility.
Coronary Circulation
Cardiac muscle requires a constant supply of oxygen and nutrients to conduct impulses and contract efficiently, but it has very little storage capacity for oxygen.
The distribution of the major blood vessels in the coronary circulation is:
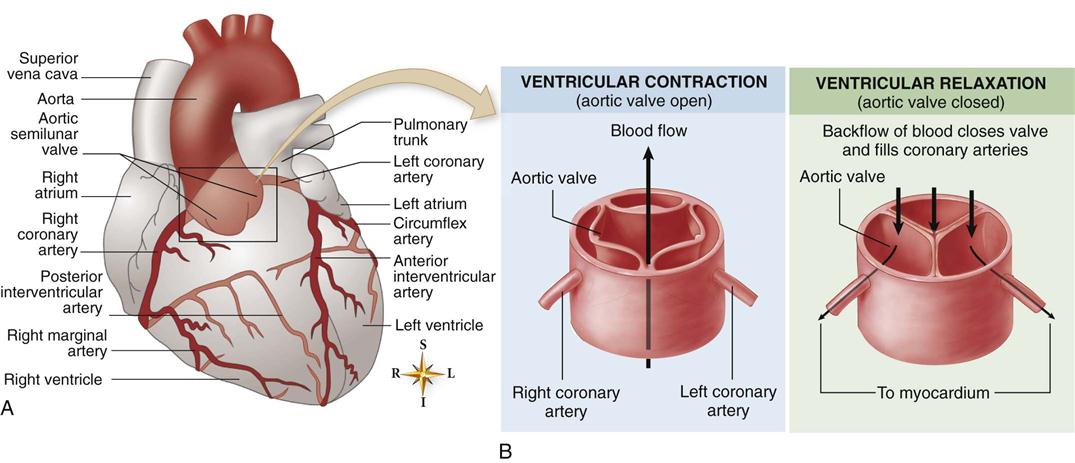
1. Two major arteries, the right and left coronary arteries, branch off the aorta immediately above the aortic valve (Fig. 12-3).
3. Similarly, the right coronary artery follows the right atrioventricular sulcus on the posterior surface of the heart and branches into the right marginal artery and the posterior interventricular artery, and then descends in the posterior interventricular groove toward the apex of the heart, where it comes close to the terminal point of the left anterior descending artery.
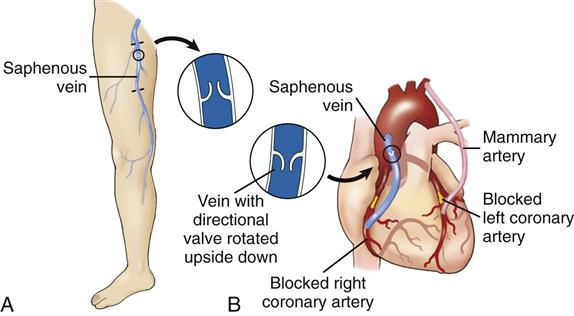
The passage of arteries over the surface of the heart in these grooves is helpful because it permits surgical replacement of obstructed arteries with “bypasses”—using sections of other veins or arteries (see Fig. 12-13 for a diagram of a bypass).
Anastomoses, or direct connections, exist between small branches of the left and right coronary arteries near the apex, as well as in other areas in which branches are nearby (see Fig. 12-3). These junctions have the potential to open up and provide another source of blood to an area. Collateral circulation (alternative source of blood and nutrients) is important if an artery becomes obstructed. When obstruction develops gradually, more capillaries from nearby arteries tend to enlarge or extend into adjacent tissues to meet the metabolic needs of the cells. Regular aerobic exercise contributes to cardiovascular fitness by stimulating the development of collateral channels.
Any interference with blood flow will affect heart function, depending on the specific area supplied by that artery. Generally, the right coronary artery supplies the right side of the heart and the inferior portion of the left ventricle, as well as the posterior interventricular septum. The left anterior descending artery brings blood to the anterior wall of the ventricles, the anterior septum, and the bundle branches, and the circumflex artery nourishes the left atrium and the lateral and posterior walls of the left ventricle. The source of blood for the SA node depends on the specific position of the arteries, which varies in individuals. The SA node is supplied by the right coronary artery in slightly more than half the population and by the left circumflex artery in the remainder. The AV node is nourished primarily by the right coronary artery. This information implies that blockage of the right coronary artery is more likely to result in conduction disturbances of the AV node (resulting in dysrhythmias), whereas interference with the blood supply to the left coronary artery will most likely impair the pumping capability of the left ventricle (potentially leading to congestive heart failure).
The course of the coronary or cardiac veins generally parallels that of the arteries, with the majority of the blood returning to the coronary sinus and emptying directly into the right atrium.
Cardiac Cycle
The cardiac cycle refers to the alternating sequence of diastole, the relaxation phase of cardiac activity, and systole, or cardiac contraction, which is coordinated by the conduction system for maximum efficiency (see Fig. 12-4).
2. The AV valves open as the pressure of blood in the atria increases and the ventricles are relaxed.
3. Blood flows into the ventricles, almost emptying the atria.
6. The two ventricles begin to contract, and pressure increases in the ventricles.
The same volume of blood is pumped from the right and left sides of the heart during each cycle. This is important to ensure that blood flow through the systemic and pulmonary circulations is consistently balanced.
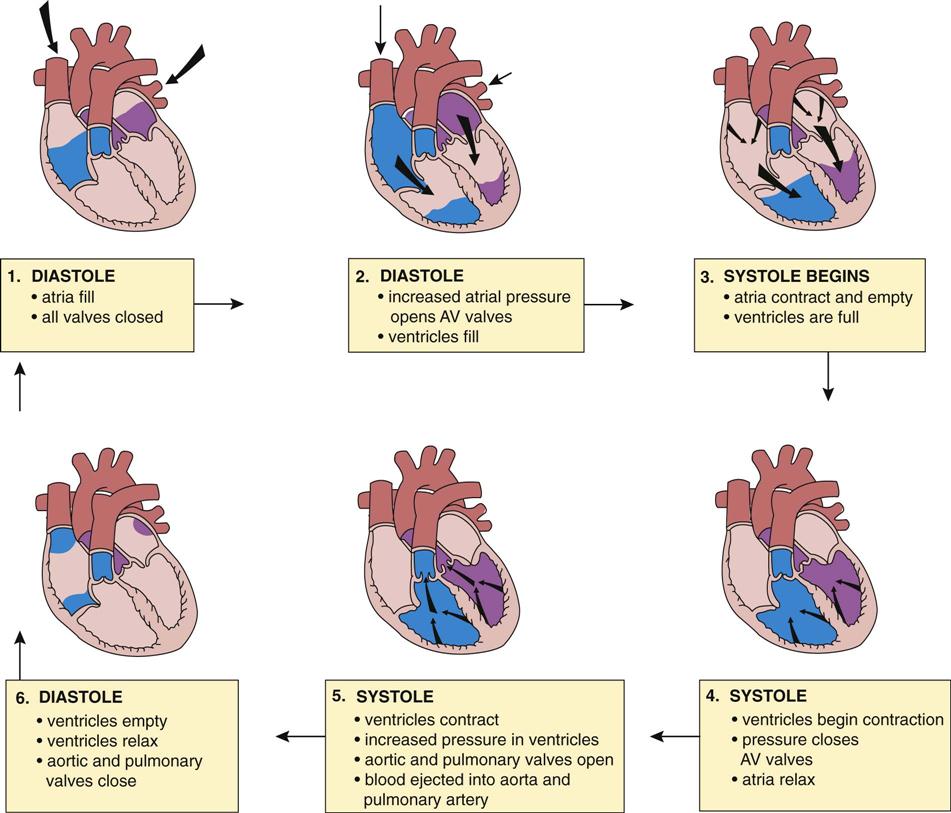
The heart sounds, “lubb-dupp,” which can be heard with a stethoscope, result from vibrations due to closure of the valves. Closure of the AV valves at the beginning of ventricular systole causes a long, low “lubb” sound, followed by a “dupp” sound as the semilunar valves close with ventricular diastole. Defective valves that leak or do not open completely cause unusual turbulence in the blood flow, resulting in abnormal sounds, or murmurs. A hole in the heart septum resulting in abnormal blood flow would also cause a heart murmur.
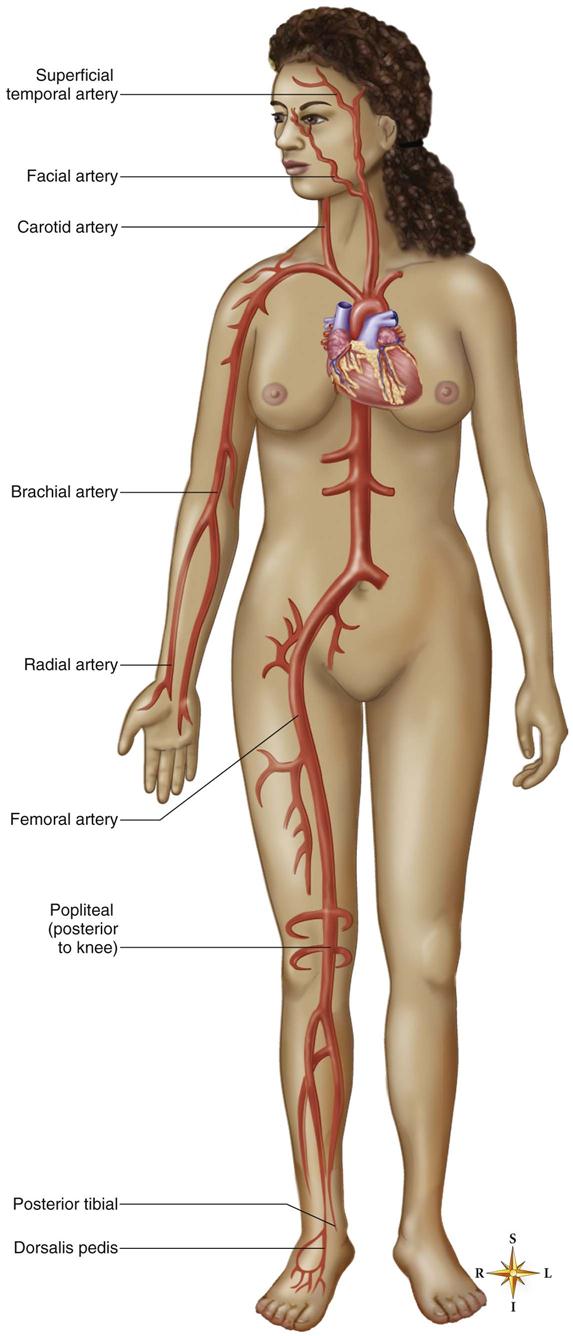
The pulse indicates the heart rate. The pulse can be felt by the fingers (not the thumb) placed over an artery that passes over bone or firm tissue, most commonly at the wrist (Fig. 12-5). During ventricular systole, the surge of blood expands the arteries. The characteristics of the pulse, such as weakness or irregularity in a peripheral pulse (e.g., the radial pulse in the wrist), often indicate a problem. The apical pulse refers to the rate measured at the heart itself. A pulse deficit is a difference in rate between the apical pulse and the radial pulse.
Cardiac function can be measured in a number of ways.
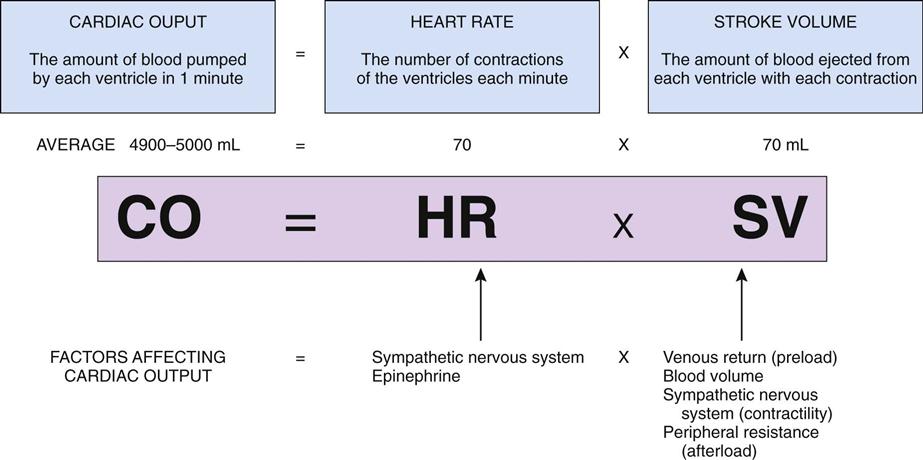
• Cardiac output is the volume of blood ejected by a ventricle in one minute and depends on heart rate and stroke volume, the volume pumped from one ventricle in one contraction) (Fig. 12-6). This means that at rest, the heart pumps into the system an amount equal to the total blood volume in the body every minute, which is a remarkable feat. When necessary, the normal heart can increase its usual output by four or five times the minimum volume.
Blood Pressure
Blood pressure refers to the pressure of blood against the systemic arterial walls. The distribution and structure of the various blood vessels is discussed in detail in Chapter 10. In adults a normal pressure is commonly in the range of 120/70 mmHg at rest. Systolic pressure, the higher number, is the pressure exerted by the blood when ejected from the left ventricle. Diastolic pressure, the lower value, is the pressure that is sustained when the ventricles are relaxed. The brachial artery in the arm is used to measure blood pressure with a sphygmomanometer and an inflatable blood pressure cuff. Pulse pressure is the difference between the systolic and diastolic pressures.
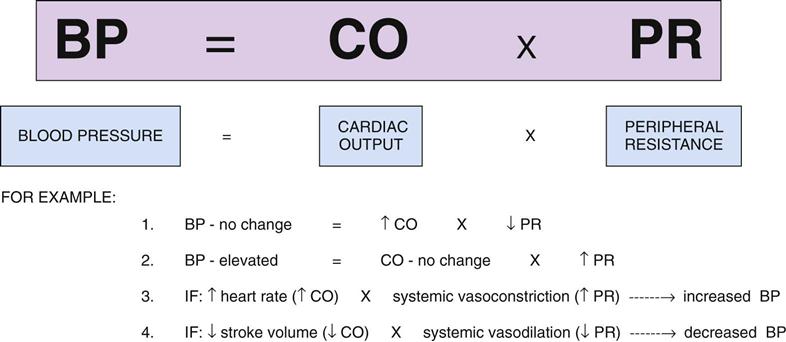
Blood pressure depends on cardiac output and peripheral resistance (Fig. 12-7). Specific variables include blood volume and viscosity, venous return, the rate and force of heart contractions, and the elasticity of the arteries. Peripheral resistance is the force opposing blood flow, or the amount of friction with the vessel walls encountered by the blood. Decreasing the diameter (or lumen) of the blood vessel increases the resistance to blood flow. Normally peripheral resistance can be altered by the systemic constriction or dilation of the arterioles. Systemic or widespread vasoconstriction occurs in response to sympathetic stimulation and increases blood pressure. Systemic or general vasodilation that leads to decreased blood pressure results from reduced SNS stimulation. (There is no parasympathetic nervous system innervation in the blood vessels.) Any obstruction in the blood vessel also increases resistance. Local vasoconstriction or dilation does not affect the overall systemic blood pressure.
Changes in blood pressure are detected by the baroreceptors and relayed to the vasomotor control center in the medulla, which adjusts the distribution of blood to maintain normal blood pressure. For example, when one rises from a supine position, blood pressure drops momentarily owing to gravitational forces until the reflex vasoconstriction mechanism in the body ensures that more blood flows to the brain.
Blood pressure is elevated by increased SNS stimulation in two ways:
Other hormones also contribute to the control of blood pressure:
• Aldosterone increases blood volume by increasing reabsorption of sodium ions and water.
• The renin-angiotensin-aldosterone system in the kidneys is an important control and compensation mechanism that is initiated when there is any decrease in renal blood flow. This stimulates the release of renin, which in turn activates angiotensin (vasoconstrictor) and stimulates aldosterone secretion (see Chapter 18). Angiotensin II is a powerful vasoconstrictor.
Heart Disorders
Heart disease is ranked as a major cause of morbidity and mortality in North America. Common heart diseases include congenital heart defects, hypertensive heart disease, angina and heart attacks, cardiac arrhythmias, and congestive heart failure. There is increasing emphasis on routine preventive measures for all individuals, with a focus on factors such as a healthy diet, regular exercise, moderation in alcohol intake, cessation of smoking, safe sexual practices, immunizations, monitoring body weight and blood pressure, and basic screening tests for cholesterol levels and the presence of cancer.
Diagnostic Tests for Cardiovascular Function
Because many of the same tests are used in the diagnosis and monitoring of a variety of cardiovascular disorders, a few of the basic tests are summarized here.
• An ECG is useful in the initial diagnosis and monitoring of arrhythmias, myocardial infarction, infection, and pericarditis (see Fig. 12-17). It is a noninvasive procedure and can illustrate the conduction activity of the heart as well as the effects of systemic abnormalities such as serum electrolyte imbalance. A portable Holter monitor may be worn by an individual to record ECG changes while he or she pursues daily activities. A log of activities is usually maintained to match with the changes in ECG. A normal baseline ECG recording is recommended for everyone; it can be used for comparison if cardiovascular disease ever develops.
• Valvular abnormalities or abnormal shunts of blood cause murmurs that may be detected by auscultation of heart sounds by means of a stethoscope. A recording of heart sounds may be made with a phonocardiograph. In echocardiography, ultrasound, or reflected sound waves, is used to record the image of the heart and valve movements (see Fig. 12-25). These tests provide useful information regarding valvular abnormalities, congenital defects, and changes in heart structure or function.
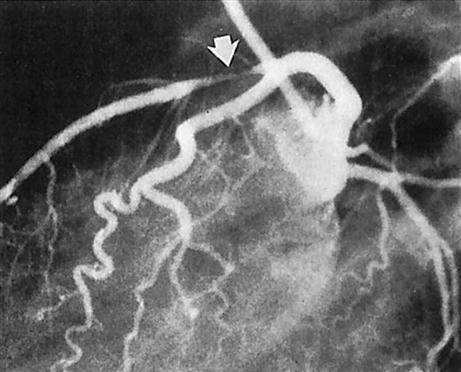
• Blood flow in the coronary arteries can be visualized with coronary angiography (Fig. 12-8). Current research using very tiny ultrasound instruments within the vessels has proved more effective in diagnosing obstructions. Obstructions can be assessed and then treated with the basic catheterization procedure, with injected thrombolytic agents or laser therapy to break down clots, or balloon angioplasty to open a narrow coronary artery mechanically.
Other specific tests are mentioned under the appropriate topic and in Ready Reference 5 at the back of the book. More specialized tests may be necessary.
General Treatment Measures for Cardiac Disorders
Because some treatment measures apply to many disorders, a number of common therapies are covered here. Additional specific treatment modalities are mentioned with the disorder to which they apply.
4. Drug therapy is an important component in the maintenance of cardiac patients. Many individuals take several drugs. Common medications include:
• Diuretics remove excess sodium and water from the body through the kidneys by blocking the reabsorption of sodium or water (see Chapter 18). Patients often refer to them as “water pills.” They are useful drugs in the treatment of high blood pressure and congestive heart failure because they increase urine output, reducing blood volume and edema. Examples are hydrochlorothiazide, a mild diuretic, and furosemide, a more potent drug. These diuretics may also remove excessive potassium from the body, requiring supplements to prevent hypokalemia. Spironolactone is an example of a “potassium-sparing” diuretic.
• Anticoagulants or “blood thinners” may be used to reduce the risk of blood clot formation in coronary or systemic arteries or on damaged or prosthetic heart valves. In many cases, a small daily dose of aspirin (ASA) is recommended to decrease platelet adhesion. Oral anticoagulants such as warfarin (Coumadin) may be taken by individuals in high-risk groups. These drugs block the coagulation process (see Fig. 10-9). Individuals must be cautious about taking other medication, including nonprescription drugs, drinking alcohol, and making dietary changes, and avoid potentially traumatic activities. It is essential to monitor clotting ability, measuring prothrombin time or activated partial thromboplastin time closely in these patients to prevent hemorrhage and to observe patients for increased bleeding tendencies (see blood clotting in Chapter 10).
Table 12-1 provides a summary of common cardiovascular drugs. A drug index may be found in Ready Reference 8 at the back of the book.
TABLE 12-1
| Name | Use | Action | Adverse Effects |
| Nitroglycerin | Angina attacks and prophylaxis | Reduces cardiac workload, peripheral and coronary vasodilator | Dizziness, headache |
| Metoprolol (Lopressor) | Hypertension, angina, antiarrhythmic | Blocks beta-adrenergic receptors, slows heart rate | Dizziness, fatigue |
| Nifedipine (Adalat) | Angina, hypertension, peripheral vasodilator, antiarrhythmic | Calcium blockers, vasodilator | Dizziness, fainting, headache |
| Digoxin (Lanoxin) | Congestive heart failure and atrial arrhythmias | Slows conduction through AV node and increases force of contraction (cardiotonic) to increase efficiency | Nausea, fatigue, headache, weakness |
| Enalapril (Vasotec) | Hypertension | ACE inhibitor—blocks formation of angiotensin II and aldosterone | Headache, dizziness, hypotension |
| Furosemide (Lasix) hypertension | Edema with CHF, hypertension | Diuretic—increases excretion of water and sodium | Nausea, diarrhea, dizziness |
| Simvastatin (Zocor) | Hypercholesteremia (CHD) | Decreases cholesterol and LDL | Digestive discomfort |
| Warfarin (Coumadin) | Prophylaxis and treatment of thromboemboli | Anticoagulant—interferes with vitamin K in synthesis of clotting | Excessive bleeding (antidote: vitamin K) |
| ASA (aspirin) | Prophylaxis of thromboemboli | Prevents platelet adhesion, anti-inflammatory | Gastric irritation, allergy |
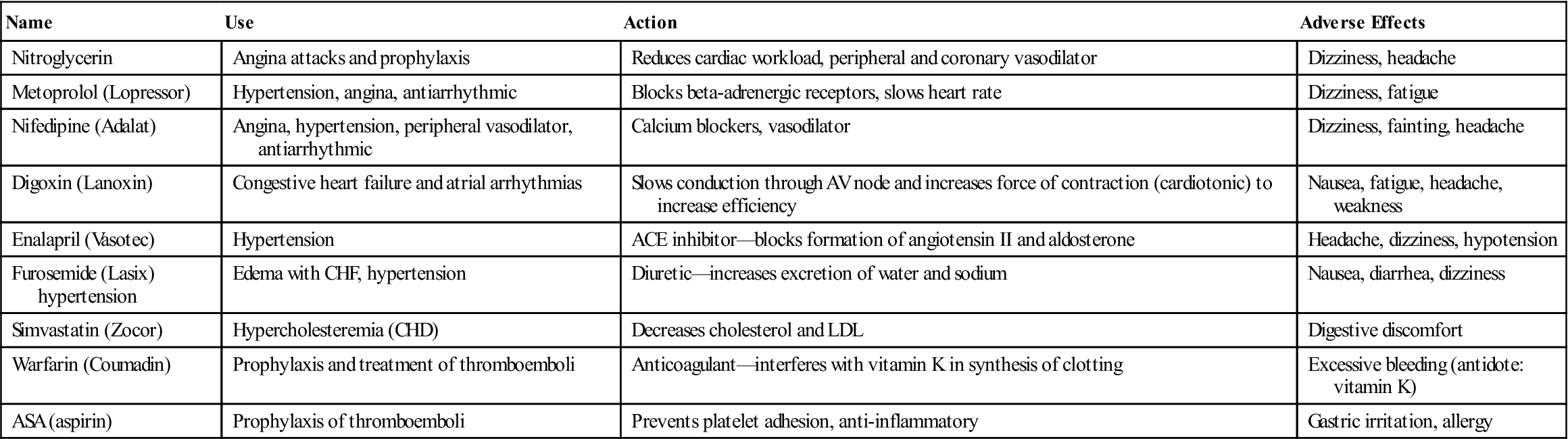
CHD, Coronary heart disease; CHF, congestive heart failure; LDL, low-density lipoprotein.
Coronary Artery Disease or Ischemic Heart Disease or Acute Coronary Syndrome
Sometimes called coronary heart disease, coronary artery disease includes angina pectoris or temporary cardiac ischemia and myocardial infarction or heart attack. Myocardial infarction results in damage to part of the heart muscle because of obstruction in a coronary artery. The basic problem is insufficient oxygen for the needs of the heart muscle.
A common cause of disability and death, coronary artery disease may ultimately lead to heart failure, serious dysrhythmias, or sudden death. It is the leading cause of death in men and women in the United States, causing approximately 385,000 deaths each year. Statistics for 2009 reveal that one in four deaths are the result of some form of heart disease, and the incidence for new or repeated heart attacks is 935,000 Americans. It is estimated that 13.2 million live with coronary artery disease in the United States. An additional 6 million are currently diagnosed with congestive heart failure (there is some overlap within these figures). The CDC reported that in 2008, high blood pressure was listed as a factor in 348,000 deaths and affects 68 million Americans. Males tend to develop heart disease at an earlier age than women, but women tend to have more complications likely due to later diagnosis. The current statistics show a decrease in numbers of individuals being diagnosed with heart disease, which many attribute to prevention awareness programs.
Arteriosclerosis and Atherosclerosis
Pathophysiology
Arteriosclerosis can be used as a general term for all types of arterial changes. It is best applied to degenerative changes in the small arteries and arterioles, commonly occurring in individuals over age 50 and those with diabetes. Elasticity is lost, the walls become thick and hard, and the lumen gradually narrows and may become obstructed. This leads to diffuse ischemia and necrosis in various tissues, such as the kidneys, brain, or heart.
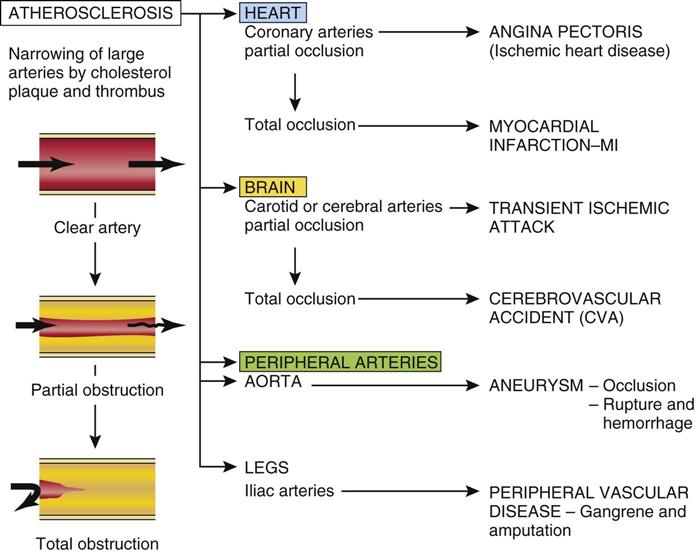
Atherosclerosis is differentiated by the presence of atheromas, plaques consisting of lipids, cells, fibrin, and cell debris, often with attached thrombi, which form inside the walls of large arteries. Note in Figure 12-9 how the unaffected artery is smooth, and the openings to branch arteries are clearly defined. By comparison, the atherosclerotic artery has a very rough, elevated surface, with loose pieces of plaque and thrombus, and the openings to branching arteries are blocked. Atheromas form primarily in the large arteries, such as the aorta and iliac arteries, the coronary arteries, and the carotid arteries, particularly at points of bifurcation, where turbulent blood flow may encourage the development of atheromas.
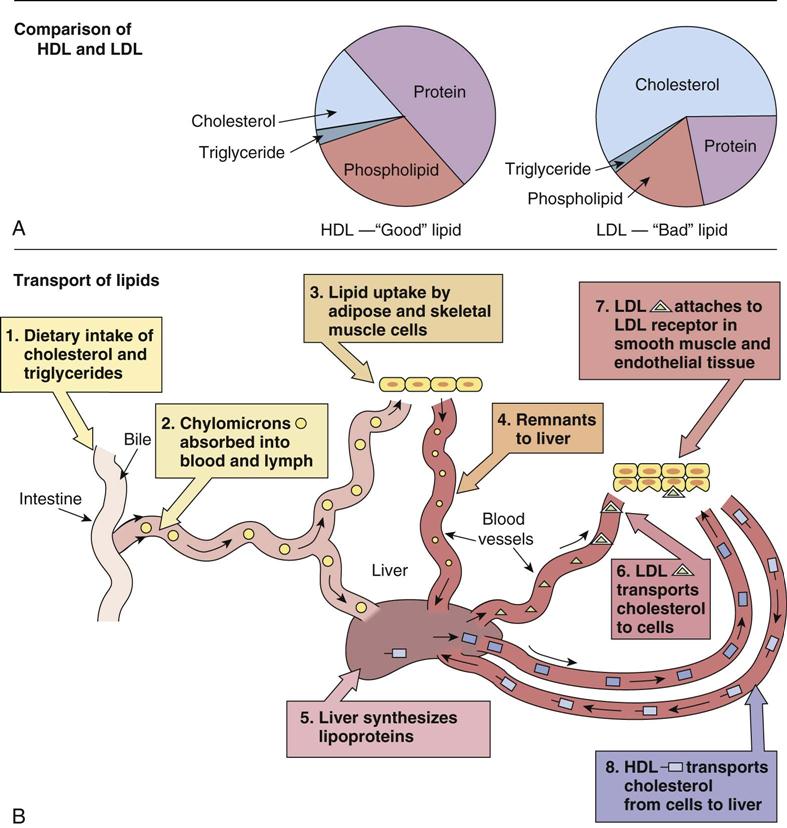
Lipids or fats, which are usually transported in various combinations with proteins (lipoproteins), play a key role in this process (Fig. 12-10). Lipids, including cholesterol and triglycerides, are essential elements in the body and are synthesized in the liver; therefore they can never be totally eliminated from the body.
Analysis of serum lipids includes assessment of all the subgroups (total cholesterol, triglycerides, low-density lipoproteins, and high-density lipoproteins) because the proportions indicate the risk factor for the individual. The serum lipids of particular importance follow:
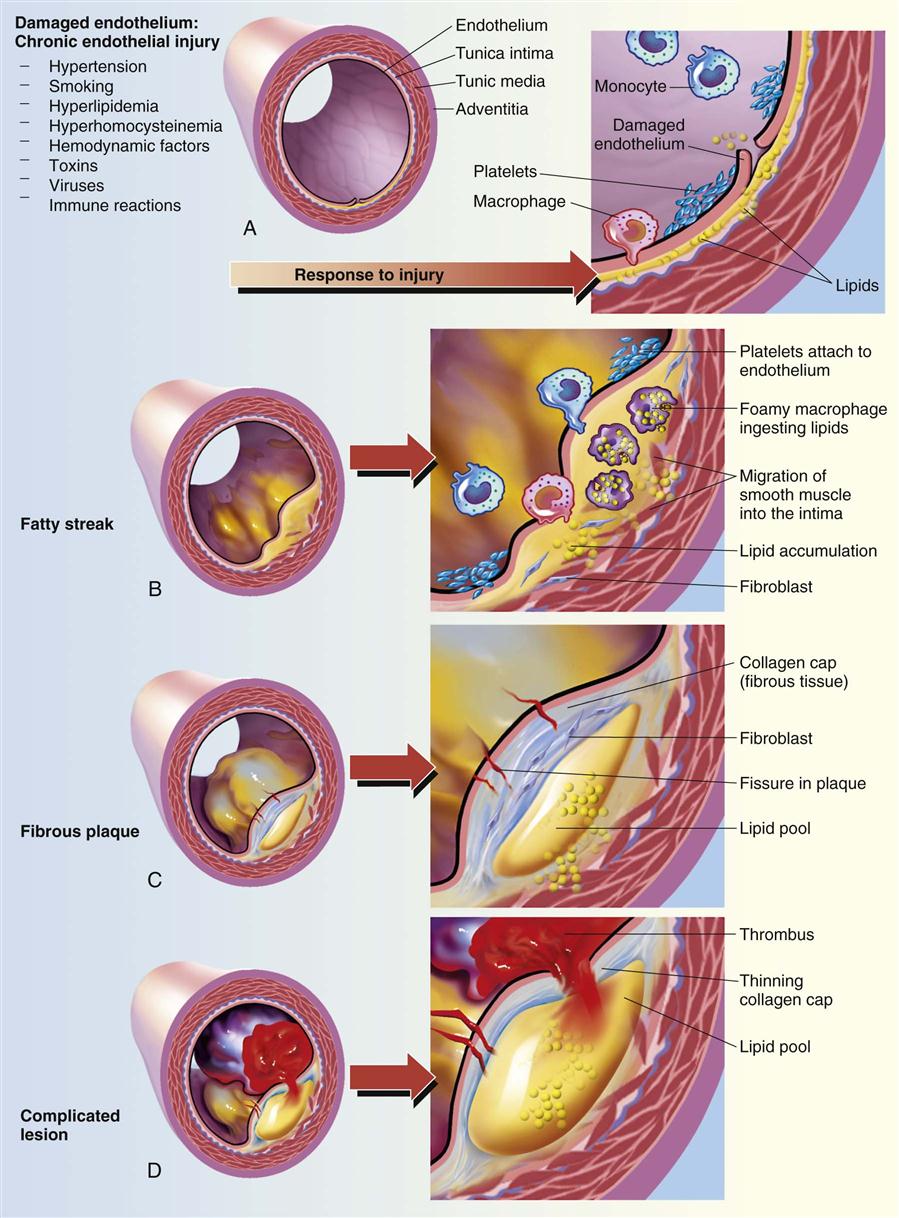
The process appears to begin with endothelial injury in the artery, often at a very young age. Endothelial injury causes inflammation in the area, leading to elevated C-reactive protein (CRP) levels. White blood cells, particularly monocytes and macrophages, and lipids accumulate in the intima, or inner lining, of the artery and in the media, or muscle layer. Smooth muscle cells proliferate or multiply (Fig. 12-11). Thus, a plaque forms and inflammation persists. Platelets adhere to the rough, damaged surface of the arterial wall, forming a thrombus and partial obstruction of the artery.
Lipids continue to build up at the site of arterial injury, along with fibrous tissue. Platelets adhere and release prostaglandins, which precipitate inflammation and vasospasm. This draws more platelets to aggregate at the site, enlarging the thrombus. Arterial flow becomes more turbulent, again promoting thrombus formation. A vicious cycle persists. Blood flow progressively decreases as the lumen narrows. At some point, the plaque may ulcerate and break open. This may precipitate more inflammation or a thrombus may form at this site, resulting in total obstruction in a very short time. This may be the precipitating factor for myocardial infarction.
The atheroma also damages the arterial wall, weakening the structure and decreasing its elasticity. In time, atheromas may calcify, causing further rigidity of the wall. This process may lead to aneurysm, a bulge in the arterial wall (see Fig. 12-34), or to rupture and hemorrhage of the vessel.
Initially the atheroma manifests as a yellowish fatty streak on the wall. It becomes progressively larger, eventually becoming a large, firm projecting mass with an irregular surface on which a thrombus easily forms. As the atheroma increases in size and the coronary arteries are partially obstructed, angina (temporary myocardial ischemia) may occur; a total obstruction leads to myocardial infarction. Atheromas are also a common cause of strokes, renal damage, and peripheral vascular disease, which affects the legs and feet (Fig. 12-12).
Etiology
The cause of atherosclerosis appears to be multifactorial, and some of the factors are synergistic, enhancing the total effect. There are two groups of risk factors for atherosclerosis, one group that can be modified to some extent and one that cannot.
The factors that cannot be changed (nonmodifiable) include:
• Age, with atherosclerosis more common after age 40 years, particularly in men
• The other group of predisposing factors are modifiable. These include factors such as:
• Obesity or diets high in cholesterol and animal fat, which elevate serum lipid levels, especially LDL. The significant increase in obesity in children is of great concern with regards to a relative increase in cardiovascular disease in the coming years. The Centers for Disease Control and Prevention estimate that more than12.5 million children and adolescents under age 19 in the United States are obese and at risk of metabolic syndrome. Data collected in the United States for 2011 also indicated that 35.7% of adult men and women were clinically obese. Obesity is the primary indicator of metabolic syndrome, which is directly linked with the development of coronary artery disease in adulthood (see Chapter 23).
• Poorly controlled hypertension, which causes endothelial damage
• Combination of some oral contraceptives and smoking
Diagnostic Tests
Serum lipid levels, including those of LDL and HDL, should be checked to identify the patient’s risk and monitor the efficacy of treatment. Serum levels of high-sensitivity CRP indicate the presence of inflammation, indicating increased risk. However, CRP may be elevated due to other chronic inflammatory disease. Low CRP levels appear to indicate a low risk of developing cardiovascular disease. Exercise stress testing can be used for screening or to assess the degree of obstruction in arteries. Nuclear medicine studies can be used to determine the degree of tissue perfusion, the presence of collateral circulation, and the degree of local cell metabolism. To minimize risk and promote early diagnosis and treatment, the acceptable range for test results may be modified or lowered as new evidence becomes available.
Treatment
3. Sodium intake should be minimized as well to control hypertension.
4. Control of primary disorders such as diabetes or hypertension is important.
8. When atheromas are advanced, surgical intervention (percutaneous transluminal coronary angioplasty may be required to reduce obstruction by means of invasive procedures requiring cardiac catheterization. The catheter contains an inflatable balloon that flattens the atheroma. Newer techniques use laser angioplasty, a laser beam, and fiberoptic technology with a catheter. The high-energy laser causes the obstruction to disintegrate into microscopic particles that are removed by macrophages. There appears to be less risk of recurrence with this method. Stents, small tube-like structures, may be inserted into arteries after angioplasty, to maintain an opening. Surgery such as coronary artery bypass grafting (CABG) to reroute blood flow around the obstruction, using veins or the left internal mammary artery for a graft, appears to have an improved long-term prognosis (Fig. 12-13). A graft can also be placed around an obstructed aorta. Less invasive means of CABG are currently being used in some patients.
Angina Pectoris
Pathophysiology
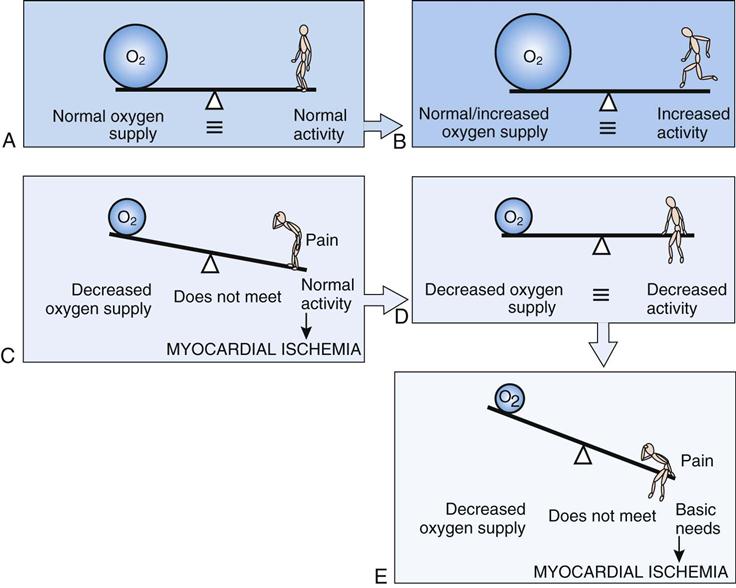
Angina, or chest pain, occurs when there is a deficit of oxygen to the heart muscle. This can occur when the blood or oxygen supply to the myocardium is impaired, when the heart is working harder than usual and needs more oxygen, or when a combination of these factors is present (Fig. 12-14). Usually the heart can adapt its blood supply to its own needs by vasodilation (autoregulation) unless the vessel walls are damaged or cannot relax. The reduced blood supply may be due to partial obstruction by atherosclerosis or spasm in the coronary arteries. When the supply and demand for oxygen are marginally balanced, an increase in cardiac demand with any physical or emotional exertion can cause a relative deficit of oxygen to the myocardium.
Chest pain may occur in a variety of patterns: classic or exertional angina; variant angina, in which vasospasm occurs at rest; and unstable angina, a more serious form. Unstable angina refers to prolonged pain at rest and of recent onset, perhaps the result of a break in an atheroma. This may precede a myocardial infarction. Most commonly, an episode of anginal pain occurs when the demand for oxygen increases suddenly, with exertion. In most cases, no permanent damage to the myocardium results from angina unless the episodes are frequent, prolonged, and severe.
Etiology
Insufficient myocardial blood supply is associated with atherosclerosis, arteriosclerosis, vasospasm (a localized contraction of arteriolar smooth muscle), and myocardial hypertrophy, in which the heart has outgrown its blood supply. Severe anemias and respiratory disease can also cause an oxygen deficit. Increased demands for oxygen can arise in circumstances such as tachycardia associated with hyperthyroidism or the increased force of contractions associated with hypertension.
Precipitating factors of angina attacks are related to activities that increase the demands on the heart, such as running upstairs, getting angry, respiratory infection with fever, exposure to weather extremes or pollution, or eating a large meal.
Signs and Symptoms
Angina occurs as recurrent, intermittent brief episodes of substernal chest pain, usually triggered by a physical or emotional stress that increases the demand by the heart for oxygen. Pain is described as a tightness or pressure in the chest and may radiate to the neck and left arm. Often pallor, diaphoresis (excessive sweating), and nausea are also present. Attacks vary in severity and last a few seconds or minutes.