Hairy Cell Leukemia Variant
Roberto N. Miranda, MD
Key Facts
Terminology
Hairy cell leukemia variant (HCL-v)
Mature B-cell neoplasm involving peripheral blood, bone marrow, and spleen
Resembles classical HCL but has atypical hematologic, morphologic, &/or immunophenotypic features
Clinical Issues
Splenomegaly (85%), hepatomegaly (20%), and lymphadenopathy (15%)
Leukocytosis in 90%, with lymphocytosis and normal monocytes
Splenectomy is palliative for symptomatic anemia, thrombocytopenia, and abdominal pain
Partial response with purine analogues in 50% of patients
Microscopic Pathology
Diffuse infiltration of red pulp cords and sinusoids with effacement of white pulp
Small cells with round to oval nuclei and nucleoli
Histologic transformation to large cell or blastic lymphoma can occur
Ancillary Tests
SIg([+] bright), usually IgG(+), CD11c(+), CD22(+), CD103(+/−), FMC7(+)
CD5(−), CD10(−), CD23(−), CD25(−)
Top Differential Diagnoses
Classical HCL
Splenic diffuse red pulp small B-cell lymphoma
Splenic marginal zone lymphoma/SLVL
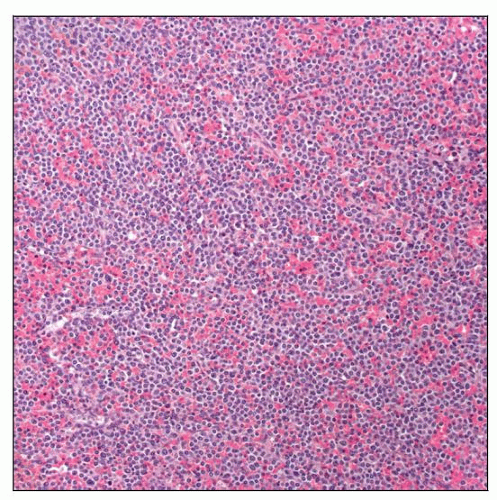 Hairy cell leukemia variant (HCL-v) shows a diffuse infiltrate throughout splenic red pulp cords and sinuses, with complete obliteration of white pulp nodules. |
TERMINOLOGY
Abbreviations
Hairy cell leukemia variant (HCL-v)
Synonyms
Splenic B-cell lymphoma with villous lymphocytes
Also used for splenic marginal zone lymphoma (SMZL)
Prolymphocytic variant of hairy cell leukemia (HCL); term is obsolete
Definitions
Mature small B-cell neoplasm that primarily involves peripheral blood, bone marrow, and spleen
Resembles classical HCL but has atypical laboratory, morphologic, or immunophenotypic features
Provisional entity in 2008 WHO classification
ETIOLOGY/PATHOGENESIS
Environmental Exposure
No known association with exposure to carcinogens, viral infections, or radiation
Cell of Origin
Activated mature memory B cell
CLINICAL ISSUES
Epidemiology
Incidence
HCL-v is less frequent than classical HCL, < 0.4% of all lymphoid leukemias
HCL-v may be more frequent in Asian countries (Japanese form of HCL-v)
Age
Predominantly affects elderly people
Median: 71 years
Gender
M:F = 1.6:1
Presentation
Splenomegaly (85%)
Hepatomegaly (20%)
Lymphadenopathy (15%)
Laboratory Tests
Leukocytosis (> 10 × 109/L) in 90%, with lymphocytosis and normal monocyte count
Median leukocyte count: 34 × 109/L
Thrombocytopenia (< 100 × 109/L) in 40%
Anemia (Hgb < 10 g/L) in 30%
Treatment
Partial response with purine analogues in 50% of patients
Pentostatin or cladribine
Interferon-α is not effective
Splenectomy is good palliative alternative for symptomatic anemia, thrombocytopenia, or abdominal pain
Usually partial response; median duration of 4 years
Prognosis
Indolent clinical course; median survival: 9 years
Morbidity related to splenomegaly, hypersplenism, and cytopenias
Histologic transformation of disease in 6%
B-symptoms, marked lymphocytosis, or lymphadenopathy may indicate transformation
Poor prognosis
MACROSCOPIC FEATURES
General Features
Splenomegaly with diffuse effacement
MICROSCOPIC PATHOLOGY
Histologic Features
Spleen
Diffuse infiltration of red pulp cords and sinusoids
Dilated sinusoids with abundant lymphocytes
Red blood cell lakes may be noted
Atrophy or complete effacement of white pulp
Liver
Infiltration in portal tracts and within sinusoids
Bone marrow
Interstitial and nodular lymphocytic distribution; occasional intrasinusoidal pattern
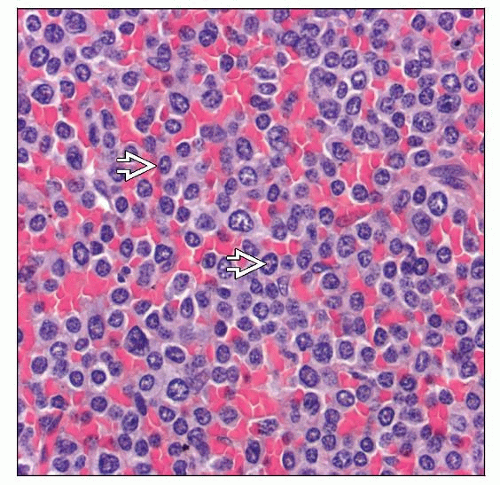
Cytologic Features
Peripheral blood smear
Circulating HCL-v cells easily identified
Some authors require 20-30% of villous lymphocytes for diagnosis
Cytoplasm is abundant, bluish to basophilic
Cytoplasmic projections around part of cell circumference
Round to oval nuclei with distinct nucleoli
Spleen and other tissue sites
Intermediate size lymphocytes with scant to moderately abundant indistinct cytoplasm
Variation in nuclear features; most commonly round with distinct, eccentric nucleoli
“Fried egg” or “honeycomb” appearance uncommon
Histologic transformation is characterized by large cells or cells with blastic chromatin
High mitotic rate
Predominant Pattern/Injury Type
Lymphoid, diffuse
Predominant Cell/Compartment Type
Lymphocytosis
ANCILLARY TESTS
Immunohistochemistry
B-cell antigens(+), DBA.44/CD76(+)
Tartrate-resistant acid phosphatase (TRAP)
Immunohistochemistry can be positive
Cytochemistry usually negative or weakly positive
CD123(−), annexin-A1(−), HC2(−), CD10(−), Bcl-6(−)
Flow Cytometry
Mature B cells with strong surface immunoglobulin (Ig)
Usually IgG, sometimes IgM and IgD are coexpressed
CD11c(+), CD22(+), CD79b([+] ˜ 20%), CD103([+] ˜ 70%), FMC7(+)
CD5(−), CD10(−), CD23(−), CD25(−), CD27(−/+)
Cytogenetics
No specific changes
Some cases show complex karyotypes
Involving 8q24/MYC, 14q32/IgH, and del(17p)/p53
Molecular Genetics
Monoclonal IgH and Ig light chain gene rearrangements
HCL-v cells carry MYC transcripts; associated with resistance to interferon-α therapy
P53 gene deleted in subset of cases is common
Higher risk of histologic transformation
DIFFERENTIAL DIAGNOSIS
Hairy Cell Leukemia (HCL), Classical
Patients present with pancytopenia and monocytopenia
Few leukemic HCL cells in blood smear
“Fried egg” appearance in tissue sections
CD25(+), CD123(+), annexin-A1(+), HC2(+)
T-bet(+), c-MAF(+)
Splenic Diffuse Red Pulp Small B-cell Lymphoma (SDRP SBCL)
Provisional entity in 2008 WHO Classification
Mature B-cell small lymphocytes with diffuse pattern involving red pulp and sinuses
Cytologically display central round nuclei with indistinct nucleoli; occasional cytoplasmic projections
Less degree of lymphocytosis; more IgM/IgD expression than HCL-v
Appears to have substantial overlap with HCL-v
Splenic Marginal Zone Lymphoma (SMZL)/Splenic Lymphoma with Villous Lymphocytes (SLVL)
Prominent nodular involvement of white pulp with secondary red pulp involvement
White pulp has biphasic histologic appearance
Neoplastic lymphocytes of intermediate size with moderately abundant cytoplasm
In blood smear: Cells have polar cytoplasmic projections (villous lymphocytes)
IgM(+), IgD(+/−), CD11c(+), CD79b(+)
CD5(−/+), CD10(−), CD23(−/+), CD43(−), CD103(−), annexin-A1(−)
B-cell Prolymphocytic Leukemia (B-PLL)
Aggressive disease with marked peripheral blood lymphocytosis
Intermediate size lymphocytes with prominent central nucleoli
Cells lack cytoplasmic villous projections
Marked splenomegaly
Prominent nodular white pulp with secondary red pulp involvement
Nucleoli are difficult to appreciate in tissue sections without 1,000x (oil) magnification
IgM(+), IgD(+/−), B-cell antigens(+), CD5(+/−), CD79b(+), CD10(−)
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL)
Prominent nodular involvement of white pulp with secondary red pulp involvement
White pulp has monophasic appearance
Small, round lymphocytes, prolymphocytes, and paraimmunoblasts
IgM(+), IgD(+/−), CD5(+), CD23(+), CD10(−), CD22(−), CD79b(−/+)
Mantle Cell Lymphoma (MCL)
Prominent nodular involvement of white pulp with secondary red pulp involvement
White pulp has monophasic appearance
Monotonous tumor cell population; no large cells (in typical cases)
IgM(+), IgD(+), CD5(+); Cyclin-D1(+, bright), CD23(−/+), CD10(−), DBA.44/CD76(−)
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
Leukocytosis and lymphocytosis common
Pathologic Interpretation Pearls
Spleen: Diffuse expansion of red pulp cords and sinuses with effacement of white pulp
Blood: Small cells with distinct nucleoli and cytoplasmic projections
CD11c(+), CD22(+), CD103(+/−), CD25(−), and TRAP cytochemistry(−)
SELECTED REFERENCES
1. Dong HY et al: Immunophenotypic analysis of CD103+ B-lymphoproliferative disorders: hairy cell leukemia and its mimics. Am J Clin Pathol. 131(4):586-95, 2009
2. Hashimoto Y et al: Hairy Cell Leukemia-Related Disorders Consistently Show Low CD27 Expression. Pathol Oncol Res. Epub ahead of print, 2009
3. Petit B et al: Among 157 marginal zone lymphomas, DBA.44(CD76) expression is restricted to tumour cells infiltrating the red pulp of the spleen with a diffuse architectural pattern. Histopathology. 54(5):626-31, 2009
4. Cannon T et al: Hairy cell leukemia: current concepts. Cancer Invest. 26(8):860-5, 2008
5. Matutes E et al: Splenic marginal zone lymphoma proposals for a revision of diagnostic, staging and therapeutic criteria. Leukemia. 22(3):487-95, 2008
6. Traverse-Glehen A et al: Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity? Blood. 111(4):2253-60, 2008
7. Razaq M et al: Hairy cell leukemia variant transforming into aggressive lymphoma with prostatic involvement in a patient with polycythemia vera. Leuk Lymphoma. 47(4):754-7, 2006
8. Cessna MH et al: Hairy cell leukemia variant: fact or fiction. Am J Clin Pathol. 123(1):132-8, 2005
9. Del Giudice I et al: The diagnostic value of CD123 in B-cell disorders with hairy or villous lymphocytes. Haematologica. 89(3):303-8, 2004
10. Kansal R et al: Histopathologic features of splenic small B-cell lymphomas. A study of 42 cases with a definitive diagnosis by the World Health Organization classification. Am J Clin Pathol. 120(3):335-47, 2003
11. Matutes E et al: The variant form of hairy-cell leukaemia. Best Pract Res Clin Haematol. 16(1):41-56, 2003
12. Mollejo M et al: Splenic small B-cell lymphoma with predominant red pulp involvement: a diffuse variant of splenic marginal zone lymphoma? Histopathology. 40(1):22-30, 2002
13. Matutes E et al: The natural history and clinico-pathological features of the variant form of hairy cell leukemia. Leukemia. 15(1):184-6, 2001
14. Sun T et al: Relationship between hairy cell leukemia variant and splenic lymphoma with villous lymphocytes: presentation of a new concept. Am J Hematol. 51(4):282-8, 1996
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree