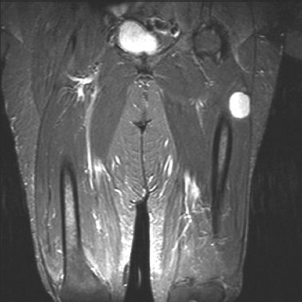
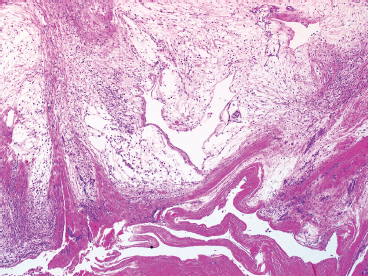
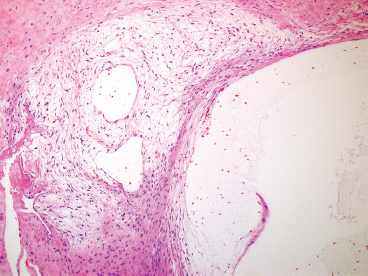
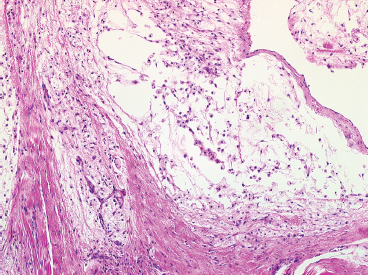
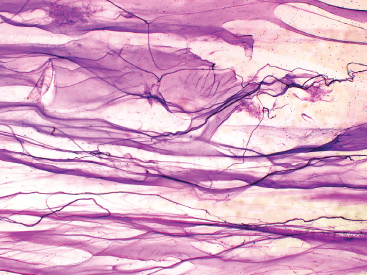
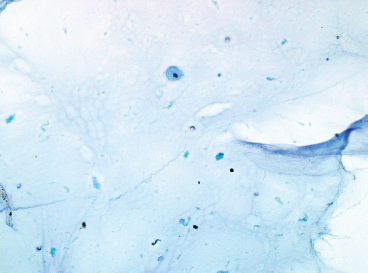
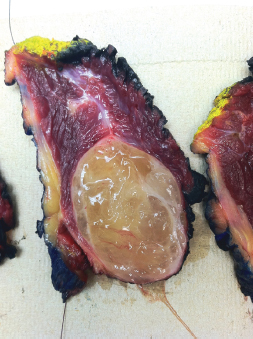
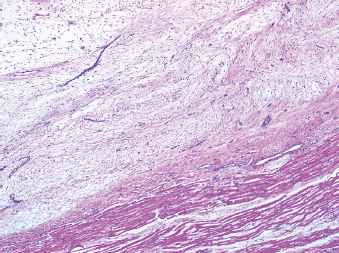
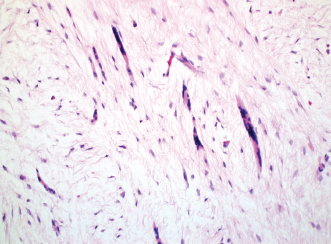
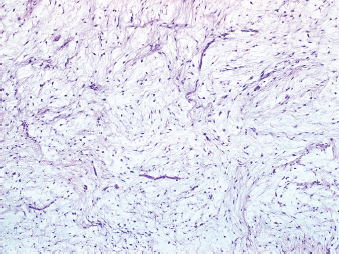
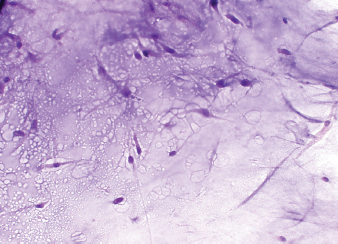
TUMORS WITH MYXOID STROMA 5.5 Extraskeletal Myxoid Chondrosarcoma 5.6 Myxofibrosarcoma (High Grade) Ganglion cysts are relatively common lesions, thought to be reactive or degenerative in nature. Ganglia are most commonly located on the dorsal aspect of the wrist. Other common locations include the fingers and the dorsum of the feet and toes (Figure 5.1.1). They frequently are attached to either a joint capsule or a tendon sheath and seldom reach a size greater than 3 to 4 cm. Ganglia are also colloquially known as “bible bumps” or “bible cysts” because an appropriate treatment would be to hit the lesion with a large book such as the Bible. The trauma of the impact would cause a rupture of the cyst and discharge of its contents into adjacent soft tissue. A more modern approach to cure is a simple excision. When excised, the cyst walls are often completely or partially collapsed (Figures 5.1.2 and 5.1.3). The surrounding soft tissue is often compressed to form a thick fibrous wall. A key to the correct diagnosis is finding focal areas of myxoid change adjacent to the cystic component (Figure 5.1.4). The differential diagnosis of this lesion is very limited due to its characteristic clinical presentation. Aspirates of ganglia are often attempted for both diagnostic and therapeutic purposes. The aspirated material is often very thick and viscous and may clog the needle, preventing a complete evacuation of the cyst. On air-dried, Giemsa-stained preps, the mucoid material is thick and purple in color (Figure 5.1.5). Because of its relative viscosity, the material often folds upon itself, resulting in a pattern of waves on the slide. Ganglia are very paucicellular, and only rare macrophages should be present (Figure 5.1.6). FIGURE 5.1.1 Ganglia tend to occur in the distal extremities. The hands and feet are the most common locations. FIGURE 5.1.2 When removed, the cystic component tends to collapse in sectioning and processing, leaving behind myxoid material and bland fibrous walls. FIGURE 5.1.3 Occasionally, small “daughter” cysts can be seen in the soft tissue adjacent to the main lesion. FIGURE 5.1.4 Focal myxoid change is often seen in the soft tissues adjacent to the main cyst. FIGURE 5.1.5 Aspirates of ganglia are most often comprised of abundant thick material, which stains magenta color on Giemsa-based preparations. FIGURE 5.1.6 Aspirates of ganglia are very hypocellular. Occasional small macrophages can be identified within the myxoid material. Myxoma is a benign soft tissue lesion that tends to occur within the skeletal muscle of the upper and lower extremities. Patients are almost always adult, and there is a slight predilection for females. Patients often notice a slowly growing but painless mass of the soft tissues. On imaging, the lesions are characterized by a “bright” signal on T2-weighted images with low-signal intensity on T1 images (Figure 5.2.1). These lesions are completely benign, and excision is curative. Occasional lesions will recur if inadequately removed. Myxomas have been associated with both Carney complex and Mazabraud syndrome. The latter represents a combination of fibrous dysplasia and myxoma, both of which occur as a result of an activating mutation in the GNAS1 gene. Sporadic cases of myxoma may also show the same GNAS1 mutation. Grossly, these lesions are circumscribed but unencapsulated (Figure 5.2.2). On closer inspection, there may be some infiltration of adjacent skeletal muscle at the periphery of the lesion. Atrophic skeletal muscle bundles may be compressed to form a sort of pseudoencapsulated appearance (Figures 5.2.3 and 5.2.4). The interior of the lesion is most commonly hypocellular with an abundance of extracellular myxoid matrix material. The matrix material will often stain positively with either Alcian blue or mucicarmine stains. Interspersed throughout the lesion are small, bland spindle cells with long, delicate cytoplasmic processes (Figure 5.2.5). These are often bipolar but occasionally can be stellate in appearance. These cells are of myofibroblastic origin and display vimentin positivity as well as occasional positive staining for CD34 and muscle markers such as desmin and actin. Myxomas often display either focal or more complete areas of increased cellularity and vascularity. This pattern is often termed the “cellular variant” of myxoma. Although the increased cellularity may be alarming at first glance, mitoses, necrosis, pleomorphism, and hyperchromasia are notably absent. Needle aspiration or other cytologic preparations of myxoma are characterized by an abundance of thick, gelatinous type of extracellular matrix material. On air-dried, Giemsa-based stains, the myxoid matrix is often a brilliant magenta to purple color and may display a fine granular type of texture. Delicate spindled cells are embedded within the matrix (Figure 5.2.6). Individual cells show long indistinct cytoplasmic processes and have inconspicuous nuclei. Macrophages may be present as well. Although occasional small vessel fragments can be present, they should not be complex or branching and should be relatively sparse. If numerous branching vessels are present, one should entertain another diagnosis, particularly myxoid liposarcoma. Juxta-articular myxoma is very similar to the intramuscular variety both histologically and cytologically. This lesion, however, has a propensity to occur near the large joints of the extremities, particularly the knee. These lesions are also more likely to have “ganglion cyst-like” change and focal hemosiderin deposition. Unlike the intramuscular variety described in the preceding, these lesions are not associated with mutations of the GNAS1 gene. FIGURE 5.2.1 MRI of a well-circumscribed intramuscular myxoma showing an intensely bright lesion on T2-weighted imaging. FIGURE 5.2.2 Excised intramuscular myxoma showing a mucoid, glistening cut surface. FIGURE 5.2.3 Myxomas form an incomplete pseudocapsule comprised of compressed and atrophic skeletal muscle and soft tissue. FIGURE 5.2.4 Occasionally small fragments of atrophic skeletal muscle are entrapped within the interior of the lesion. FIGURE 5.2.5 Myxomas have an abundance of extracellular myxoid material, some small (but not branching or complex) vessels, and a very bland spindle cell population. FIGURE 5.2.6 Aspirates of myxoma are composed of abundant thick myxoid material and a sparse population of spindled cells with long cytoplasmic processes. Aggressive angiomyxoma is often referred to as “deep” angiomyxoma, a term that denotes this lesion’s location and biologic behavior. This is a site-restricted neoplasm that tends to arise in the deeper soft tissues of the pelvic or perineal regions of adult women (Figure 5.3.1). This lesion should not be confused with other similar neoplasms that occur in the same region, namely angiomyofibroblastoma and cellular angiofibroma. These two lesions more often arise in the more superficial soft tissues. The distinction between these entities is important as an angiomyxoma will recur if not completely excised. Deep angiomyxoma is often not detected until it reaches a very large size (Figure 5.3.2). Over half of patients have large (>10 cm in size) tumors when they seek medical attention. Symptoms include vague pain or pressure sensations. Affected individuals are most likely to be adult females, but rare cases have been reported in men. Growth of these lesions is hormonally influenced. They are frequently immunoreactive for estrogen and progesterone receptors and may diminish in size when treated by hormone agonists. Although they do not metastasize, they have a propensity to recur and may be associated with morbidity because of their deep-seated location. Aggressive/deep angiomyxomas are often lobulated lesions, which tend to grow around other structures (rectum, vagina) but not infiltrate. They are hypocellular and contain an abundance of a “myxoedematous” type of matrix, which appears somewhat myxoid, but actually represents intralesional edema (Figure 5.3.3). Scattered throughout the lesion are a number of small- to medium-sized vessels with very thin walls. The predominant cell type is a very small spindle cell with indistinct cytoplasmic processes (Figure 5.3.4). Nuclear atypia and pleomorphism are absent. Rare mitotic figures can be seen. The differential diagnosis of aggressive angiomyxoma includes a number of other neoplasms that typically occur in the genital or inguinal region. These include angiomyofibroblastoma, cellular angiofibroma, and myofibroblastoma. Clinical and histologic features of these lesions are summarized in Chapter 6 (Table 6.9.1). The immunohistochemical profile of aggressive or deep angiomyxoma is fairly distinctive. The lesions are often strongly positive for estrogen and progesterone receptors. In addition, the stromal cells also frequently stain for muscle markers including actin and desmin. More recently, a recurrent translocation involving the high-mobility group A (HMGA2) gene locus on chromosome 12 has been identified. Detection of the translocation by fluorescent in situ hybridization (FISH) or of the encoded protein by immunohistochemical analysis can be performed. Although HMGA2 expression is not unique to aggressive angiomyxoma, it does appear to have some usefulness in diagnosis, as HMGA2 transcriptional upregulation is not identified in other tumors of the pelvic and genital regions.
HISTOPATHOLOGY
CYTOLOGIC FEATURES
INTRAMUSCULAR MYXOMA
PATHOLOGIC FEATURES
CYTOLOGIC FEATURES
JUXTA-ARTICULAR MYXOMA
HISTOPATHOLOGY
CYTOLOGIC FEATURES
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree