DRUG CLASSES
Acid neutralizers
Acid reducer
• Histamine H2 antagonists
• Proton pump inhibitors
GI stimulants
Antiemetics
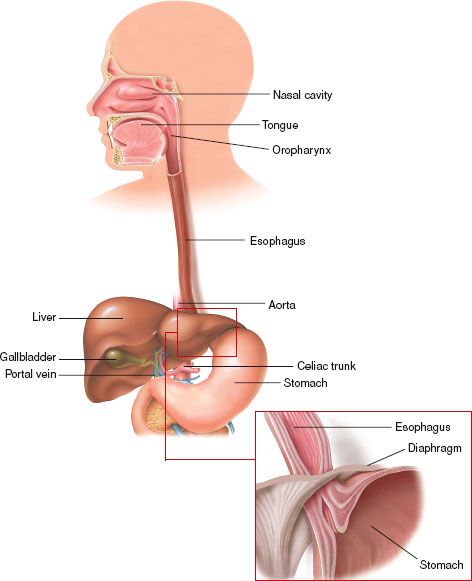
The upper GI system consists of the mouth, esophagus, and stomach (Fig. 40.1). The GI system is essentially a long tube in the body where ingested food and fluids are processed for absorption of nutrients. The mouth is responsible for breaking down food parts and mixing them with saliva to begin the digestion process. The tubular esophagus connects the mouth to the stomach, where food is mixed with acids and enzymes to become a solution for absorption. Some of the cells of the stomach secrete hydrochloric acid (HCl), a substance that aids in the initial digestive process. Problems occur when acids or stomach contents reverse direction and come back up into the esophagus or stomach, which can create tissue damage and ulcers.
PHARMACOLOGY IN PRACTICE

Alfredo Garcia is being seen in the clinic for an upper respiratory infection. During the intake assessment, you find that his blood pressure is high and he complains of “heartburn.” You ask him what helps relieve the heartburn. Mr. Garcia is attempting to use home remedies to decrease acid production in his stomach, and he tells you that he thinks he might have an ulcer, so he has been drinking cream and half-and-half to coat the ulcer. At one time, antiulcer diets included the use of dairy products with the intent of coating the mucosal lining of the stomach, protecting it from acid secretion. While reading this chapter, you will learn about the current method to treat peptic ulcers in the stomach.
Figure 40.1 The upper GI system with esophagogastric junction featured. (Courtesy of the Anatomical Chart Co.)
Drugs are presented in this chapter according to their function, whether they treat gastric acid production or prevent vomiting. Drugs that neutralize HCl and protect the mucosal lining are called antacids. Drugs that reduce the production and release of HCl include histamine type 2 receptor (H2) antagonists, proton pump inhibitors, and miscellaneous acid-reducing agents. The proton pump inhibitors are particularly important in the treatment of Helicobacter pylori infection in patients with active duodenal ulcers. H. pylori are believed to cause a type of chronic gastritis and some peptic and duodenal ulcers as well. GI stimulants facilitate emptying of stomach contents into the small intestine and are used both as ulcer treatments and as antiemetics. Antiemetics are used to treat and prevent nausea and vomiting. Some of the more common drugs are listed in the Summary Drug Table: Upper Gastrointestinal System Drugs.
Actions
Antacids (“against acids”) are drugs that neutralize or reduce the acidity of stomach and duodenal contents by combining with HCl and increasing the pH of the stomach acid. Antacids do not “coat” the stomach lining, although they may increase the sphincter tone of the lower esophagus. Examples of antacids include aluminum (Amphojel), magaldrate (Riopan), and magnesium (Milk of Magnesia).
Uses
Antacids are used in the treatment of hyperacidity caused by the following:
• Heartburn, acid indigestion, or sour stomach
• Gastroesophageal reflux disease (GERD; a reflux or backup of gastric contents into the esophagus)
• Peptic ulcer
Antacids may be used to treat conditions that are not associated with the GI system. For example, aluminum carbonate is a phosphate-binding agent and is used in treating hyperphosphatemia (often associated with chronic renal failure) or as an adjunct to a low-phosphate diet to prevent formation of phosphate-based urinary stones. Calcium may be used in treating calcium deficiency states such as menopausal osteoporosis. Magnesium may be used for treating magnesium deficiencies or magnesium depletion from malnutrition, restricted diet, or alcoholism.
Adverse Reactions
The magnesium- and sodium-containing antacids may have a laxative effect and may produce diarrhea. Aluminum- and calcium-containing products tend to produce constipation. Although the antacids have the potential for serious adverse reactions, they have a wide margin of safety, especially when used as prescribed. Adverse reactions of concern include:
- Aluminum-containing antacids—constipation, intestinal impaction, anorexia, weakness, tremors, and bone pain
- Magnesium-containing antacids—severe diarrhea, dehydration, and hypermagnesemia (nausea, vomiting, hypotension, decreased respirations)
- Calcium-containing antacids—rebound hyperacidity, metabolic alkalosis, hypercalcemia, vomiting, confusion, headache, renal calculi, and neurologic impairment
- Sodium bicarbonate—systemic alkalosis and rebound hyperacidity
Contraindications and Precautions
The antacids are contraindicated in patients with severe abdominal pain of unknown cause and during lactation. Sodium-containing antacids are contraindicated in patients with cardiovascular problems, such as hypertension or heart failure, and those on sodium-restricted diets. Calcium-containing antacids are contraindicated in patients with renal calculi or hypercalcemia.
Aluminum-containing antacids are used cautiously in patients with gastric outlet obstruction or those with upper GI bleeding. Magnesium- and aluminum-containing antacids are used cautiously in patients with decreased kidney function. The calcium-containing antacids are used cautiously in patients with respiratory insufficiency, renal impairment, or cardiac disease. Antacids are classified as pregnancy category C drugs and should be used with caution during pregnancy.
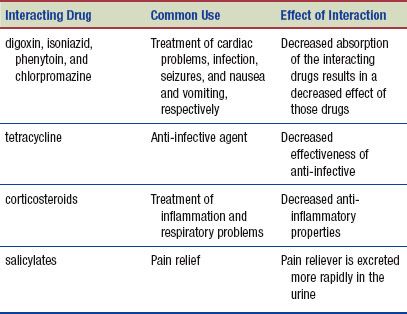
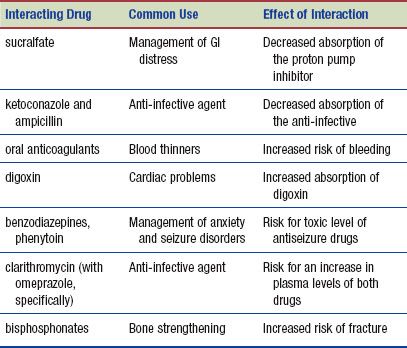
Interactions
The following interactions may occur when an antacid is administered with another agent:
Drugs that reduce the production of HCl include histamine H2 antagonists, proton pump inhibitors, and miscellaneous drugs such as pepsin inhibitors, prostaglandins, and cholinergic blockers.
Histamine H2 Antagonists
Actions
These drugs inhibit the action of histamine at H2 receptor cells of the stomach, which then reduces the secretion of gastric acid. Because cholinergic blocking drugs typically block the action of histamine throughout the entire body, they are used less frequently. Histamine H2 antagonists do not cause the effects of the cholinergic blockers, because they are selective only for the H2 receptors in the stomach and not the general body H2 receptors. When ulcers are present, the decrease in acid allows the ulcerated areas to heal. Examples of histamine H2 antagonists include cimetidine (Tagamet), famotidine (Pepcid), and ranitidine (Zantac).
Uses
These drugs are used prophylactically to treat stress-related ulcers and acute upper GI bleeding in critically ill patients. They are also used for the treatment of the following:
• Heartburn, acid indigestion, and sour stomach (frequently sold as over-the-counter remedies)
• GERD
• Gastric or duodenal ulcer
• Gastric hypersecretory conditions (excessive gastric secretion of HCl)
Adverse Reactions
Histamine H2 antagonist adverse reactions are usually mild and transient as well as rare (affecting less than 2% of users), and include:
• Dizziness, somnolence, headache
• Confusion, hallucinations, diarrhea, and reversible impotence
Contraindications and Precautions
The histamine H2 antagonists are contraindicated in patients with a known hypersensitivity to the drugs. These drugs are used cautiously in patients with renal or hepatic impairment and in severely ill, older, or debilitated patients. Cimetidine is used cautiously in patients with diabetes. Histamine H2 antagonists are pregnancy category B (cimetidine, famotidine, and ranitidine) and C (nizatidine) drugs and should be used with caution during pregnancy and lactation.
Interactions
The following interactions may occur when a histamine H2 antagonist is administered with another agent:
Proton Pump Inhibitors
Actions
Proton pump inhibitors, such as lansoprazole, omeprazole, pantoprazole, and rabeprazole, are a group of drugs with antisecretory properties. These drugs suppress gastric acid secretion by inhibition of the hydrogen-potassium adenosine triphosphatase (ATPase) enzyme system of the gastric parietal cells. The ATPase enzyme system is also called the acid (proton) pump system. The proton pump inhibitors suppress gastric acid secretion by blocking the final step in the production of gastric acid by the gastric mucosa. Examples of proton pump inhibitors include esomeprazole (Nexium) and omeprazole (Prilosec).
Uses
Proton pump inhibitors are used for treatment or symptomatic relief of various gastric disorders, including:
• Gastric and duodenal ulcers (specifically associated with H. pylori infections)
• GERD and erosive esophagitis
• Pathologic hypersecretory conditions
• Prevention of bleeding in high-risk patients using antiplatelet drugs
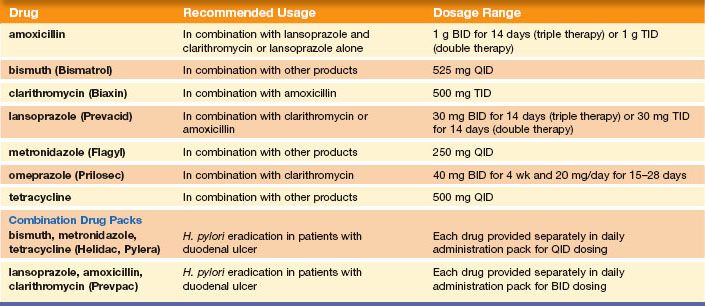
An important use of these drugs is combination therapy for the treatment of H. pylori infection in patients with duodenal ulcers. One treatment regimen used to treat infection with H. pylori is a triple-drug therapy, such as one of the proton pump inhibitors (e.g., omeprazole or lansoprazole) and two anti-infectives (e.g., amoxicillin and clarithromycin). Another triple-drug treatment regimen consists of bismuth plus two anti-infective drugs. Helidac, a triple-drug treatment regimen (bismuth, metronidazole, and tetracycline), may be given along with a histamine H2 antagonist to treat disorders of the GI tract infected with H. pylori. Table 40.1 lists various drug combinations used in the treatment of H. pylori infection. Additional information concerning anti-infective agents is found in Chapters 6 through 9. The Summary Drug Table: Upper Gastrointestinal System Drugs provides additional information on the proton pump inhibitor drugs used in treating H. pylori infection.
Adverse Reactions
The most common adverse reactions seen with the proton pump inhibitors include headache, nausea, diarrhea, and abdominal pain.
Contraindications and Precautions
Proton pump inhibitors are contraindicated in patients who are hypersensitive to any of the drugs. Proton pump inhibitors are used cautiously in older adults and in patients with hepatic impairment. Prolonged treatment may decrease the body’s ability to absorb vitamin B12, resulting in anemia. Omeprazole (pregnancy category C) and lansoprazole, rabeprazole, and pantoprazole (pregnancy category B) are contraindicated during pregnancy and lactation.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Menopausal Women
An increase in fractures of the hip, wrist, and spine have been seen in those taking high doses of proton pump inhibitors and undergoing treatment of osteoporosis with bisphosphonates.
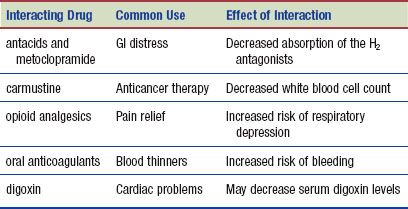
Interactions
The following interactions may occur when a proton pump inhibitor is administered with another agent:
Miscellaneous Acid Reducers
Three other types of acid-reducing drugs that are less frequently used are the cholinergic blocking drugs (also called anticholinergic drugs), a pepsin inhibitor, and a prostaglandin drug. Cholinergic blocking drugs reduce gastric motility and decrease the amount of acid secreted by the stomach. These drugs have been largely replaced by histamine H2 antagonists, which appear to be more effective and have fewer adverse effects. Examples of cholinergic blocking drugs used for GI disorders include propantheline and glycopyrrolate (Robinul). For information about specific cholinergic blocking drugs, see Chapter 27.
Sucralfate (Carafate) is known as a pepsin inhibitor or mucosal protective drug. The drug binds with protein molecules to form a viscous substance that buffers acid and protects the mucosal lining. Sucralfate is used in the short-term treatment of duodenal ulcers. The most common adverse reaction is constipation. Drug interactions of sucralfate are similar to those of the proton pump inhibitors.
A prostaglandin drug, misoprostol (Cytotec), has been used to reduce the risk of nonsteroidal anti-inflammatory drug (NSAID)–induced gastric ulcers in high-risk patients, such as older adults or the critically ill. Misoprostol both inhibits the production of gastric acid and has mucosal protective properties. Because this drug can cause abortion or birth defects, it is not recommended for use in ulcer reduction in women who are pregnant or may become pregnant or who are lactating. Adverse reactions include headache, nausea, diarrhea, and abdominal pain. The drug effects are decreased when it is taken with antacids.
Gastrointestinal Stimulants
Actions
Metoclopramide (Reglan) is used to treat delayed gastric emptying and emesis—that is, it increases the motility of the upper GI tract without increasing the production of secretions. By sensitizing tissue to the effects of acetylcholine, the tone and amplitude of gastric contractions are increased, resulting in faster emptying of gastric contents into the small intestine. It also inhibits stimulation of the vomiting center in the brain.
Uses
The GI stimulants are used in the treatment of the following:
• GERD
• Gastric stasis (failure to move food normally out of the stomach) in diabetic patients, in patients with nausea and vomiting associated with cancer chemotherapy, and in patients in the immediate postoperative period
Adverse Reactions
Adverse reactions associated with metoclopramide are usually mild. Higher doses or prolonged administration may produce central nervous system (CNS) symptoms, such as restlessness, drowsiness, dizziness, extrapyramidal effects (tremor, involuntary movements of the limbs, muscle rigidity), facial grimacing, and depression.
Contraindications and Precautions
The GI stimulant is contraindicated in patients with known hypersensitivity to the drug, GI obstruction, gastric perforation or hemorrhage, or pheochromocytoma. Patients with Parkinson’s disease or a seizure disorder who are taking drugs likely to cause extrapyramidal symptoms should not take these drugs.
This drug is used cautiously in patients with diabetes and cardiovascular disease. Metoclopramide is a pregnancy category B drug. The drug is secreted in breast milk and should be used with caution during pregnancy and lactation.
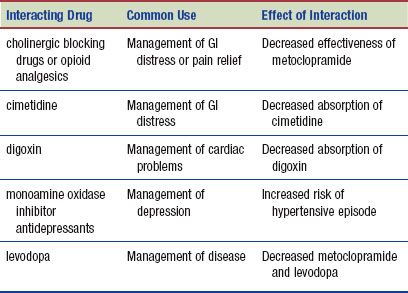
Interactions
The following interactions may occur when a GI stimulant is administered with another agent:
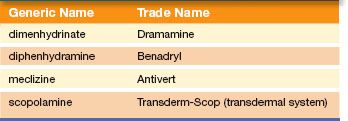
An antiemetic drug is used to treat or prevent nausea (unpleasant gastric sensation usually preceding vomiting) or vomiting (forceful expulsion of gastric contents through the mouth). The drugs discussed in this section are used to treat severe nausea and vomiting. Individuals may experience nausea due to motion sickness or a condition called vertigo (a sensation of spinning or a rotation-type motion). Many of the drugs used to treat motion sickness can be purchased over the counter. Table 40.2 lists examples of drugs used in the treatment of motion sickness or vertigo.
Actions
The brain is involved in the sensation of nausea. The medulla has an area called the vomiting center. The process of vomiting happens when the area is stimulated directly by GI irritation, motion sickness, and vestibular neuritis (inflammation of the vestibular nerve). An adjacent area, the chemoreceptor trigger zone (CTZ), is a group of nerve fibers that sends signals to the vomiting center in the medulla when the metabolism is unbalanced. When these nerves are stimulated by chemicals, such as drugs or toxic substances, impulses are sent to the vomiting center located in the medulla. Vomiting caused by drugs, radiation, and metabolic disorders often occurs because of stimulation of the CTZ. These drugs appear to act primarily by inhibiting the CTZ and the brain’s primary neurotransmitters dopamine and acetylcholine.
Table 40.2 Motion Sickness Drugs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree