Chapter 33 Treatment of Obesity and Eating Disorders
| Abbreviations | |
|---|---|
| CNS | Central nervous system |
| DA | Dopamine |
| GI | Gastrointestinal |
| 5-HT | Serotonin |
| MAO | Monoamine oxidase |
| NE | Norepinephrine |
Therapeutic Overview
| Therapeutic Overview |
|---|
| Obesity |
| Significant risk factors should be present before initiating drug therapy |
| Patients with concurrent diseases such as diabetes and hypertension require close monitoring |
| Exercise and a supervised dietary plan are essential |
| Centrally active drugs that enhance aminergic transmission may be of benefit |
| Peripherally active drugs that decrease fat absorption may be of benefit |
| Anorexia and Bulimia |
| Baseline medical and psychological assessment |
| Psychotherapy is cornerstone of treatment |
| Antidepressants may be of benefit |
| Cachexia |
| Associated with advanced cancers and AIDS |
| Corticosteroids, progestational agents, anabolic steroids, and stimulation of cannabinoid type 1 receptors stimulate appetite and weight gain |
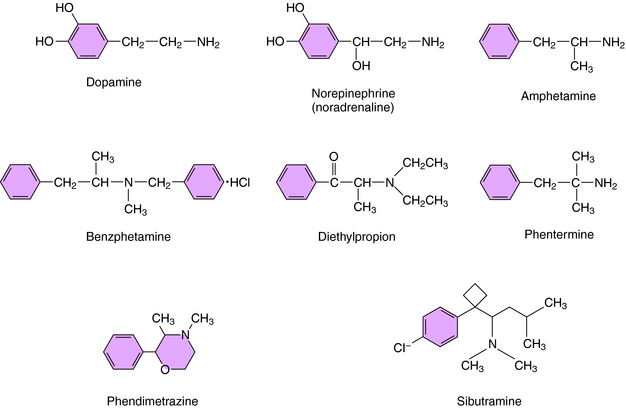
Mechanisms of Action
Drugs approved for the treatment of obesity include centrally active agents and the GI lipase inhibitor orlistat. The four sympathomimetics currently approved for the treatment of obesity include benzphetamine, diethylpropion, phentermine, and phendimetrazine. These drugs are β-phenethylamine derivatives structurally related to the biogenic amines norepinephrine (NE) and dopamine (DA) and to the stimulant amphetamine (Fig. 33-1). As a consequence of the latter, these agents have been deemed to have the potential for abuse and thus are classified by the U.S. DEA as Schedule III (benzphetamine and phendimetrazine) and Schedule IV (diethylpropion and phentermine) drugs, with diethylpropion and phentermine producing less central nervous system (CNS) stimulation than benzphetamine and phendimetrazine. All these agents are indicated for the short-term (up to 12 weeks) treatment of obesity and increase synaptic concentrations of NE or DA by promoting their release. These compounds are believed to suppress appetite through effects on the satiety center in the hypothalamus rather than effects on metabolism.
Orlistat is the only weight-loss drug that does not suppress appetite. Rather, orlistat binds to and inhibits the enzyme lipase in the lumen of the stomach and small intestine, thereby decreasing the production of absorbable monoglycerides and free fatty acids from triglycerides. Orlistat is a synthetic derivative of lipstatin, a naturally occurring lipase inhibitor produced by Streptomyces toxytricini. Normal GI lipases are essential for the dietary absorption of long-chain triglycerides and facilitate gastric emptying and secretion of pancreatic and biliary substances. Because the body has limited ability to synthesize fat from carbohydrates and proteins, most accumulated body fat in humans comes from dietary intake. Orlistat reduces fat absorption up to 30% in individuals whose diets contain a significant fat component. Reduced fat absorption translates into significant calorie reduction and weight loss in obese individuals. In addition, the lower luminal free fatty acid concentrations also reduce cholesterol absorption, thereby improving lipid profiles. Orlistat is not a controlled substance, is approved for the long-term treatment of obesity, and is now available over the counter.
Drugs for Anorexia and Bulimia
Based on evidence that individuals with anorexia and bulimia are prone to mood disturbances, the pharmacological treatment of these disorders has focused on use of antidepressants. Evidence supports the efficacy of these compounds for treatment of bulimia. Antidepressants in all classes including the tricyclic antidepressants, monoamine oxidase (MAO) inhibitors, and selective serotonin reuptake inhibitors have been shown to be equally efficacious. However, because of side effects associated with the use of tricyclic antidepressants and MAO inhibitors (Chapter 30), selective serotonin reuptake inhibitors may be considered first-line agents. Antidepressants reduce binge eating, vomiting, and depression and improve eating habits in bulimia but do not affect poor body image. Imipramine, desipramine, phenelzine, amitriptyline, and trazodone have all been used with some success, but currently fluoxetine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree