Chapter 58 DRUG OVERVIEW FOR TREATMENT—SELECTED CONDITIONS ∗Metronidazole is classed as both an antibiotic and an antiprotozoal. The student and the beginning clinician may be overwhelmed by the numerous antibiotics that are available. Table 58-1 serves as a general summary of common offending organisms for various infections. Both the first treatment choice and the alternative treatment suggestions listed are based on a compendium of various authorities. TABLE 58-1 Empirical Antimicrobial Treatment∗ Fluoroquinolones with enhanced activity vs. S. pneumo: gatifloxacin, levofloxacin, and moxifloxacin. ∗Treatment recommendations, dosages, and therapy may vary, depending on age, pregnancy, or lactation. Consult the latest CDC recommendations at www.CDC.gov. Guidelines are provided by the Infectious Diseases Society of America (www.idsociety.org): • Cellulitis, erysipelas: Group A strep, occasionally group B, C, or G; Streptococcus pyogenes, S. aureus (uncommon) • Necrotizing fasciitis, “flesh-eating bacteria”: Usually polymicrobic with gram-positive and gram-negative and anaerobic; groups A, C, and G strep, Vibrio, enterococci, staphylococci, Escherichia coli, Pseudomonas, Proteus, Serratia, Clostridium. These patients require hospitalization. • Diabetic: Group A strep, S. aureus, Enterobacteriaceae, clostridia (rare). Patients often are complicated and require hospitalization. Treatment usually is provided until 3 days after resolution of inflammation. • S. aureus remains a possibility and should be considered if first-line treatment is not successful. Culturing an open wound seldom produces useful information; often the report comes back with multiple organisms. Site of infection and how infection was acquired will often reveal the most likely causative organism. Community-acquired MRSA infection is increasingly common; it should be diagnosed early and treated with medications such as Septra or doxycycline. Vancomycin has become the standard in areas where MRSA infections exceed 15% of the isolate. Alternatives to vancomycin also should be considered so widespread vancomycin resistance may be delayed, if possible. Consider levofloxacin, tetracycline, clindamycin, rifampin, gentamicin, linezolid, daptomycin, and tigecycline. Consult the latest CDC guidelines regularly for recommendations as they are issued. By far, the most common causative agent is a virus, which causes an acute self-limiting disease that should not be treated with an antibiotic. Influenza is caused by a virus and can be treated with the drugs listed in Chapter 15. Evidence suggests that antibiotics, especially broad-spectrum antibiotics, continue to be overused for adult URIs. • Sinusitis, acute: S. pneumoniae, H. influenzae, M. catarrhalis • Less frequent: Group A strep, anaerobes, S. aureus, Streptococcus spp, Neisseria spp, and gram-negative rods • Sinusitis, chronic: Anaerobic bacteria often present (e.g., Bacteroides spp, Peptostreptococcus, Fusobacterium)
Treatment of Specific Infections and Miscellaneous Antibiotics
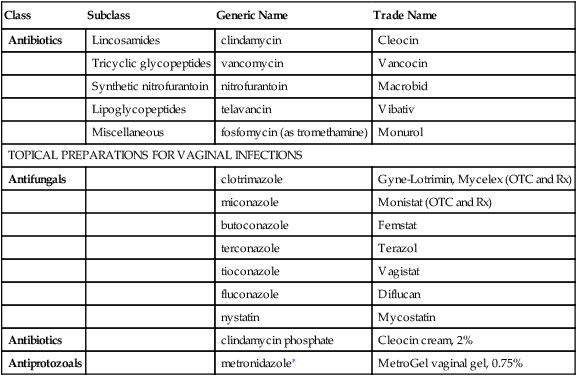
Class
Subclass
Generic Name
Trade Name
Antibiotics
Lincosamides
clindamycin
Cleocin
Tricyclic glycopeptides
vancomycin
Vancocin
Synthetic nitrofurantoin
nitrofurantoin
Macrobid
Lipoglycopeptides
telavancin
Vibativ
Miscellaneous
fosfomycin (as tromethamine)
Monurol
TOPICAL PREPARATIONS FOR VAGINAL INFECTIONS
Antifungals
clotrimazole
Gyne-Lotrimin, Mycelex (OTC and Rx)
miconazole
Monistat (OTC and Rx)
butoconazole
Femstat
terconazole
Terazol
tioconazole
Vagistat
fluconazole
Diflucan
nystatin
Mycostatin
Antibiotics
clindamycin phosphate
Cleocin cream, 2%
Antiprotozoals
metronidazole∗
MetroGel vaginal gel, 0.75%
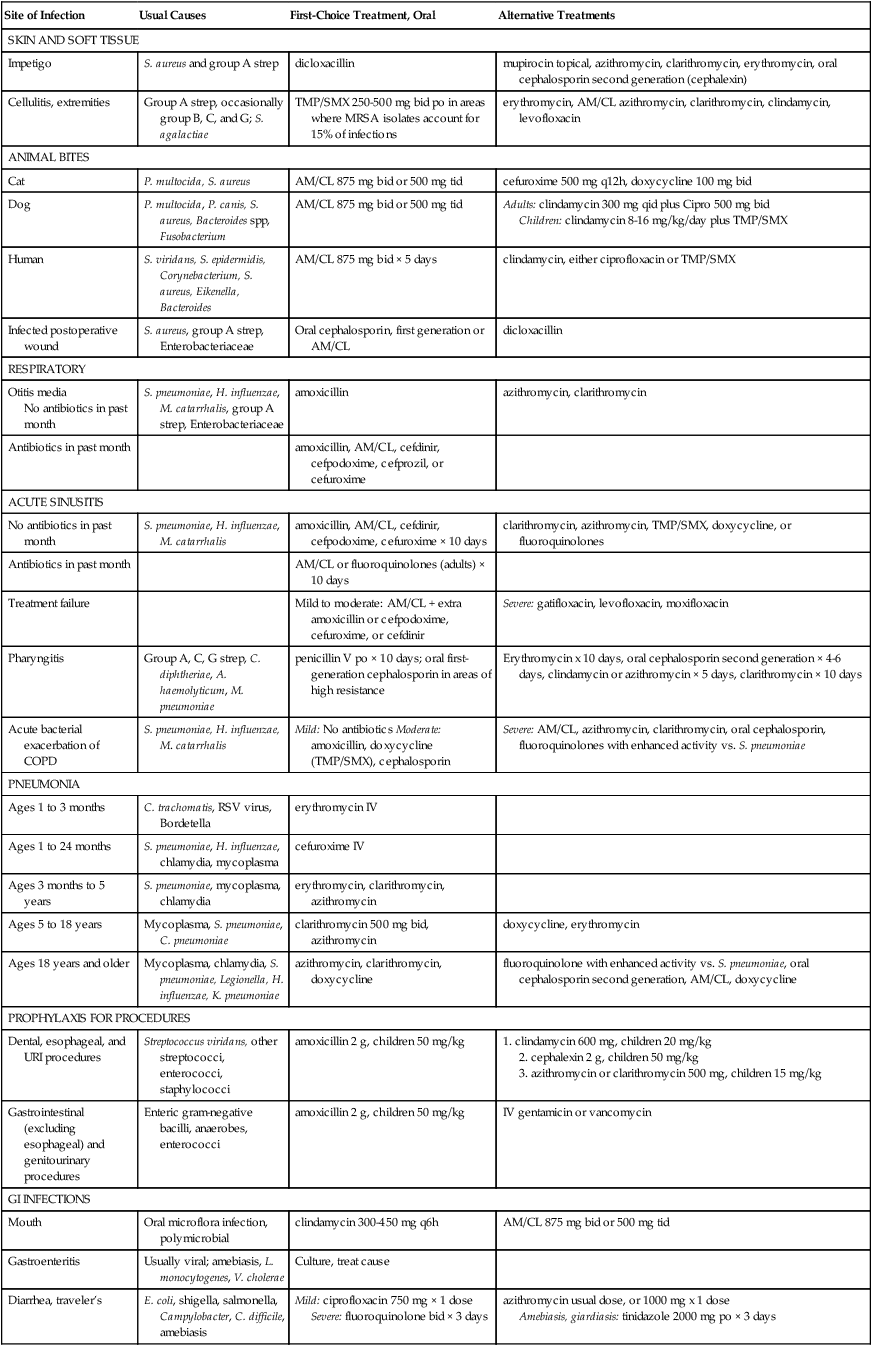
Therapeutic Overview
Site of Infection
Usual Causes
First-Choice Treatment, Oral
Alternative Treatments
SKIN AND SOFT TISSUE
Impetigo
S. aureus and group A strep
dicloxacillin
mupirocin topical, azithromycin, clarithromycin, erythromycin, oral cephalosporin second generation (cephalexin)
Cellulitis, extremities
Group A strep, occasionally group B, C, and G; S. agalactiae
TMP/SMX 250-500 mg bid po in areas where MRSA isolates account for 15% of infections
erythromycin, AM/CL azithromycin, clarithromycin, clindamycin, levofloxacin
ANIMAL BITES
Cat
P. multocida, S. aureus
AM/CL 875 mg bid or 500 mg tid
cefuroxime 500 mg q12h, doxycycline 100 mg bid
Dog
P. multocida, P. canis, S. aureus, Bacteroides spp, Fusobacterium
AM/CL 875 mg bid or 500 mg tid
Adults: clindamycin 300 mg qid plus Cipro 500 mg bid
Children: clindamycin 8-16 mg/kg/day plus TMP/SMX
Human
S. viridans, S. epidermidis, Corynebacterium, S. aureus, Eikenella, Bacteroides
AM/CL 875 mg bid × 5 days
clindamycin, either ciprofloxacin or TMP/SMX
Infected postoperative wound
S. aureus, group A strep, Enterobacteriaceae
Oral cephalosporin, first generation or AM/CL
dicloxacillin
RESPIRATORY
Otitis media
No antibiotics in past month
S. pneumoniae, H. influenzae, M. catarrhalis, group A strep, Enterobacteriaceae
amoxicillin
azithromycin, clarithromycin
Antibiotics in past month
amoxicillin, AM/CL, cefdinir, cefpodoxime, cefprozil, or cefuroxime
ACUTE SINUSITIS
No antibiotics in past month
S. pneumoniae, H. influenzae, M. catarrhalis
amoxicillin, AM/CL, cefdinir, cefpodoxime, cefuroxime × 10 days
clarithromycin, azithromycin, TMP/SMX, doxycycline, or fluoroquinolones
Antibiotics in past month
AM/CL or fluoroquinolones (adults) × 10 days
Treatment failure
Mild to moderate: AM/CL + extra amoxicillin or cefpodoxime, cefuroxime, or cefdinir
Severe: gatifloxacin, levofloxacin, moxifloxacin
Pharyngitis
Group A, C, G strep, C. diphtheriae, A. haemolyticum, M. pneumoniae
penicillin V po × 10 days; oral first-generation cephalosporin in areas of high resistance
Erythromycin x 10 days, oral cephalosporin second generation × 4-6 days, clindamycin or azithromycin × 5 days, clarithromycin × 10 days
Acute bacterial exacerbation of COPD
S. pneumoniae, H. influenzae, M. catarrhalis
Mild: No antibiotics Moderate: amoxicillin, doxycycline (TMP/SMX), cephalosporin
Severe: AM/CL, azithromycin, clarithromycin, oral cephalosporin, fluoroquinolones with enhanced activity vs. S. pneumoniae
PNEUMONIA
Ages 1 to 3 months
C. trachomatis, RSV virus, Bordetella
erythromycin IV
Ages 1 to 24 months
S. pneumoniae, H. influenzae, chlamydia, mycoplasma
cefuroxime IV
Ages 3 months to 5 years
S. pneumoniae, mycoplasma, chlamydia
erythromycin, clarithromycin, azithromycin
Ages 5 to 18 years
Mycoplasma, S. pneumoniae, C. pneumoniae
clarithromycin 500 mg bid, azithromycin
doxycycline, erythromycin
Ages 18 years and older
Mycoplasma, chlamydia, S. pneumoniae, Legionella, H. influenzae, K. pneumoniae
azithromycin, clarithromycin, doxycycline
fluoroquinolone with enhanced activity vs. S. pneumoniae, oral cephalosporin second generation, AM/CL, doxycycline
PROPHYLAXIS FOR PROCEDURES
Dental, esophageal, and URI procedures
Streptococcus viridans, other streptococci, enterococci, staphylococci
amoxicillin 2 g, children 50 mg/kg
1. clindamycin 600 mg, children 20 mg/kg
2. cephalexin 2 g, children 50 mg/kg
3. azithromycin or clarithromycin 500 mg, children 15 mg/kg
Gastrointestinal (excluding esophageal) and genitourinary procedures
Enteric gram-negative bacilli, anaerobes, enterococci
amoxicillin 2 g, children 50 mg/kg
IV gentamicin or vancomycin
GI INFECTIONS
Mouth
Oral microflora infection, polymicrobial
clindamycin 300-450 mg q6h
AM/CL 875 mg bid or 500 mg tid
Gastroenteritis
Usually viral; amebiasis, L. monocytogenes, V. cholerae
Culture, treat cause
Diarrhea, traveler’s
E. coli, shigella, salmonella, Campylobacter, C. difficile, amebiasis
Mild: ciprofloxacin 750 mg × 1 dose
Severe: fluoroquinolone bid × 3 days
azithromycin usual dose, or 1000 mg x 1 dose
Amebiasis, giardiasis: tinidazole 2000 mg po × 3 days
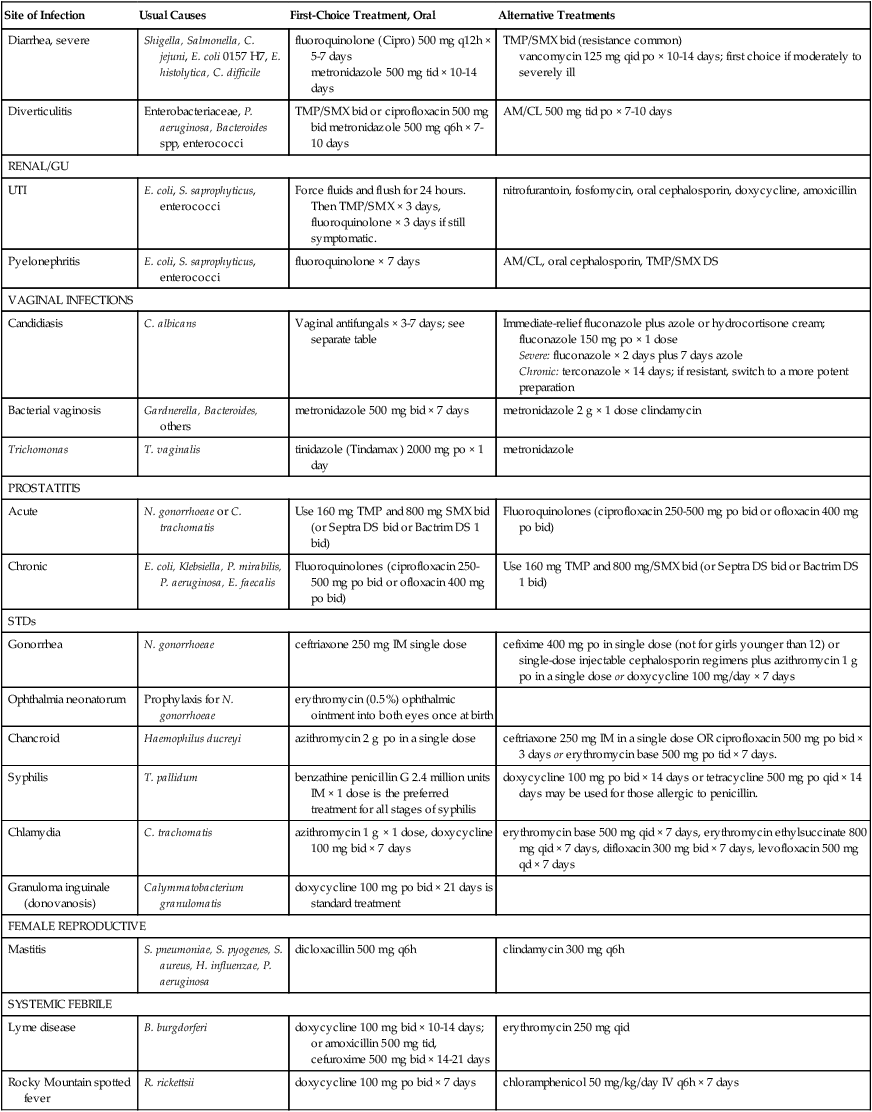
Diarrhea, severe
Shigella, Salmonella, C. jejuni, E. coli 0157 H7, E. histolytica, C. difficile
fluoroquinolone (Cipro) 500 mg q12h × 5-7 days
metronidazole 500 mg tid × 10-14 days
TMP/SMX bid (resistance common)
vancomycin 125 mg qid po × 10-14 days; first choice if moderately to severely ill
Diverticulitis
Enterobacteriaceae, P. aeruginosa, Bacteroides spp, enterococci
TMP/SMX bid or ciprofloxacin 500 mg bid metronidazole 500 mg q6h × 7-10 days
AM/CL 500 mg tid po × 7-10 days
RENAL/GU
UTI
E. coli, S. saprophyticus, enterococci
Force fluids and flush for 24 hours. Then TMP/SMX × 3 days, fluoroquinolone × 3 days if still symptomatic.
nitrofurantoin, fosfomycin, oral cephalosporin, doxycycline, amoxicillin
Pyelonephritis
E. coli, S. saprophyticus, enterococci
fluoroquinolone × 7 days
AM/CL, oral cephalosporin, TMP/SMX DS
VAGINAL INFECTIONS
Candidiasis
C. albicans
Vaginal antifungals × 3-7 days; see separate table
Immediate-relief fluconazole plus azole or hydrocortisone cream; fluconazole 150 mg po × 1 dose
Severe: fluconazole × 2 days plus 7 days azole
Chronic: terconazole × 14 days; if resistant, switch to a more potent preparation
Bacterial vaginosis
Gardnerella, Bacteroides, others
metronidazole 500 mg bid × 7 days
metronidazole 2 g × 1 dose clindamycin
Trichomonas
T. vaginalis
tinidazole (Tindamax ) 2000 mg po × 1 day
metronidazole
PROSTATITIS
Acute
N. gonorrhoeae or C. trachomatis
Use 160 mg TMP and 800 mg SMX bid (or Septra DS bid or Bactrim DS 1 bid)
Fluoroquinolones (ciprofloxacin 250-500 mg po bid or ofloxacin 400 mg po bid)
Chronic
E. coli, Klebsiella, P. mirabilis, P. aeruginosa, E. faecalis
Fluoroquinolones (ciprofloxacin 250-500 mg po bid or ofloxacin 400 mg po bid)
Use 160 mg TMP and 800 mg/SMX bid (or Septra DS bid or Bactrim DS 1 bid)
STDs
Gonorrhea
N. gonorrhoeae
ceftriaxone 250 mg IM single dose
cefixime 400 mg po in single dose (not for girls younger than 12) or single-dose injectable cephalosporin regimens plus azithromycin 1 g po in a single dose or doxycycline 100 mg/day × 7 days
Ophthalmia neonatorum
Prophylaxis for N. gonorrhoeae
erythromycin (0.5%) ophthalmic ointment into both eyes once at birth
Chancroid
Haemophilus ducreyi
azithromycin 2 g po in a single dose
ceftriaxone 250 mg IM in a single dose OR ciprofloxacin 500 mg po bid × 3 days or erythromycin base 500 mg po tid × 7 days.
Syphilis
T. pallidum
benzathine penicillin G 2.4 million units IM × 1 dose is the preferred treatment for all stages of syphilis
doxycycline 100 mg po bid × 14 days or tetracycline 500 mg po qid × 14 days may be used for those allergic to penicillin.
Chlamydia
C. trachomatis
azithromycin 1 g × 1 dose, doxycycline 100 mg bid × 7 days
erythromycin base 500 mg qid × 7 days, erythromycin ethylsuccinate 800 mg qid × 7 days, difloxacin 300 mg bid × 7 days, levofloxacin 500 mg qd × 7 days
Granuloma inguinale (donovanosis)
Calymmatobacterium granulomatis
doxycycline 100 mg po bid × 21 days is standard treatment
FEMALE REPRODUCTIVE
Mastitis
S. pneumoniae, S. pyogenes, S. aureus, H. influenzae, P. aeruginosa
dicloxacillin 500 mg q6h
clindamycin 300 mg q6h
SYSTEMIC FEBRILE
Lyme disease
B. burgdorferi
doxycycline 100 mg bid × 10-14 days; or amoxicillin 500 mg tid, cefuroxime 500 mg bid × 14-21 days
erythromycin 250 mg qid
Rocky Mountain spotted fever
R. rickettsii
doxycycline 100 mg po bid × 7 days
chloramphenicol 50 mg/kg/day IV q6h × 7 days
Skin and Soft Tissue Infections, Including Impetigo
Cellulitis
Respiratory Tract Infections
Sinusitis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Treatment of Specific Infections and Miscellaneous Antibiotics
Only gold members can continue reading. Log In or Register to continue
