CHAPTER 13 Unique Anatomic Features of the Pediatric Spine
IMPORTANCE OF THE PEDIATRIC SPINE
Understanding the spines of children is important for a number of reasons. Contrary to common belief, a fairly high number of children, particularly adolescents, suffer from back pain, and the pain is recurrent in many (Burton et al., 1996). A study of children in Finland, conducted by Taimela et al. (1997), showed the following prevalence of back pain among children:
No difference was found in the incidence of low back pain between males and females in the study. However, pain was identified as being chronic or recurrent in 26% of boys with low back pain and in 33% of girls with low back pain (Taimela et al., 1997). Perhaps surprisingly, intervertebral disc (IVD) degeneration has been identified in with magnetic resonance imaging (MRI) in 15-year-old children, and an unexpectedly high number of young people in their twenties have bulging IVDs that are thought to be the cause of their back pain (Kraemer, 1995; Salminen et al., 1995). IVD protrusion is more prevalent in taller adolescents who have less ability to forward flex than in those of average height with better mobility in forward flexion (Salminen, Erkintalo-Tertti, and Paajanen, 1993). As might be expected, the incidence of low back pain among children who are less physically active is higher than in children who engage in the average level of physical activity (Salminen et al., 1995). Fortunately low back pain in childhood and adolescence does not seem to be related to disabling back pain in adulthood (Burton et al., 1996).
The purpose of this chapter is to identify unique anatomic features related to the pediatric spine. A separate chapter on this topic is important because the spines of children are not just miniature versions of the spines of adults. For example, many of the differences related to the pediatric spine can be mistaken for fractures on the x-rays of children (Fesmire and Luten, 1989). Because normally children are not x-rayed unless the chief complaint is related to trauma, or suspected trauma or other serious pathology, the identification of fractures is a primary focus when viewing these x-ray films. Knowing the precise locations of the ossification centers and the locations of closure, or final union, of the primary and secondary centers of ossification is important because these sites are the regions that can be mistaken for fractures most easily.
AGE-RELATED ANATOMIC CHANGES OF THE PEDIATRIC SPINE
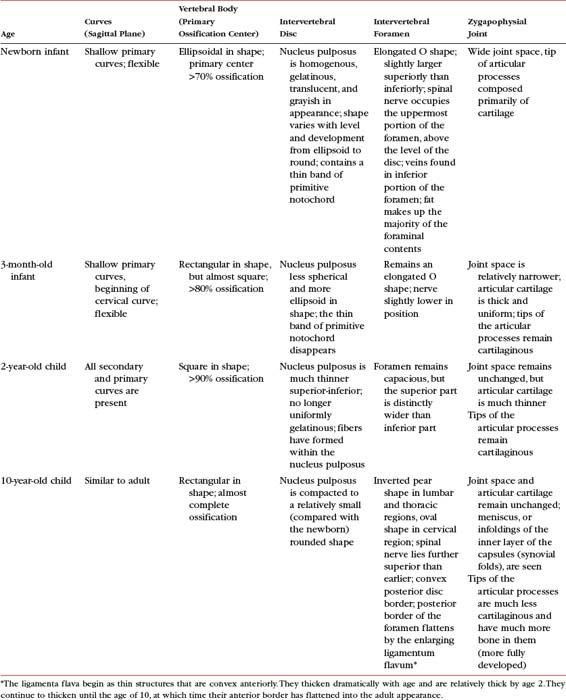
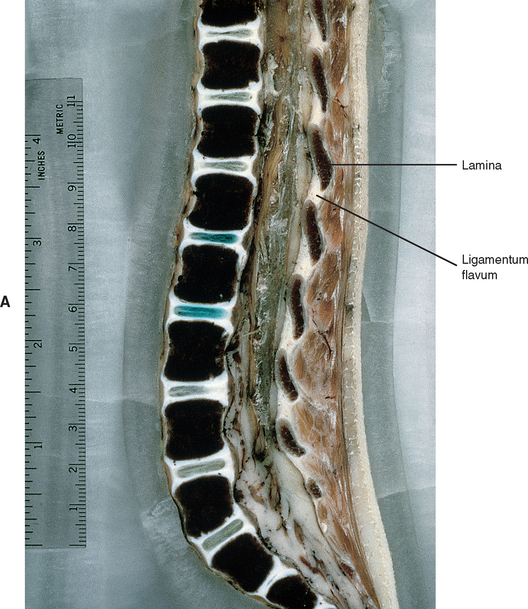
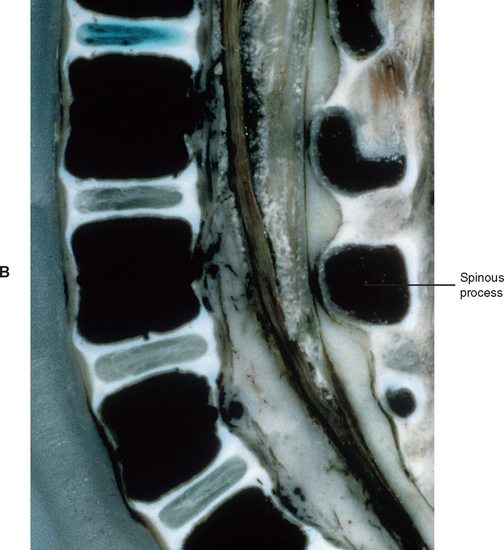
The age-related changes to key anatomic structures of the spine are covered in several ways in this chapter. First, Table 13-1 describes the changes of key anatomic structures for several pediatric age groups. Notice that the key anatomic structures included in Table 13-1 are the curves of the spine, vertebral bodies, IVDs, intervertebral foramina (IVFs), Z joints, and neurologic elements in the vertebral canal. The age groups of Table 13-1 are newborn, 3 months, 2 years, and 10 years. Next, the following sections briefly summarize the most important anatomic changes for the age groups just listed. Finally, age-related changes of the Z joints and the IVFs are described. These two anatomic structures are featured because they undergo unique and clinically important changes with age.
The Newborn Spine
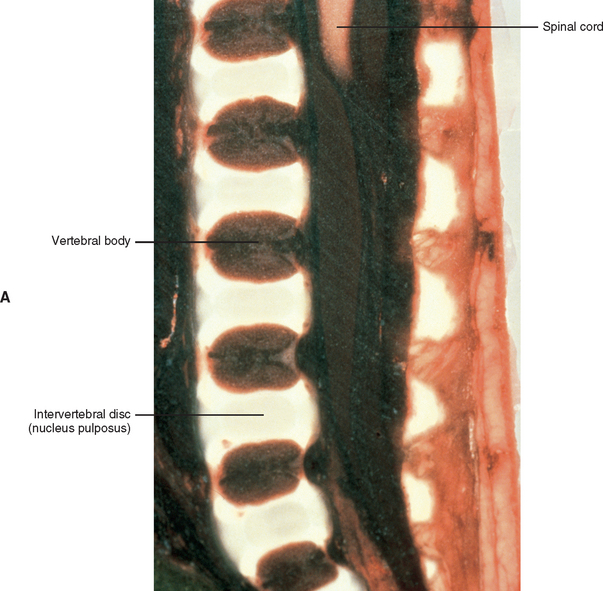
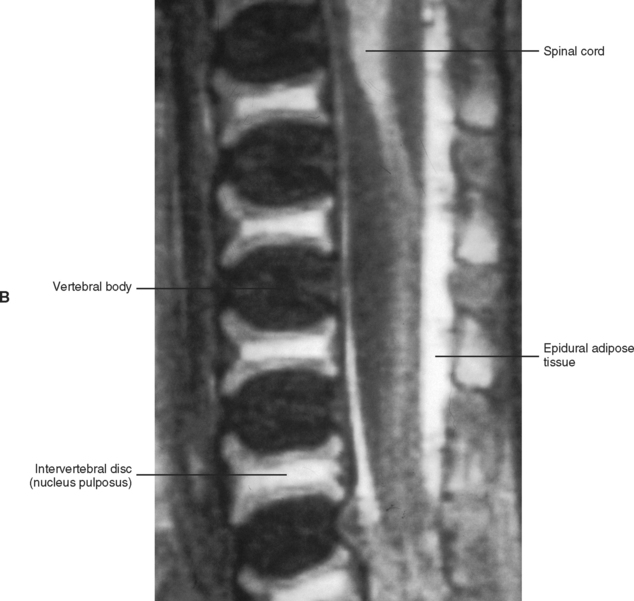
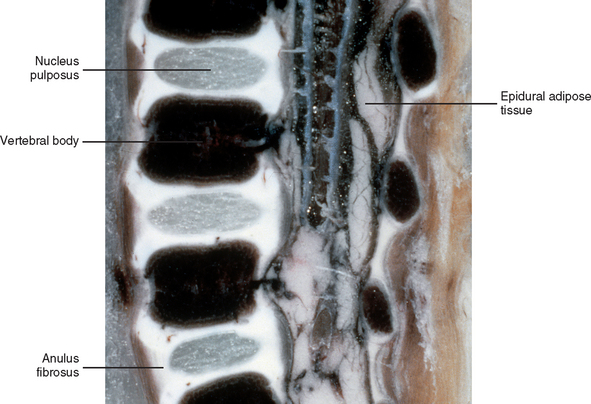
The primary curves (thoracic and sacral kyphoses) of the newborn spine are developed; however, the secondary curves are rudimentary. The vertebral bodies of the newborn spine are more or less ellipsoidal in shape. They are considerably ossified at birth (70%). The IVDs of the newborn are extremely large relative to their adult size, and the nucleus pulposus is more or less rounded in shape (Fig. 13-1).
At birth, the vertebral canal between L1-4 is 70% of its adult size; however, the L5 vertebral foramen and the L5-S1 vertebral canal are only 50% developed. The remaining 30% of the L1-4 vertebral canal development is completed by the end of the first year of infancy, whereas the L5 vertebral foramen and canal continues to develop until approximately 5 years of age. Of clinical importance is that the vertebral canal does not undergo “catch-up growth;” that is, if development is incomplete in infancy the vertebral canal will remain smaller than normal throughout life (Ursu, Porter, and Navaratnam, 1996).
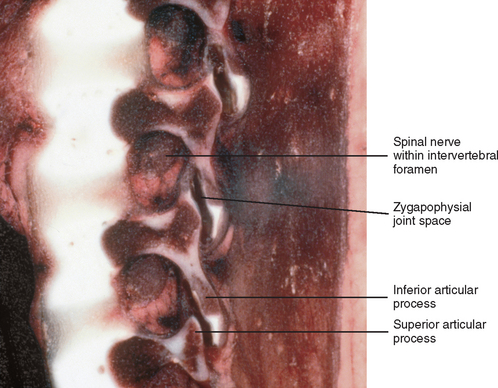
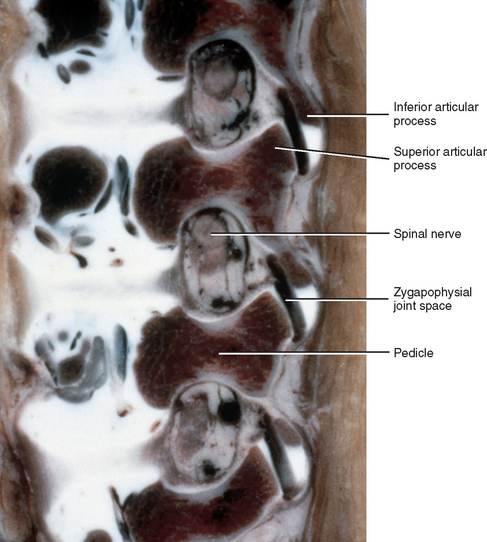
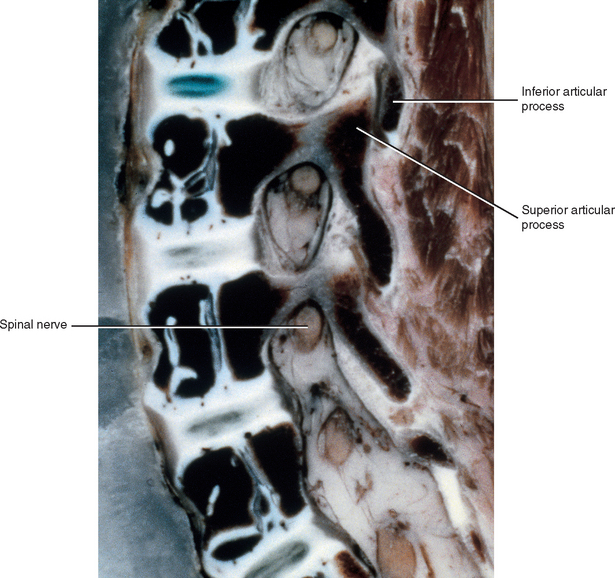
Newborn IVFs are relatively huge (Fig. 13-2). The term capacious is used sometimes to describe the size of the IVFs with respect to the relatively small foraminal contents of young children. Occasionally authors incorrectly apply the term capacious to the IVFs of adults (Crelin, 1973), whereas others have shown that this clearly is not the case (Hewitt, 1970; Giles, 1994). The main reason for the relatively large size of the IVFs in newborns is that the Z joints, which form the posterior border of the IVFs, are underdeveloped in young children (see Fig. 13-2). Both the superior and inferior articular processes are extremely small and the distal ends of both are primarily cartilaginous. The spines of newborns should be handled with extreme care for this reason.
The plane of articulation of the newborn Z joints is more horizontal in orientation than in the adult. This plane gradually becomes more vertically oriented until the age of 10 years, when the adult angle of approximately 45 degrees to the vertical plane is achieved (Kasai et al., 1996).
The 3-Month-Old Spine
The vertebral bodies are continuing to ossify at 3 months of age; they are now approximately 80% ossified, compared with the 70% ossification found in the newborn. The vertebral bodies also are becoming more rectangular in shape, rather than the ellipsoidal shape seen in newborns. The IVDs are narrowing from superior to inferior and the nucleus pulposus is taking on a more ellipsoidal shape, rather than the rounded shape of newborns (Fig. 13-3).
The IVFs of 3-month-old spines remain large, and the articular processes of the Z joints remain relatively underdeveloped (Fig. 13-4). The distal ends of the superior and inferior articular processes are still primarily composed of cartilage (see Fig. 13-4).
The 2-Year-Old Spine
The primary thoracic and sacral curves are well defined at 2 years of age. In addition, both secondary curves have developed at this age. That is, the cervical lordosis developed at approximately 3 months of age, and the lumbar lordosis began between 9 and 12 months of age. Like the cervical lordosis, the lumbar lordosis is created by postural changes. Specifically the lumbar lordosis begins when the infant starts to pull himself or herself up to stand, and then begins to walk. The cervical lordosis is greater in infants less than 5 years of age than in children above this age and in adults. This is thought to be the result of holding up the comparatively heavy head with the relatively underdeveloped cervical vertebrae and cervical paraspinal musculature (Kasai et al., 1996).
The vertebral bodies of the 2-year-old child are almost 90% ossified, and are almost fully developed. They are more rectangular in shape than at 3 months, and the superior and inferior bony rims of the vertebral bodies are more “squared off” at this stage, rather than rounded, as in the 3-month-old infant. At 2 years the IVDs are narrowing from top to bottom, taking on more of an adult type of appearance, although significant further development remains to be completed (Fig. 13-5).
The IVFs of the 2-year-old spine remain capacious; however, they begin to slightly narrow at their inferior aspect, particularly in the lumbar region (Fig. 13-6). The superior and inferior articular processes, which form the Z joints, begin to grow into the posterior and inferior aspect of the IVFs and then become more fully ossified during this stage of development. Even with this added growth and ossification, the Z joints are still relatively underdeveloped, leaving the IVFs comparatively large (see Fig. 13-6).
The 10-Year-Old Spine
The neurocentral synchondrosis persists as a plate of growth cartilage until it completes its fusion and is completely replaced with bone at 3 to 6 years of age. This cartilage plate, and later bony plate, which is located within the posterolateral aspect of the fully developed vertebral body, extends from the superior to inferior anular apophyses. This bony plate persists throughout life (Maat, Matricali, and van Persijn van Meerten, 1996). These plates are thought to be the reason that burst fractures of the vertebral body usually do not enter the posterolateral aspect of the anatomic vertebral body, and why during such fractures a central segment of the vertebral body frequently protrudes directly posteriorly, between the “wedge shape” formed by the left and right bony plates found at the neurocentral junction (Maat, Matricali, and van Persijn van Meerten, 1996).
The primary and secondary curves are fully developed at 10 years of age. Although the cervical lordosis may be prominent in early childhood, it diminishes after the age of 5 and is absent in 14% of the late childhood and adolescent population until approximately 16 years of age. This is partially because the cervical vertebral bodies can be wedge shaped (shorter anteriorly) during this period of time. The anterior wedging of the vertebral bodies reduces the cervical lordosis and also can be mistaken for a compression fracture (Fesmire and Luten, 1989). However, the fact that the wedged vertebrae occur at multiple levels precludes fracture.
Ligamentous laxity typically exists in the cervical spines of children, especially those less than 8 years of age. Such laxity can create a pseudosubluxation (i.e., the appearance of dislocation) during forward flexion (Kasai et al., 1996) as seen on lateral x-rays. This phenomenon is found in 46% of children 1 to 8 years old. The pseudosubluxation usually is most marked between the second and third cervical vertebrae (Fesmire and Luten, 1989).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree