Yolk Sac Tumor
Steven S. Shen, MD, PhD
Mahul B. Amin, MD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Germ cell tumor characterized by variety of growth patterns that recapitulate yolk sac, allantois, and extraembryonic mesenchyme
Clinical Issues
Most common germ cell tumor of infants and young children
No association with cryptorchidism
Pure form rare in adults: Usually present as component of mixed germ cell tumors
Microscopic Pathology
YST has multiple growth patterns with 1 dominant pattern or more frequently mixed patterns
Reticular or microcystic pattern most frequent (80%)
Other common patterns include endodermal sinus, solid, papillary, and glandular
Relatively uniform cells with clear or vacuolated to lightly eosinophilic cytoplasm
Bland cuboidal, columnar to flattened, or spindle cells
Presence of small, spherical, intracellular or extracellular hyaline globules
Prominent basement membrane deposition
Ancillary Tests
Positive for cytokeratin, AFP, PLAP (variable), SALL4, glypican-3
Negative for CD30(BerH2), Podoplanin(D2-40), Oct3/4, hCG, inhibin-α
Podoplanin(D2-40) and Oct3/4 are positive in seminoma and embryonal carcinoma
TERMINOLOGY
Abbreviations
Yolk sac tumor (YST)
Synonyms
Endodermal sinus tumor (EST)
Definitions
Germ cell tumor characterized by variety of growth patterns that recapitulate yolk sac, allantois, and extraembryonic mesenchyme
CLINICAL ISSUES
Epidemiology
Incidence
Pure YST is most common testicular tumor of infants and young children
Accounts for 75% of all childhood testicular neoplasms
No association with cryptorchidism or other germ cell tumor components
Pure YST is extremely rare in adult testes
At extragonadal sites, especially mediastinum, pure YST may be seen
YST is frequent component of mixed germ cell tumors (in ~ 40%) in adults
Age
Mean age: 16-18 months for pure YST
Mean age: 25-35 years for adult YST
10 years younger than patients with seminoma
Presentation
Nonsymptomatic, rapid testicular enlargement
Approximately 90% of patients with childhood YST have clinical stage I disease
Presence of YST in adult patients with mixed germ cell tumor is frequently associated with lower stage presentation
Laboratory Tests
More than 95% patients have elevated serum α-fetoprotein (AFP)
Test for serum AFP is valuable tool in diagnosis and monitoring effectiveness of therapy
Treatment
For infants and children with pure YST
Radical inguinal orchiectomy for stage I tumor with close follow-up protocol (surveillance)
Cisplatin-based therapy for relapse on surveillance, advanced stage disease, or metastasis
For adult YST (usually mixed with other germ cell tumor)
Similar to other nonseminomatous germ cell tumor based on clinical stage
Radical inguinal orchiectomy ± retroperitoneal lymph node dissection
Cisplatin-based chemotherapy for metastatic disease
Prognosis
Prognosis associated with clinical stage, lymphovascular invasion, degree of serum AFP elevation
Children have better prognosis than adults
IMAGE FINDINGS
General Features
Ultrasonography may detect scrotal mass
MACROSCOPIC FEATURES
General Features
Nonencapsulated, gray-white, soft or firm, homogeneous mass
Typical myxoid or gelatinous cut surface
Hemorrhage and necrosis may be present
Tumors in adults are typically more heterogeneous
Size
Range: 2-6 cm
MICROSCOPIC PATHOLOGY
Histologic Features
YST frequently has multiple growth patterns with 1 dominant pattern
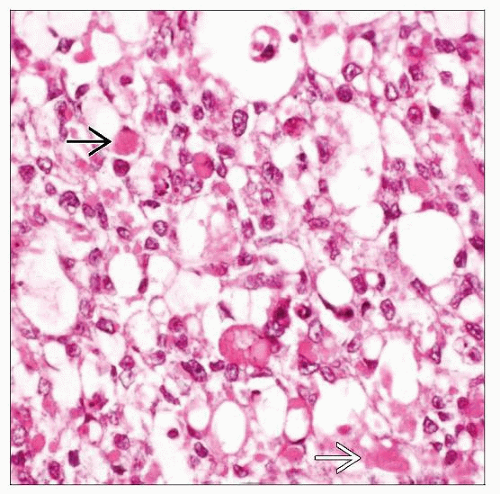
Microcystic or reticular pattern most frequent (80%)
Anastomosing thin cords forming round or irregular spaces or tubules of variable size
Characteristic intracellular vacuoles and merging of cells create sieve-like appearance
Nuclei are irregularly shaped (round, columnar, stellate, triangular) and are often pushed to edge of cells
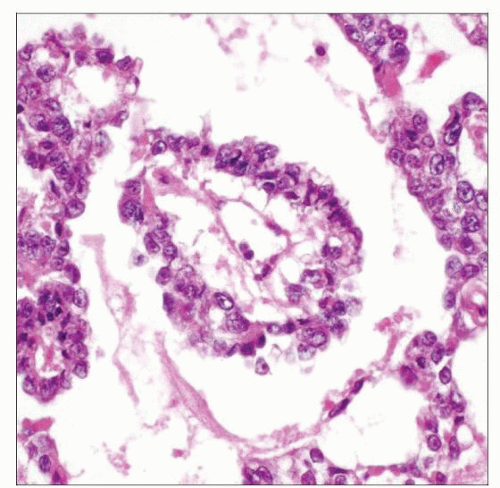
Endodermal sinus pattern
Composed of numerous Schiller-Duval bodies (resembling fetal glomeruli) with central fibrovascular core
Fibrovascular core is lined by cuboidal to columnar tumor cells, which are surrounded by cystic spaces and more flattened layer of tumor cells
Labyrinthine spaces or perivascular arrangement of tumor cells are common
Solid pattern
Solid sheets of polygonal tumor cells with pale eosinophilic or clear cytoplasm, which lack fibrovascular septae, lymphocytes, or granulomas
May be confused with seminoma, embryonal carcinoma, and monophasic areas of choriocarcinoma
Tumor cells with random pleomorphism; slightly greater atypia than seminoma but less than embryonal carcinoma
Papillary and tubulopapillary
Papillae ± central fibrovascular cores
Tumor cells are often cuboidal and low columnar with “hobnail” appearance
Polyvesicular vitelline pattern
Large constricted vesicles lined by flattened to cuboidal cells
Often associated with abundant myxoid or loosely fibrous stroma
Glandular-alveolar pattern
Simple round to complex branching glands with intervening myxoid stroma
Parietal pattern
Epithelial cells surrounded by pink bands of basement membrane material
Enteric or endometrioid pattern
Glandular pattern with columnar cells, cytoplasmic clearing, subnuclear vacuoles, and smooth luminal surface
Hepatoid pattern
Sheets of tumor cells with abundant eosinophilic cytoplasm and eosinophilic globules
Spindled cell or sarcomatoid pattern
Composed of spindle (or sarcomatoid) cells with myxoid stroma
Myxomatous pattern
Epithelioid to spindle cells dispersed in paucicellular light blue myxoid stroma
Frequently under-recognized due to innocuous appearance
Macrocystic pattern
Large cystic spaces due to coalescence of microcysts lined by flattened tumor cells
Mixed pattern
Mixture of any of above growth patterns
Intra- and extracellular PAS-positive hyaline globules
More commonly seen in microcystic and reticular, solid, and hepatoid patterns
Cytologic Features
Relatively uniform epithelioid cells with clear or vacuolated to pale eosinophilic cytoplasm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree