Chapter 15 Intranasal steroids and cromolyn are generally considered second-line treatment for upper respiratory conditions. Oral formulations of these drugs are used for lower respiratory conditions. These drugs are discussed in detail in Chapter 14; only their intranasal use in upper respiratory conditions is discussed here. Antitussives and expectorants are used as adjunct therapy in upper respiratory and lower respiratory conditions. Combination drugs that contain these different categories of medications are available both OTC and by prescription. These combination product ingredients change rapidly, and this may be very confusing to the consumer. Often, OTC combinations purchased by patients contain medications that are not indicated for the condition for which the combination is labeled, and use can be counterproductive to clearing up symptoms. Many nighttime formulations contain alcohol and acetaminophen, which should not be consumed together. Some consumers use products incorrectly, taking an antihistamine for congestion when actually a decongestant is needed. Products with analgesics are often used by patients even in the absence of pain or fever. Many consumers, particularly the elderly, use these products without considering the ingredients and possible drug interactions with medications they are already taking, or preexisting medical conditions that may be adversely affected by certain medications. An example would be patients with hypertension, glaucoma, or urinary retention who take pseudoephedrine for congestion. Many patients self-prescribe OTCs for respiratory problems, so query patients specifically about use of OTC products. (See Chapter 7 for information on OTC use.) The steroids used in intranasal products have potent glucocorticoid and weak mineralocorticoid activity. Glucocorticoids inhibit cells, including mast cells, eosinophils, neutrophils, macrophages, lymphocytes, and mediators such as histamine, leukotrienes, and cytokines. They exert direct local antiinflammatory effects with minimal systemic effects. Intranasal corticosteroids effectively control the four major symptoms of allergic rhinitis: rhinorrhea, congestion, sneezing, and nasal itch. They are helpful in managing moderate to severe disease and are used in treating both seasonal and perennial allergic rhinitis. These medications must be used consistently on a daily basis for effectiveness, and maximum effects may not be noted for several days to weeks. For details on the immune system, see Chapter 68. Cromolyn sodium is an OTC intranasal mast cell stabilizer that is used as a preventative agent that is taken in advance of allergen exposure. It is an antiinflammatory agent that has no intrinsic bronchodilator, antihistaminic, vasoconstrictor, or glucocorticoid activity. Cromolyn inhibits sensitized and mast cell degranulation that occurs after exposure to specific antigens. The drug inhibits the release of mediators, histamine, and slow-reacting substance of anaphylaxis (SRS-A) from the mast cell. It inhibits calcium from entering the mast cell, resulting in the prevention of mediator release. It is effective in reducing rhinorrhea, sneezing, and nasal itch, but it has minimal effect on nasal congestion. Cromolyn acts locally on tissue, inhibiting the release of chemical mediators by preventing mast cell degranulation. It has an excellent safety profile and minimal adverse effects consisting of nasal irritation, stinging, and sneezing. Cromolyn must be taken properly as a nebulized aerosol, inhaled through the mouth, or swallowed orally four to six times a day, and its effect may not be seen for 4 to 6 weeks to months. For details, see Chapter 14. • A comprehensive algorithm of Treatment Guidelines for Upper Respiratory Illness in Children and Adults from the Institute for Clinical Systems Improvement (ICSI) can be found at http://www.guideline.gov/algorithm/5564/NGC-5564_1.html. Algorithms from previous guidelines for viral upper respiratory infection (VURI), pharyngitis, rhinitis, and sinusitis were incorporated into this algorithm. • American College of Chest Physicians (ACCP) evidence-based clinical practice guidelines for cough and the common cold provide recommendations and algorithms for care of acute cough due to viral infection (http://www.guideline.gov/summary/summary.aspx?doc_id=8654&nbr=004819). • Infectious Disease Society New Guidelines for management of rhinosinusitis. http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/IDSA%20Clinical%20Practice%20Guideline%20for%20Acute%20Bacterial%20Rhinosinusitis%20in%20Children%20and%20Adults.pdf • The VURI in adults and children in the above-mentioned guideline contains an annotated bibliography and discussion of the evidence that supports the recommendations. • According to randomized controlled trials (RCTs) in allergic rhinitis, oral antihistamines were used first in rhinitis and were found to help control itching, sneezing, rhinorrhea, and stuffiness in most patients; however, they do not alleviate ocular symptoms. Nasal corticosteroids are indicated for patients who do not respond to antihistamines and are considered the most potent medication for the treatment of rhinitis. Nasal cromolyn is less effective than nasal corticosteroids. Intranasal antihistamines are effective in treating nasal symptoms of seasonal, perennial, and vasomotor rhinitis but offer no benefit over conventional treatment. Oral decongestants decrease nasal mucosa swelling, and this reduces nasal congestion. • Hand washing is the most effective way to prevent the spread of VURI. Because this is viewed as mundane and common knowledge, many clinicians fail to reinforce this message and further fail to act as role models by washing their own hands at the beginning of each patient encounter. • It is important to recognize the signs and symptoms of serious illness in VURI and allergic rhinitis. Symptoms such as upper and lower airway obstruction and severe headache require prompt evaluation and care. • Do not treat cold symptoms with aspirin-containing products for anyone younger than age 21. • Avoid acetaminophen in patients with liver dysfunction. • In adults, evidence suggests that zinc gluconate may decrease the duration of a cold if started within 24 hours of onset; however, studies are conflicting. Adverse reactions such as nausea and bad taste may limit its usefulness. Loss of smell has occurred. No current studies indicate that zinc has effectiveness in treating cold symptoms in children. • Findings in the medical literature do not support the use of echinacea in preventing VURI • Allergy testing is rarely helpful in diagnosing allergic rhinitis but may be useful in patients with multiple allergen sensitivities. The goal of therapy is to relieve symptoms, and avoidance of allergens is the first step in this process. • Controversy is ongoing regarding the use of medication vs. immunotherapy. Risk–cost analyses have not been performed; however, patients with moderate to severe perennial allergies may benefit most from immunotherapy. • Patients with cough associated with viral respiratory infection can be treated with a first-generation antihistamine/decongestant combination preparation. Naproxen can also be used to help to decrease cough. Newer-generation, nonsedating antihistamines are ineffective in reducing cough and should not be used. • Current recommendations have been revised to narrow recommended inhaled anticholinergic agents to a single drug, ipratropium bromide, for cough due to URI or bronchitis. The current guideline supports the use of codeine only in chronic bronchitis and not in cough due to URI. Peripheral and central cough suppressants have limited efficacy in cough due to URI. OTC combination cold medications, other than antihistamine/decongestant combinations, and preparations that contain zinc are not recommended for acute cough due to the common cold. • Nonpharmacologic treatment for URI consists of rest as needed and increased fluids, especially water. Adequate hydration (called bronchial toilet) may be more helpful in symptom relief than medication because it helps to decrease cough, thin secretions, and hydrate tissues. • Use of a teaspoon of honey has been shown to be effective in reducing cough in small children. • For nonpharmacologic treatment of allergic rhinitis, identify environmental precipitants, which may include time of year, work and home environment, and pets. Implement strategies designed to reduce these factors. Avoid outdoor allergens, use air conditioning in home and car, exercise outdoors in the afternoon when pollen counts are typically low, use high-efficiency particulate air (HEPA) filters in the home, and use a dryer rather than a clothesline, where clothes can collect airborne pollen. • For indoor allergens, use strategies for dust, pet, mold, and cockroach avoidance. • Normal saline nasal sprays or nasal irrigation, twice daily, may help reduce postnasal drip, sneezing, and congestion. • Ask patients if they are using complimentary or alternative medicines, many of which may interact with drugs given for upper respiratory problems. TABLE 15-1 • Patient history reveals which symptoms are most troublesome and can be targeted. Decongestants, antihistamines, or a combination thereof are proven effective. Antitussives or expectorants may be helpful. Because URIs are viral in origin, antibiotics are not indicated. Many patients must have this important fact explained to them. • Pharmacologic treatment of allergic rhinitis involves identifying and targeting symptoms that are most problematic to the patient; these may include sneezing, runny nose, itching, and nasal congestion. • Treat mild, intermittent symptoms with an antihistamine, preferably nonsedating, or a decongestant. If the patient is unable to take an oral antihistamine, consider the use of a nasal antihistamine, intranasal cromolyn, or leukotriene receptor antagonist. • Treat moderate, frequent symptoms with a regular- to high-dose intranasal corticosteroid. Add an oral or a nasal antihistamine and decongestant, if necessary. • Treat moderate, persistent symptoms with a combination regimen, consisting of intranasal corticosteroids plus a nonsedating or intranasal antihistamine and decongestant, if necessary. • Treat severe symptoms with a combination regimen consisting of a nonsedating antihistamine with or without a decongestant and intranasal corticosteroid. Consider the use of an oral steroid for 5 days, as well as the use of oxymetazoline as needed for no longer than 3 days. • These common drugs, which are widely available without prescription, are very effective in treating nasal congestion. Decongestants are sympathomimetic amines used to relieve nasal congestion caused by colds, allergies, and URIs; they also promote sinus drainage and relieve eustachian tube congestion. Oral forms are often used in combination with antihistamines and expectorants in both OTC and prescription doses (see Table 15-2). Topical nasal decongestants provide direct relief to swollen nasal membranes and sometimes are used to decrease congestion of the eustachian tube in middle ear infection and to relieve pressure and blockage of the ear during air travel. Decongestants should be used with caution in patients with hypertension, cardiovascular and peripheral vascular disease, hyperthyroidism, diabetes mellitus, prostatic hypertrophy, urinary retention, and increased intraocular pressure because of their sympathomimetic effects. They are contraindicated in patients with mitral valve prolapse and cardiac palpitations. They also have many side effects that can limit their use, particularly in the elderly. • Oral decongestants generally do not cause sedation but may cause systemic effects, including nervousness, dizziness, and difficulty sleeping, particularly in infants and the elderly. The clinical problems most often seen with oral decongestants include tachycardia, nervousness, insomnia, palpitations, headache, and irritability, which may be poorly tolerated in the frail elderly; patients with poorly controlled hypertension may experience an increase in blood pressure. The provider should question the patient thoroughly about his history of decongestant use. Patients may voice complaints of their “heart racing,” or that the drug keeps them awake. Data suggest that oral decongestants may be used cautiously in patients with controlled hypertension. Sustained-release formulations may have less effect on the cardiovascular system. However, because they may antagonize the effects of antihypertensive medications, alternative agents such as topical decongestants should be used for these patients. The FDA has determined that the combination of pseudoephedrine and caffeine is not recognized as safe and effective for OTC use. Cough and cold formulations for children under the age of 6 are not recommended, and most manufacturers have removed these products from the market because of so many cases of accidental overdosing. • Topical decongestants have little systemic effect, but because of rebound congestion (rhinitis medicamentosa), they should be used only in acute conditions for no longer than 3 consecutive days. Rebound congestion is treated by gradual withdrawal, one nare at a time. Saline nasal spray is often helpful. Overall, topical decongestants are more effective than oral ones, but oral decongestants have longer durations of action and are less irritating. • Antihistamines are H1-receptor antagonists that are often used alone or in combination with decongestants and expectorants to relieve symptoms associated with perennial and seasonal allergies with associated rhinitis, vasomotor rhinitis, allergic conjunctivitis, and cold symptoms such as sneezing and runny nose. They also are used to relieve allergic and nonallergic pruritic symptoms, to alleviate mild urticaria and angioedema, for prophylaxis against allergic reactions to blood or plasma products, and as adjunctive therapy in anaphylactic reactions Certain antihistamines also have antiemetic effects and are useful for nausea, vomiting, vertigo, and motion sickness. • Many OTC cold remedies contain antihistamines; however, their use in the treatment of cold symptoms is controversial. Antihistamines are best used to treat allergic symptoms such as rhinorrhea; watery, itchy eyes; postnasal drainage; and sneezing. Decongestants are preferred for treatment of cold symptoms, such as nasal congestion caused by swollen nasal membranes. • In general, antihistamines are not recommended to treat lower respiratory tract symptoms, including asthma, because some of their anticholinergic effects may cause thickening of respiratory secretions and may impair expectoration. Several evidence-based reports, however, indicate that antihistamines can be safely used in asthmatic patients with severe perennial allergies without exacerbating the asthma. • Two generations of antihistamines are available. First-generation agents are usually available OTC and often are used before a health care provider is consulted. Most cause sedation and have sometimes been included in sleep aids. However, they remain highly effective in symptomatic treatment, and some products have been released (by prescription only) that provide new delivery systems that decrease drowsiness. • Second-generation antihistamines are favored by clinicians for their efficacy/safety ratio and rapid onset of relief from sneezing, pruritus, and watery rhinorrhea. Most of these are now available OTC. All antihistamines are not very effective against nasal congestion and may even compound or contribute to its development. Local antihistamine nasal sprays and various ocular antihistamines are also effective in less than 30 minutes. • OTC antihistamines that generally cause sedation may interfere with the patient’s activities and contribute to poor adherence. Therefore, an antihistamine and a decongestant often are combined to counteract the side effects of each drug while providing dual treatment. Sedating antihistamines are sometimes preferred if symptoms prevent patients from sleeping. Sedating antihistamines are also used in combination with analgesics as a pain reliever and sleep aid. Prescribed antihistamines are less likely to cause sedation and are generally well tolerated. If a particular antihistamine has lost effectiveness or causes untoward side effects, another antihistamine should be selected from a different class. If the patient requires two antihistamines for severe symptoms, drugs from two different classes should be selected. • Cetirizine was recently put on the FDA drug watch list because of the incidence of oculogyric crisis. • Intranasal corticosteroids are the most effective agents for the management of allergic rhinitis because of their direct reduction of nasal inflammation and their ability to reduce nasal hyperreactivity. All agents are safe and effective and will improve the patient’s quality of life if the patient uses them on a daily basis. Many patients do not like the odor or taste associated with specific agents, and one or two different medications may have to be tried before the most tolerable agent can be found for an individual. It is essential for the health care provider to help the patient understand the important role of these agents and to demonstrate how they should be administered correctly. • Intranasal corticosteroids should be used for at least 1 month before it is decided whether they are effective. Patients should be warned that improvement usually does not begin until 1 to 2 weeks after therapy is started. Intranasal corticosteroids can be used with asthmatic patients and with those who have comorbid nasal polyposis. Intranasal steroids may help to shrink nasal polyps. • Exceeding the recommended dose may result in systemic effects, including suppression of hypothalamic-pituitary-adrenal (HPA) axis function. Systemic effects are possible with inhaled steroids and are less likely with intranasal corticosteroids when used at conventional recommended doses. • It should be noted that in some cases, oral corticosteroids may be required for a short time. These powerful drugs reduce nasal inflammation and hyperreactivity but have potentially serious side effects when used over a long period. A short course of tapered corticosteroids is advisable only for moderate to severe exacerbations of allergic rhinitis.
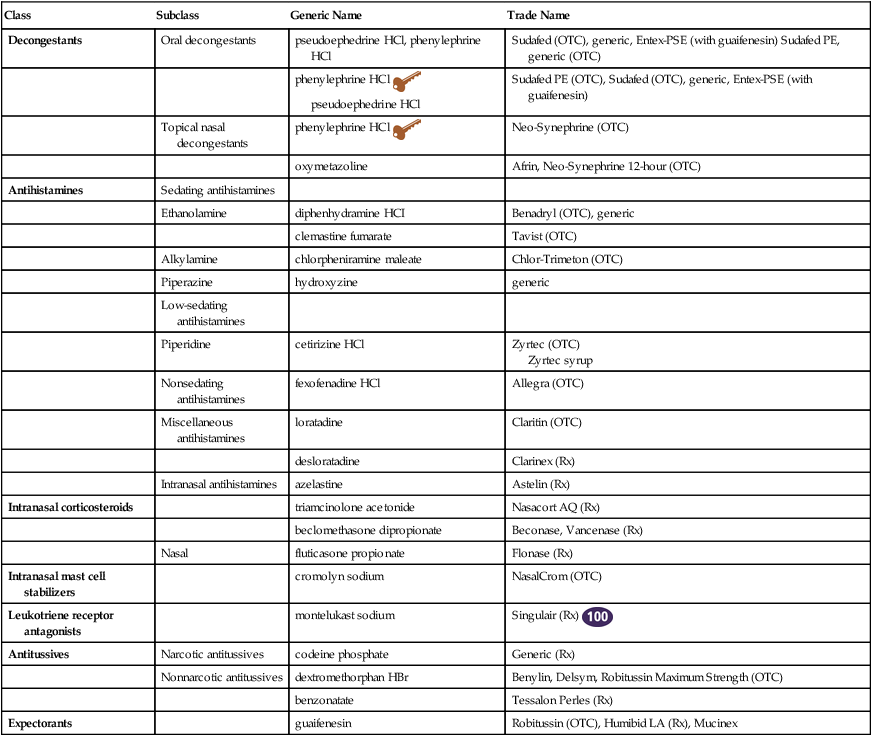
Upper Respiratory Agents
Class
Subclass
Generic Name
Trade Name
Decongestants
Oral decongestants
pseudoephedrine HCl, phenylephrine HCl
Sudafed (OTC), generic, Entex-PSE (with guaifenesin) Sudafed PE, generic (OTC)
phenylephrine HCl ![]() pseudoephedrine HCl
pseudoephedrine HCl
Sudafed PE (OTC), Sudafed (OTC), generic, Entex-PSE (with guaifenesin)
Topical nasal decongestants
phenylephrine HCl ![]()
Neo-Synephrine (OTC)
oxymetazoline
Afrin, Neo-Synephrine 12-hour (OTC)
Antihistamines
Sedating antihistamines
Ethanolamine
diphenhydramine HCI
Benadryl (OTC), generic
clemastine fumarate
Tavist (OTC)
Alkylamine
chlorpheniramine maleate
Chlor-Trimeton (OTC)
Piperazine
hydroxyzine
generic
Low-sedating antihistamines
Piperidine
cetirizine HCl
Zyrtec (OTC)
Zyrtec syrup
Nonsedating antihistamines
fexofenadine HCl
Allegra (OTC)
Miscellaneous antihistamines
loratadine
Claritin (OTC)
desloratadine
Clarinex (Rx)
Intranasal antihistamines
azelastine
Astelin (Rx)
Intranasal corticosteroids
triamcinolone acetonide
Nasacort AQ (Rx)
beclomethasone dipropionate
Beconase, Vancenase (Rx)
Nasal
fluticasone propionate
Flonase (Rx)
Intranasal mast cell stabilizers
cromolyn sodium
NasalCrom (OTC)
Leukotriene receptor antagonists
montelukast sodium
Singulair (Rx) ![]()
Antitussives
Narcotic antitussives
codeine phosphate
Generic (Rx)
Nonnarcotic antitussives
dextromethorphan HBr
Benylin, Delsym, Robitussin Maximum Strength (OTC)
benzonatate
Tessalon Perles (Rx)
Expectorants
guaifenesin
Robitussin (OTC), Humibid LA (Rx), Mucinex
Mechanism of Action
Decongestants
Intranasal Corticosteroids
Intranasal Mast Cell Stabilizers
Treatment Principles
Standardized Guidelines
Evidence-Based Recommendations
Cardinal Points of Treatment
Upper Respiratory Illness
Allergic Rhinitis
Cough
Nonpharmacologic Treatment
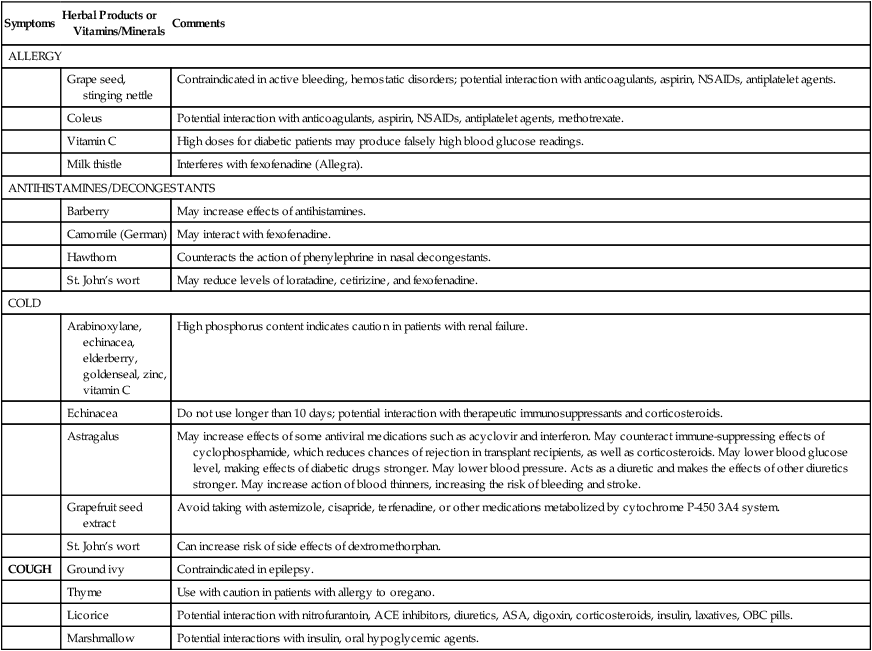
![]() See Table 15-1 for a list of potential herbal-drug interactions.
See Table 15-1 for a list of potential herbal-drug interactions.
Symptoms
Herbal Products or Vitamins/Minerals
Comments
ALLERGY
Grape seed, stinging nettle
Contraindicated in active bleeding, hemostatic disorders; potential interaction with anticoagulants, aspirin, NSAIDs, antiplatelet agents.
Coleus
Potential interaction with anticoagulants, aspirin, NSAIDs, antiplatelet agents, methotrexate.
Vitamin C
High doses for diabetic patients may produce falsely high blood glucose readings.
Milk thistle
Interferes with fexofenadine (Allegra).
ANTIHISTAMINES/DECONGESTANTS
Barberry
May increase effects of antihistamines.
Camomile (German)
May interact with fexofenadine.
Hawthorn
Counteracts the action of phenylephrine in nasal decongestants.
St. John’s wort
May reduce levels of loratadine, cetirizine, and fexofenadine.
COLD
Arabinoxylane, echinacea, elderberry, goldenseal, zinc, vitamin C
High phosphorus content indicates caution in patients with renal failure.
Echinacea
Do not use longer than 10 days; potential interaction with therapeutic immunosuppressants and corticosteroids.
Astragalus
May increase effects of some antiviral medications such as acyclovir and interferon. May counteract immune-suppressing effects of cyclophosphamide, which reduces chances of rejection in transplant recipients, as well as corticosteroids. May lower blood glucose level, making effects of diabetic drugs stronger. May lower blood pressure. Acts as a diuretic and makes the effects of other diuretics stronger. May increase action of blood thinners, increasing the risk of bleeding and stroke.
Grapefruit seed extract
Avoid taking with astemizole, cisapride, terfenadine, or other medications metabolized by cytochrome P-450 3A4 system.
St. John’s wort
Can increase risk of side effects of dextromethorphan.
COUGH
Ground ivy
Contraindicated in epilepsy.
Thyme
Use with caution in patients with allergy to oregano.
Licorice
Potential interaction with nitrofurantoin, ACE inhibitors, diuretics, ASA, digoxin, corticosteroids, insulin, laxatives, OBC pills.
Marshmallow
Potential interactions with insulin, oral hypoglycemic agents.
Pharmacologic Treatment
Decongestants
Antihistamines
Intranasal Corticosteroids
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Upper Respiratory Agents
Only gold members can continue reading. Log In or Register to continue
