Unicentric Hyaline Vascular Variant Castleman Disease
Pei Lin, MD
Key Facts
Clinical Issues
Young adults
Lymphadenopathy, localized
Excision is usually curative
Microscopic Pathology
Large follicles with regressed (involuted) germinal centers
2 or more germinal centers per follicle (“twinning”)
Concentric rings of mantle zone lymphocytes (“onion skin”)
Hyaline-vascular (“lollipop”) follicles
Increased vascular proliferation in interfollicular zones
Plasma cells and immunoblasts are not abundant
Ancillary Tests
Polytypic B cells and normal T cells
Increased FDCs in germinal centers: CD21(+), CD23(+), CD35(+), &/or EGFR(+)
No evidence of monoclonal Ig or TCR gene rearrangements
No consistent cytogenetic or molecular abnormalities known
Top Differential Diagnoses
Castleman disease, plasma cell variant
Thymoma
Angioimmunoblastic T-cell lymphoma
HIV lymphadenitis
Castleman-like changes associated with various lymphomas
TERMINOLOGY
Abbreviations
Castleman disease, hyaline-vascular variant (HV-CD)
Synonyms
Angiofollicular lymph node hyperplasia
Giant lymph node hyperplasia
Angiomatous lymphoid hamartoma
Definitions
Typically unicentric and reactive lymphoproliferation of unknown etiology involving lymph nodes
ETIOLOGY/PATHOGENESIS
Unknown
Possible factors in pathogenesis
Dysregulation of vascular endothelial growth factor
Follicular dendritic cell (FDC) dysplasia may be precursor
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Young adults; median age: 4th decade
Gender
No preference
Presentation
Patients present with localized mass
Mass often detected incidentally
Rarely symptoms related to compression of adjacent tissues by enlarged lymph nodes
Lymphadenopathy, localized
Mediastinal or thoracic lymph nodes most commonly involved
Other sites: Cervical and retroperitoneal lymph nodes
Extranodal sites of involvement are rare
Patients may develop secondary amyloidosis
Treatment
Surgical approaches
Surgery to remove enlarged lymph nodes
Adjuvant therapy
Usually not necessary
Radiation therapy has been used to alleviate compression symptoms
Prognosis
Excellent
Surgical removal is usually curative; relapse can occur uncommonly
Malignant neoplasms can arise in association with HV-CD
Follicular dendritic cell sarcomas are most common
Vascular neoplasms
Secondary neoplasms in HV-CD are often low grade but metastases are reported
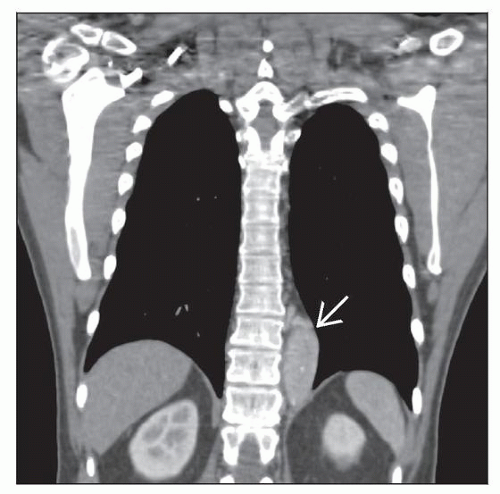
IMAGE FINDINGS
Radiographic Findings
Enlarged lymph node or group of lymph nodes, but any site can be involved
Mediastinal or thoracic lymph nodes most common
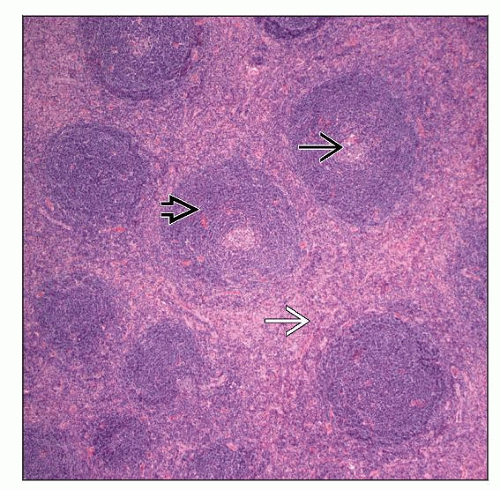
MICROSCOPIC PATHOLOGY
Histologic Features
Numerous follicles in cortex and medulla of lymph node
Obliteration of subcapsular sinuses
2 or more germinal centers in a follicle (“twinning”)
Follicles typically large with regressed (or involuted) germinal centers
Germinal centers are composed mostly of FDC with few lymphocytes
FDCs often hyperplastic and can show dysplasia
Many follicles show so-called “lollipop” features characterized by
Concentric rings of the mantle zone lymphocytes (“onion skin” appearance)
Sclerotic blood vessels radially traversing into germinal center
Interfollicular or stromal component is also important
Increased number of high endothelial venules with hyalinized walls
Stromal component can predominate with only few hyaline-vascular follicles
Clusters of plasmacytoid dendritic cells (plasmacytoid monocytes) can be prominent
Plasma cells and immunoblasts are not abundant in HV-CD
Much more common in plasma cell variant of CD
ANCILLARY TESTS
Immunohistochemistry
Human herpes virus-8 (HHV8) is absent
Polytypic B cells and T cells
Increased FDCs in involuted germinal centers often positive for CD21, CD23, CD35, or EGFR
Dysplastic FDCs often stain variably for FDC markers
Plasma cells are polytypic
Flow Cytometry
Polytypic B cells and T cells with normal immunophenotype
Cytogenetics
Rare cases reported with chromosomal translocations or other clonal abnormalities
No consistent cytogenetic findings
Del(12q13-15) resulted in intragenic HMGIC gene rearrangement reported in 1 case
PCR
No evidence of monoclonal immunoglobulin (Ig) or Tcell receptor (TCR) gene rearrangements
DIFFERENTIAL DIAGNOSIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree