Urothelial Carcinoma of Prostate
Gladell P. Paner, MD
Mahul B. Amin, MD
Key Facts
Terminology
UroCa involving prostate arising from prostatic urethra, periurethral glands, and proximal prostatic ducts
Clinicopathologically distinct from bladder UroCa transmurally invading through bladder wall and extending into prostate (pT4 bladder cancer)
Clinical Issues
Primary prostate UroCa is uncommon, comprising 1-4% of prostate cancers in adults
Prostate involvement in cystoprostatectomy for invasive bladder UroCa is relatively more common, ranging from 12-58%
Similar in age distribution to bladder UroCa
Most primary prostatic UroCa presents with obstructive urinary symptoms
Disease specific survival higher in CIS of prostatic urethral glands, ducts, and acini vs. urethral submucosal and prostatic stromal invasion
Prostatic stromal invasion associated with higher incidence of nodal metastasis
Survival rate poorer for bladder UroCa transmurally invading through bladder wall and extending into prostate (pT4 bladder cancer) vs. with prostatic stromal invasion arising intraurethrally
Microscopic Pathology
Diagnostic criteria identical to those of bladder UroCa
CIS can spread from prostatic urethra, involves ducts and acini, or grows along ejaculatory duct to seminal vesicle
Stromal invasion may arise anywhere along this spread
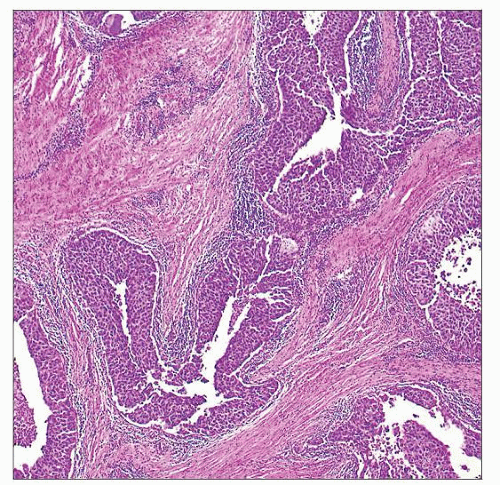
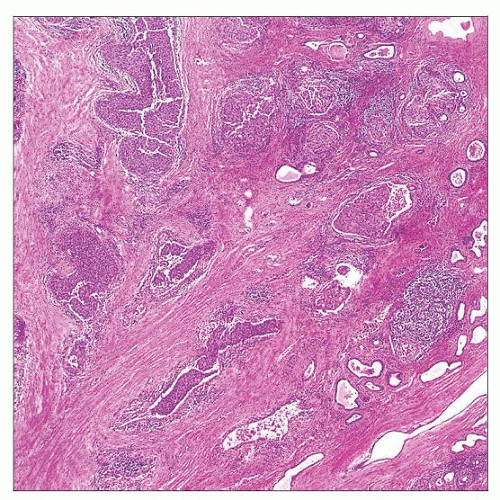 UroCa is shown involving prostatic ducts and acini. Preexisting acini are expanded and completely filled by UroCa. Stromal invasion may arise anywhere along prostatic urethra to the acini. |
TERMINOLOGY
Abbreviations
Urothelial carcinoma (UroCa)
Carcinoma in situ (CIS)
Synonyms
Intraepithelial carcinoma of periurethral glands and prostatic ducts
Periurethral prostatic duct carcinoma
Definitions
UroCa involving prostate arising from prostatic urethra, periurethral glands, and proximal prostatic ducts
Clinicopathologically distinct from bladder UroCa transmurally invading through bladder wall and extending into prostate (pT4 bladder UroCa)
ETIOLOGY/PATHOGENESIS
Origin
Urothelium in periurethral mucosal and submucosal glands &/or junction with prostatic ducts
In strict terms, UroCa arising from these sites is true primary prostatic UroCa
Prostatic urethral urothelium
Frequently coexists with primary prostatic UroCa
CLINICAL ISSUES
Epidemiology
Incidence
Primary prostate UroCa is uncommon, comprising 1-4% of prostate cancers in adults
64% have concomitant bladder urothelial CIS
24% have no prior or concurrent invasive or in situ bladder UroCa
Prostatic involvement in cystoprostatectomy for bladder UroCa is relatively more common, ranging from 12-58%
UroCa extending from prostatic urethra and ducts comprises 76-87%
UroCa transmurally invading bladder wall into prostate (pT4 bladder UroCa) comprises 13-24%
Age
Similar in age distribution to bladder UroCa
Mean: 66 years, range: 52-87 years
Presentation
More commonly detected in cystoprostatectomies for UroCa of bladder
Most primary prostatic UroCa present with obstructive urinary symptoms, such as hesitancy, slowed stream, frequency, and dysuria
May have rapid progression of obstruction, usually < 6 months
Other symptoms include hematuria, prostatism, weight loss, and rectal pain
Prostate may be large on rectal examination, and may be mistaken clinically as benign prostatic hyperplasia, prostatitis, or prostate cancer
Symptomatic cases more often encountered in transurethral resection of prostate (TURP) specimens performed for obstructive symptoms
Laboratory Tests
Serum PSA level typically not elevated
However, 1 study showed 78% of prostate UroCa detected by needle biopsy had elevated serum PSA levels
Although this high percentage is perhaps reflective of specimen type performed for elevated PSA, which may or may not be due to UroCa
May have elevated serum alkaline phosphatase level, due to bone metastasis
Treatment
Depends on extent, location, and stage of disease
In patients presenting with limited disease in TUR specimens
Prostatic urethral UroCa with minimal or superficial prostatic acinar involvement without stromal involvement may be treated with bacillus Calmette-Guérin (BCG)
Cystoscopy should be performed to determine presence of bladder neoplasia
1 study reported 87% complete response rate for BCG, but only 17% of these had prostatic acinar involvement and none had stromal invasion
For cases involving prostatic stroma and peripheral zone
Radical cystoprostatectomy is treatment of choice
Chemotherapy and radiotherapy may have role
Prognosis
Depends on extent, location, and stage of disease
Primary prostatic UroCa with no invasive bladder UroCa
Disease-specific survival higher in CIS of prostatic urethra and involvement of prostatic ducts and acini vs. UroCa involving suburethral glands or prostatic stroma
5-year disease-specific survival
Prostatic urethral CIS and CIS involving prostatic ducts and acini without stromal invasion (100%)
Prostatic stromal invasion (45%)
Extraprostatic extension (0%)
Lymph node extension (30%)
Prostate primary UroCa overall (52%)
Concurrent prostate adenocarcinoma seen in 8%
Subsequent UroCa of upper urinary tract seen in 6%
Metastases most commonly occur in bone, lung, and liver
Prostate UroCa in patients with invasive bladder UroCa
Bladder UroCa with no prostatic involvement vs. with involvement
Bladder UroCa patients without prostatic involvement 5-year survival rate: 64%
Bladder UroCa patients with either prostatic CIS and urethral lamina propria invasion 5-year survival rate: 44%
Bladder UroCa patients with prostatic stromal/periprostatic/seminal vesical invasion 5-year survival rate: 32%
Bladder UroCa patients with prostatic urethral UroCa involving prostatic stroma vs. pT4 bladder UroCa
Prostate involvement by UroCa from urethra 5- year overall survival: 43-64%
pT4 bladder UroCa 5-year overall survival: 22-25%
Bladder UroCa patients with prostatic urethral UroCa, noninvasive (involving ducts and acini only) vs. invasive (involving prostatic stroma)
Survival rates similar for prostatic urethral and noninvasive prostatic urethral UroCa
Prostatic stromal invasion associated with higher incidence of nodal metastasis and worse survival
Noninvasive UroCa 5-year overall survival rate: 49%
Stromal invasive UroCa 5-year overall survival rate: 25%
Prostate involvement decreases survival of bladder cancer, which varies according to primary stage of bladder cancer
Age, degree of prostate invasion, and lymph node involvement are independent prognostic variables
Locoregional Involvement in Reported Series
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree