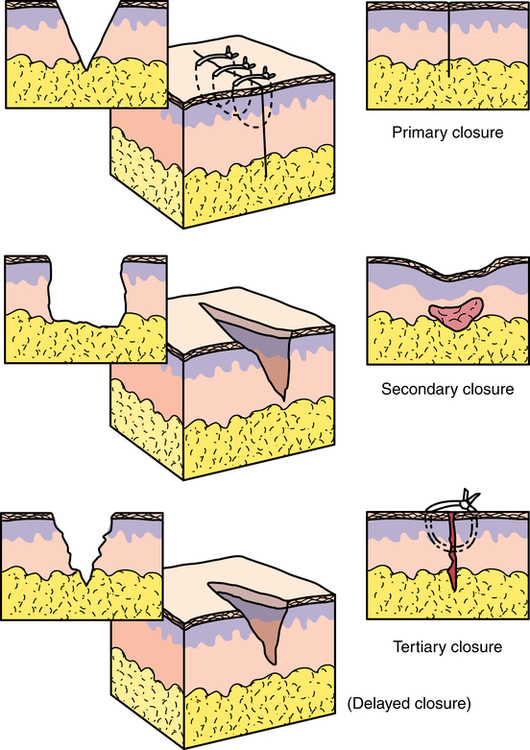
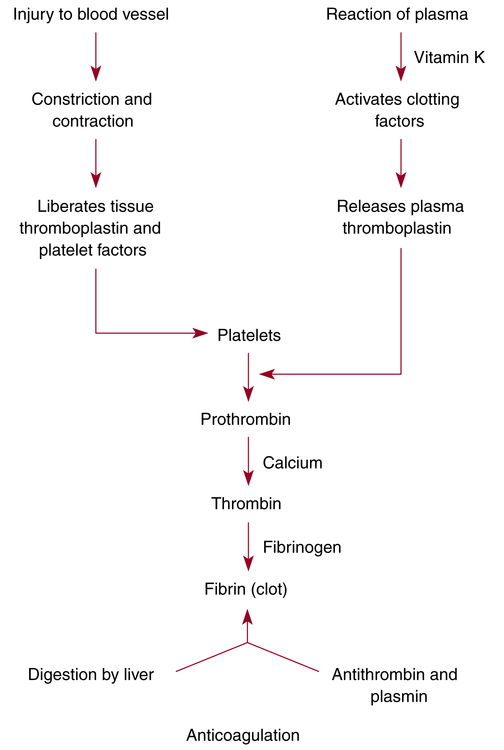
Chapter 29 After studying this chapter, the learner will be able to: • Identify tissue layers specific to the anatomic site of a wound. • List several factors that affect wound healing. • Describe the three mechanisms of wound healing. • List three complications of wound healing. Band of scar tissue that holds together or unites surfaces or structures that are normally separated. Firm avascular scar tissue. Formation of extensive scar tissue over a joint. Space caused by separation of wound edges or by air trapped between layers of tissue. Removal of damaged tissue and cellular or other debris from a wound to promote healing and to prevent infection. Partial or total splitting open or separation of the layers of a wound. Tissue that is nonviable, necrotic. Abnormal accumulation of fluid in interstitial spaces of tissues. Protrusion of viscera through an abdominal incision. Tissue is drained of blood. Passage of blood, serum, or lymph into tissues. Fluid, cells, or other substances that have been discharged from vessels or tissues. It contains white blood cells, lymphokines, and growth factors that stimulate healing.7 Formation of fibrous collagen to fill the gap between the edges of a wound healing with contraction (i.e., second intention). Inflammatory lesion that forms around a foreign substance, such as glove powder or a suture knot. Collection of extravasated blood in tissue. Arrest of blood flow or hemorrhage; the mechanism is via coagulation (formation of a blood clot). Excessive raised dense scarring that does not exceed the border of the wound. Condition caused by treatment or procedure performed by medical personnel. Intentional cut through intact tissue (synonym: surgical incision). Decrease of blood supply to tissues. Overgrowth of firm rounded scar that extends beyond the border of the wound. Can be painful and may bleed if injured. Death of tissue cells; devitalized tissue. Deposition of fibrous connective tissue to bridge separated wound edges and to restore continuity of tissues. Collection of extravasated serum from interstitial tissue or a resolving hematoma in tissue. Ability of tissues to resist rupture. Immune response of the body to tissue injury or foreign substances. Separation of wound edges. Interruption of tissue integrity, either intentional or unintentional, requires understanding of the mechanism and factors that cause wounding and influence wound healing.3,7,8 When tissue is cut, the body’s inherent defense mechanisms respond immediately to begin repair. Three mechanisms of wound healing are recognized: first intention/primary union, second intention, and third intention/delayed primary closure (Fig. 29-1).3 Each mechanism has practical applications in the making and closing of incisions or traumatic wounds. The degree of contamination and the amount of viable tissues are factors in the determination of which method of healing is used. • Well-approximated edges with suture, wound sealant, or wound-closure strips • Minimal or no postoperative swelling • No serous discharge or local infection • No separation of wound edges 1. Lag phase of acute inflammatory response: Tissue fluids containing plasma, proteins, blood cells, fibrin, and antibodies exude from the tissues into the wound, depositing fibrin, which weakly holds the wound edges together for the first 5 days. Fibrin and serum protein dry out and form a scab that seals the wound from further fluid loss and microbial invasion. At the same time, fibroblasts, fibrous tissue germ cells, and epithelial cells migrate from the general circulation. Subsequent adhesion of these cells, a process known as fibroplasia, holds the wound edges together. Leukocytes and other white blood cells produce proteolytic enzymes to dissolve and remove damaged tissue debris. Macrophages and neutrophils ingest foreign material, cellular debris, and bacteria. 2. Healing or proliferative phase of fibroplasia: After the fifth postoperative day, fibroblasts multiply rapidly, bridging wound edges and restoring the continuity of body structures. Collagen, a protein substance that is the chief constituent of connective tissue, is secreted from the fibroblasts and formed into fibers. Reepithelialization causes the rapid gain in tensile strength and pliability of the healing wound. Tensile strength is the ability of the tissues to resist rupture. The healing phase begins rapidly, diminishes progressively, and terminates on about the 14th day. It may continue for up to 20 days. 3. Maturation or differentiation phase: From the 14th postoperative day until the wound is fully healed, scar formation occurs by deposition of fibrous connective tissue. The collagen content remains constant, but the fiber pattern reforms and crosslinks to increase the tensile strength. Wound contraction occurs over a period of weeks up to 6 months. As collagen density increases, vascularity decreases and the scar grows pale. The scar tissue is only 80% as strong as the original tissue. 1. Infection, excessive trauma, loss of tissue, and poorly approximated tissue are common. Inflammatory response is exaggerated. 2. The wound is left open and allowed to heal from the inner toward the outer surface. Devitalized tissue is debrided. a. In some wounds, the use of maggot therapy is useful for debridement.2 b. Debridement of devitalized tissue can be performed with scissors or a knife. c. The wound can be packed with dressing material that attaches to the necrotic tissue. When the packing is removed, the dead tissue separates from the wound bed. 3. Healing is delayed. The wound may need grafting. 4. Healing may produce a weak union, which may be conducive to incisional herniation later. 5. The risk of secondary infection is proportional to the amount of necrotic tissue present in the wound and to compromised immune response in the patient. Repeated debridement may be necessary. 6. Scar formation is excessive. 7. Contracture of skin is pronounced. After healing is complete, the scar may need revision or release. 1. The wound is cleaned and debrided. 2. The defect is packed with moist gauze to promote drainage and granulation. 3. Antibiotic therapy is implemented. 4. The wound may be an old traumatic or septic wound. 5. The area should not be devascularized, and deep sutures should be avoided. Granulomas can form. 6. Two clean surfaces of granulation tissue are brought together for later closure. A wound is an injury, either intentional or unintentional, that disrupts the continuity of body tissues with or without tissue loss. Wounds may be surgical (intentional), traumatic, incidental, or chronic.10 According to the Centers for Disease Control and Prevention (CDC), risk of infection increases in proportion to contamination of the incision and surrounding tissues exposed during the course of the surgical procedure. The true extent of risk cannot be evaluated until the procedure is completed. The wound is classified at the end of the surgical procedure as one of four types (Box 29-1): Vasoconstriction caused by smoking decreases blood supply and oxygenation to the wound.11 Carbon monoxide in smoke binds with hemoglobin (forming carboxyhemoglobin) and further diminishes oxygenation. Smoking contributes to respiratory complications. This can cause forceful coughing that can raise intraabdominal pressure and create increased strain on an abdominal wound and impair healing. Complete hemostasis must be achieved to prevent loss of blood and to prevent hematoma (blood clot) formation. Blood loss is caused by tissue trauma. The method of dissection and coagulation of bleeders can cause devitalization of tissue. Devitalized tissue cannot heal; it only necroses. Delivery of oxygen to healing tissues is affected. Any condition that lowers circulating blood flow and the delivery of oxygen to the tissues impairs healing.12 Tissue edges are brought together with precision, avoiding strangulation and eliminating dead space, to promote wound healing. A closure that is too tight or closure under tension causes ischemia, a decrease of blood supply to tissues. Approximation is critical to the healing of flaps and grafts. Constricted or interrupted blood supply can cause flap failure or loss of a vascularized graft.13 • Early ambulation improves circulation, which aids in the healing process and eliminates stasis of blood, which may result in thrombus and embolus formation. • The patient is better able to cooperate in deep-breathing exercises to raise bronchial secretions; thus, pulmonary complications are reduced. • Early ambulation decreases gas pain, distention, and the tendency toward nausea and vomiting. It helps prevent constipation. Bodily functions return to normal more readily. • Increased exercise aids digestion. Thus, the patient’s oral intake progresses sooner after the surgical procedure, so that less supplementary intravenous fluid is necessary for hydration and nutrition. • Early ambulation eliminates the general muscle weakness that follows bed rest. • Fewer pain-relieving drugs are necessary. • Early ambulation boosts patients’ morale with the knowledge that they will be out of bed early after the surgical procedure, able to care for themselves, and soon ready to go home. This helps the mental outlook and, through it, the physical recovery. The fibrin strands reinforce the platelet plug to form a resilient hemostatic plug capable of withstanding arterial pressure when the constricted vessel relaxes. Massive thrombosis within the vessels would occur once coagulation was initiated, if it continued. However, fibrin is digested during the process. The products of this digestion, and antithrombins normally present in blood, act as anticoagulants. The coagulation mechanism rapidly and efficiently inhibits excessive blood loss so that excessive coagulation does not occur (Fig. 29-2).
Wound healing and hemostasis
Mechanism of wound healing
First intention/primary union
Second intention
Third intention/delayed primary closure
Types of wounds
Factors influencing wound healing
Surgical wound classification
Generalized health condition of the patient
Circulatory status
Smoking.
Surgical technique
Method of hemostasis
Tissue approximation
Physical activity
Hemostasis
Hemostatic process
Wound healing and hemostasis

 Website
Website