 Vertebral Arteries
Vertebral ArteriesSurgical Anatomy of the Vertebral Arteries
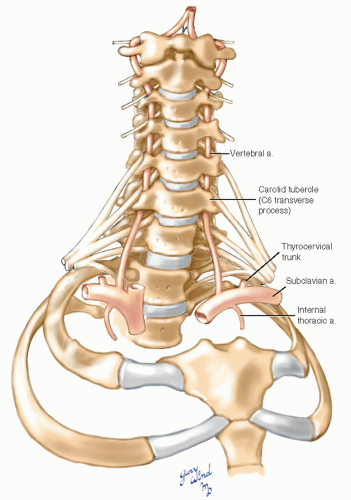
Deep in the root of the neck, the vertebral arteries run the first third of their course from the proximal subclavian arteries to the transverse processes of the sixth cervical vertebrae (Fig. 2-1). For the remaining two-thirds of their course to the foramen magnum, the arteries are encased in a ladder-like bony lattice made up of the fenestrated transverse processes of the upper cervical vertebrae. The foramina for the artery occupy the anterior portion of the trough-like transverse processes, while the roots of the cervical nerves occupy the posterior position.
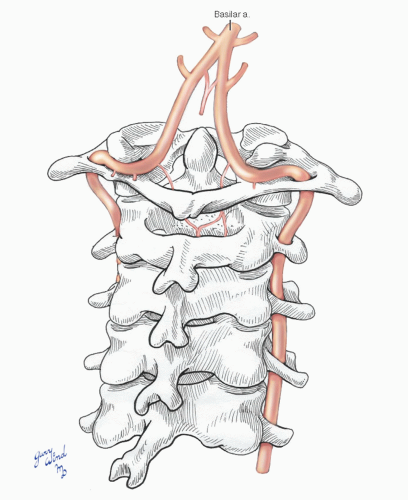
After passing through the transverse processes of the atlas, the arteries loop behind the articular processes and follow an anterior converging course upward through the foramen magnum. Within the cranium, the vertebral arteries unite at the lower border of the pons to form the basilar artery.
The deep central location of the vertebral arteries affords protection but makes surgical access more difficult than access to the companion carotid system. The following discussion focuses on the details of important relationships at different levels of the arteries.
Anterior Paravertebral Musculature
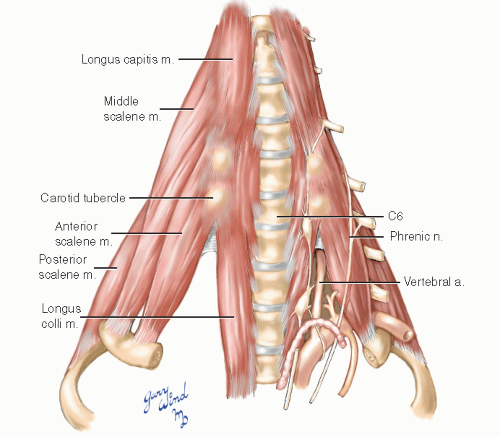
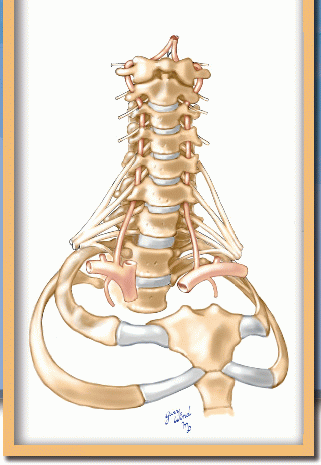
The vertebral arteries lie within a plane defined by a delta-shaped array of muscles attaching to the vertebral bodies and transverse processes (Fig. 2-2). The longus colli and longus capitis muscles provide anterior support to the cervical vertebrae and bracket the anterior longitudinal ligament of the spine between them. Laterally, the scalene muscles fan out from the cervical transverse processes and insert on the first and second ribs. The lower cervical nerve roots emerge between anterior and middle scalene muscles, while the upper roots appear between the longus capitis and levator scapulae muscles. This muscular delta is covered by prevertebral fascia. The anterior scalene and longus colli muscles converge at the prominent anterior tubercle of the transverse process of C6, sometimes called the carotid tubercle (of Chassaignac). In the inverted “V” formed by the muscles below this landmark, the first portion of the vertebral artery penetrates the prevertebral fascia to ascend through the C6 transverse foramen.
The Root of the Neck
The vertebral arteries originate from the first part of the subclavian arteries close to the origins of the internal thoracic (formerly internal mammary), thyrocervical, and costocervical vessels (Fig. 2-3). These origins are arrayed radially around the subclavian with the vertebral arising superiorly and posteriorly. The first portion of the vertebral arteries passes over the cupola of the lung to reach the scalenovertebral angle.
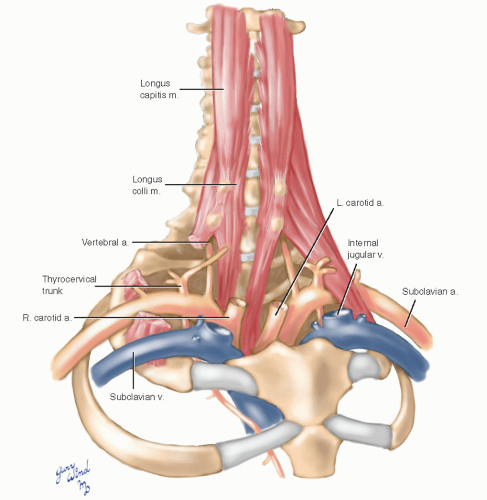 Fig. 2-3 The great vessels at the root of the neck overlie the vertebral arteries and must be mobilized during surgical approaches to the vertebral arteries. |
The venous tributaries that accompany the distal vertebral artery converge to form a single vertebral vein on emerging from the sixth transverse process (Fig. 2-4). The vein enters the proximal subclavian vein just distal to the internal jugular vein. On the left side, the thoracic duct emerges from the posterior thorax, arches over the subclavian artery, and enters the subclavian vein between the internal jugular and vertebral veins.
The cervical sympathetic chain lies on the prevertebral fascia anterior to the longus colli and capitis muscles, which in turn lie anterior to the transverse processes housing the vertebral arteries. The middle cervical sympathetic ganglion lies at about the level of the carotid tubercle, and the inferior ganglion lies posteromedial to the origin of the vertebral artery. The inferior ganglion gives off fibers that wrap around and ascend with the vertebral artery.
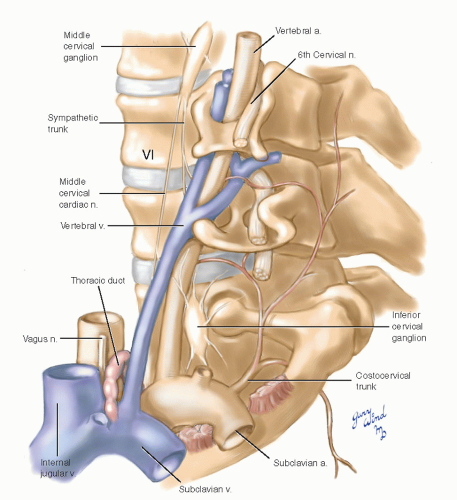 Fig. 2-4 In this lateral view of the proximal left vertebral artery, the scalene fat pad has been removed to show relationships to the thoracic duct, venous, and neural structures. |
The costocervical trunk arises posteriorly from the subclavian. Its cervical division ascends in the deep posterior cervical muscles and communicates with the vertebral along its course and with descending branches of the occipital artery.
Anterior Relations of the Proximal and Midvertebral Artery
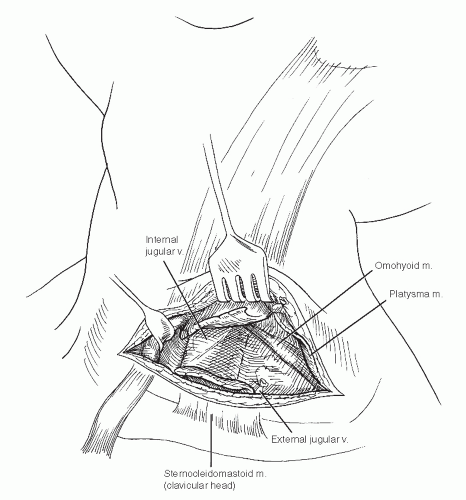
Beneath skin and platysma, the sternocleidomastoid muscle and investing fascia constitute the first layer to unroof on the way to the vertebral arteries (Fig. 2-5). The omohyoid muscle runs diagonally between the sternocleidomastoid and the underlying carotid sheath. The carotid sheath lies between the sternocleidomastoid muscle and prevertebral fascia medially, and lateral to the sheath, the scalene fat pad directly overlies the first portion of the vertebral artery.
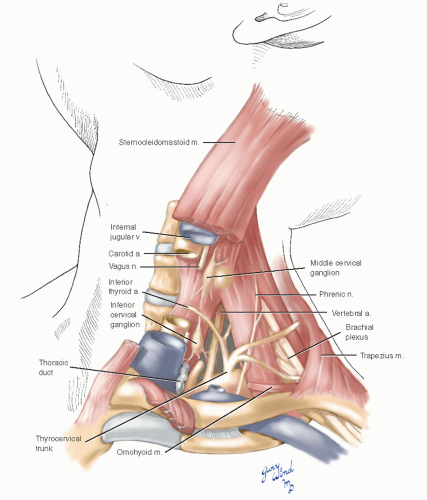 Fig. 2-5 This cut-away view shows the major anatomic landmarks that must be negotiated to reach the vertebral artery. |
In and around the fat pad are critical structures that must be respected when approaching the vertebral artery. Medially on the left side is the previously described thoracic duct. Deep to the fat pad laterally, the phrenic nerves descend diagonally across the anterior scalene muscles, pass lateral to the thyrocervical trunks, and dip between subclavian artery and vein to enter the chest. The inferior thyroid artery crosses anterior to the proximal vertebral artery.
The Distal Vertebral Artery
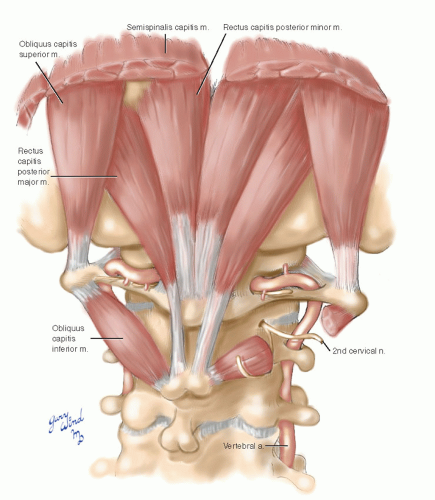
Between the transverse processes of the atlas and axis vertebrae, there is more space for access to the vertebral arteries than in other interspaces due to the decreased bulk of the bony arches posteriorly (Fig. 2-6). After emerging through the foramina of the atlas, the arteries take a sharp bend backward and lie in grooves encircling the posterior rims of the bony articular plateaus. They then course anteriorly, medial to the atlantooccipital articulation, and pass through the foramen magnum.
At the level of the posterior groove, the arteries give off branches to the deep muscles of the neck that anastomose with ascending cervical, occipital, and deep cervical arteries. Medial to the articular facets, the arteries give off branches that descend within the vertebral canal, supplying vertebral bodies and meninges. Prior to converging at the level of the pons, small descending branches fuse to form a midline vessel along the ventral surface of the medulla.
The tortuous terminal extracranial vertebral arteries lie deep within the suboccipital muscular triangles and are difficult to expose (Fig. 2-7).
An anterolateral approach to the C1 to C2 segment is possible by detaching the levator scapulae origins from the tips of the transverse processes (Fig. 2-8).
An anterolateral approach to the C1 to C2 segment is possible by detaching the levator scapulae origins from the tips of the transverse processes (Fig. 2-8).
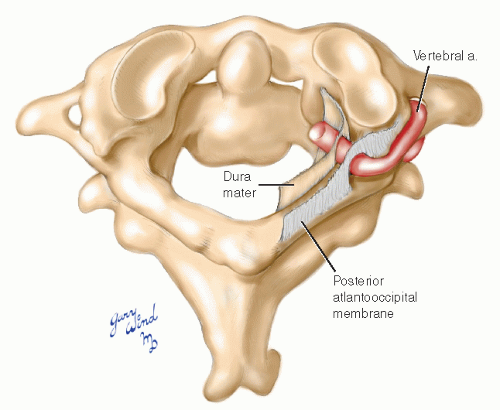
After passing around the posterior part of the articular process, the vertebral artery penetrates first the atlantooccipital ligament and then the dura on its way to the foramen magnum (Fig. 2-9).
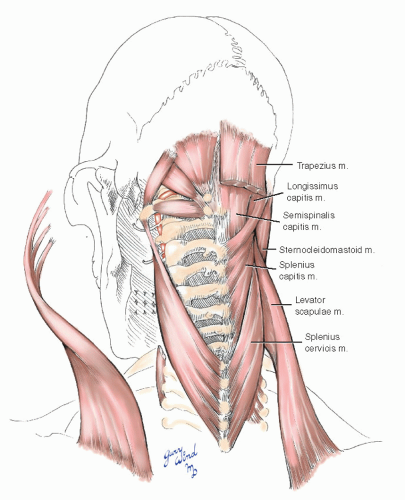 Fig. 2-8 The insertions of muscle slips from the levator scapulae and splenius cervicis onto the first transverse process must be divided to gain access to the C1/C2 segment of the vertebral artery. |
Exposure of the Vertebral Artery in the Neck
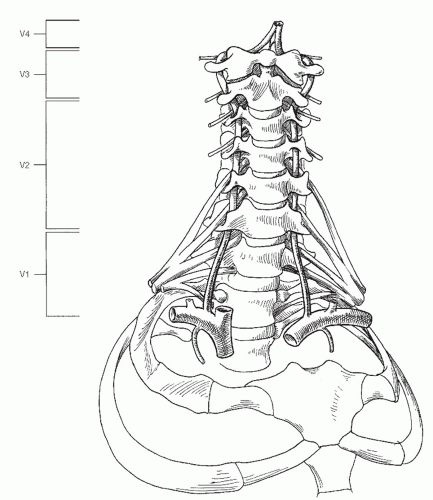
A number of approaches are available to expose the extracranial vertebral artery, depending on the segment. A useful classification for describing the regional anatomy of the vertebral artery has been highlighted by Morasch1 (Fig. 2-10). The most proximal segment (V1) extends from the subclavian origin of the vertebral artery to the level at which the artery enters the transverse process of C6. The interosseous segment (V2) courses within the transverse processes of the cervical vertebrae from C6 to C2. The third segment (V3) begins at the top of the C2 transverse process and terminates at the base of the skull. The intracranial portion (V4) begins at the atlantooccipital membrane and terminates at the basilar artery.
Exposure of the Extraosseous Vertebral Artery (V1 Segment)
There are two main options for exposure of the most proximal portion of the vertebral artery: the transverse supraclavicular approach and the vertical anterior cervical approach. Although the supraclavicular approach affords excellent exposure of the vertebral artery at its origin, the exposure is relatively limited and requires transection of the sternocleidomastoid muscle. The anterior cervical approach does not require muscular transection, and it permits rapid extension of the incision for vascular control of more distal vertebral artery segments. However, exposure of the vertebral artery is more difficult through a cervical incision. In general, the supraclavicular approach is employed for elective operations involving vertebral artery reimplantation into the adjacent common carotid artery, and the anterior cervical approach is favored during emergency explorations for suspected vertebral artery injury.1,2,3,4
Supraclavicular Approach
The patient is supine, and the head is turned away from the side of surgery. The incision is made approximately 1 cm above the clavicle, beginning at the clavicular head and extending laterally for a distance of 7 or 8 cm (Fig. 2-11). The incision is
deepened through the platysma muscle and superficial fascia. The external jugular vein is divided at the lateral border of the sternocleidomastoid muscle.
deepened through the platysma muscle and superficial fascia. The external jugular vein is divided at the lateral border of the sternocleidomastoid muscle.
Division of the clavicular head of the sternocleidomastoid muscle and retraction of the sternal head exposes the underlying carotid sheath. The sheath is mobilized by vertical dissection along the lateral border of the internal jugular vein, and the omohyoid muscle is divided (Fig. 2-12




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree