•Serum screening for preformed antibodies using a panel of typing cells
•Techniques identical to cross match
•Expressed as a percentage of cells with which the patient’s serum reacts (0% to 100%)
•Sensitization (or increased panel reactive antibody) occurs as a consequence of prior pregnancy, blood transfusion, or transplant

Lymphocytotoxicity cross match. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Cross Match
•Refers to any test for the detection of recipient sensitization against donor HLA
•Presensitization to HLA antibodies occurs only with previous exposure to foreign HLA from blood transfusions, pregnancy, or prior transplantation
•Cross matching to exclude the presence of antibodies to donor leukocytes must be carried out immediately prior to transplantation
•Hyperacute or accelerated rejection frequently occurs if transplantation is performed with a strongly positive cross match (e.g., a positive HLA I IgG cross match)
Methods
1.Complement-dependent lymphocytotoxicity cross match—Utilizes recipient serum, donor cells (T cells, B cells, or monocytes), and complement. If specific donor antibodies are present, antibody binding leads to fixation of complement and lysis of donor lymphocytes. Most commonly used cross match tests utilize mixed lymphocyte populations (most being T cells), therefore a strong cross match indicates antibodies to HLA I.
2.Flow cytometry (FC)—much more specific and sensitive
Is successful kidney/pancreas transplant associated with stabilization of proliferative retinopathy?
Yes—stabilization or even improvement.
Simultaneous Kidney/Pancreas Transplant
•Successful pancreas transplant approximates euglycemia with normalization of glycosylated hemoglobin
•Stabilizes or improves diabetic retinopathy
•Improves both autonomic and peripheral diabetic neuropathy, but requires months to years to be demonstrable
•Prevents recurrence of diabetic nephropathy in transplanted kidneys
•Decreases orthostatic hypotension
•Not associated with reversal of peripheral vascular disease or coronary artery disease
•Overall graft survival rates are up to 90%
Technique of Pancreas Transplant
•Pancreas is anastomosed to the common iliac artery and vein
•Duodenal drainage is most commonly enteric; however, can be into bladder to monitor urinary amylase
•Bladder drainage is associated with hematuria, renal stones, and bicarbonate loss

Simultaneous kidney–pancreas transplant with urinary anastomosis. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
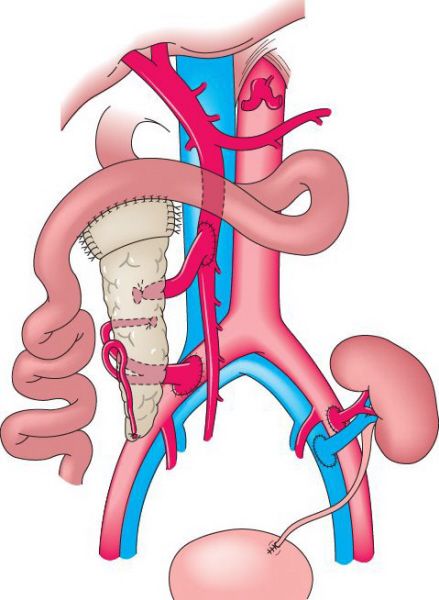
Simultaneous kidney–pancreas transplant with enteric drainage. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
The acceptable maximal cold ischemia time is shortest in which organ/s?
Heart and lungs.
Preservation of Donor Organs
•Hypothermia (4°C to 7°C) to decrease metabolism
•Preservation solutions designed to improve cell wall stability—University of Wisconsin solution (high K and hyperosmolar)
•Cold ischemia time
•Heart/Lung: 0 to 4 hours (ASAP)
•Pancreas: 0 to 12 hours (up to 24)
•Liver: 0 to 12 hours (up to 24)
•Kidney: 0 to 48 hours (72 with perfusion)
What are the criteria to establish brain death?
No pupillary response to light
No corneal reflex
No eye movement with doll’s eyes or caloric testing
No motor response to supraorbital pain
No cough reflex
Apnea
•Each year, there are 11,000 to 14,000 cadaveric organ donors
•Most donors are victims of trauma, cerebrovascular accidents, cerebral anoxia, or non-metastasizing brain tumors
•In 2% of cases, patients are declared dead after cardiovascular death in cases in which brain death criteria have not been met
Prerequisites for Diagnosis of Brain Death
•All appropriate diagnostic and therapeutic procedures have been performed and the patient’s condition is irreversible
•With hypothermia, the patient must be rewarmed to normothermia
•In cases of alcohol ingestion, at least 8 hours must elapse
Clinical Exam for Brain Death
•Apnea test documenting no respiratory drive despite a PaCO2 >50
•Absence of cephalic reflexes (pupillary, corneal, oculo-auditory, oculovestibular, oculocephalic, cough, pharyngeal, and swallowing)
Confirmatory Test (May Be Required in Some States)
•No blood flow to brain on a nuclear medicine perfusion scan
•Lack of brain activity on an electroencephalography (EEG)
Donor Exclusion Criteria
•HIV infection
•Malignancy (except some isolated CNS malignancy)
•Bacterial sepsis
•Hepatitis B surface antigen positive
Relative Contraindications for Organ Donation
•Advanced age
•IV drug use/abuse
•Extensive trauma
What is the mechanism of action of the commonly used immunosuppressive medications?
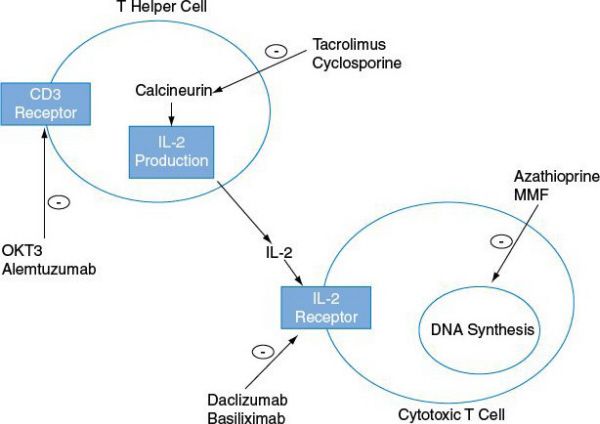
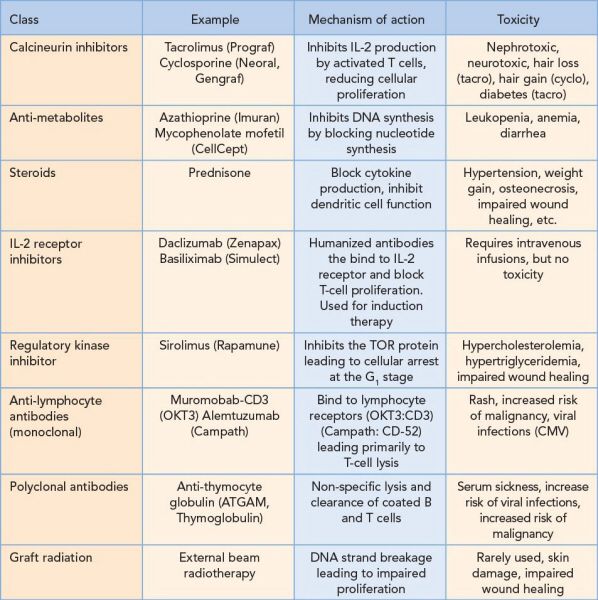
Induction
Given at the time of transplant to reduce the risk of acute cellular rejection
•Monoclonal and polyclonal antibody preparations
•IL-2 receptor inhibitors
Maintenance
Provided to decrease incidence of acute rejection over the life of the graft
•Steroids
•Calcineurin inhibitors
•Anti-metabolites
•Sirolimus
•Steroids
•Monoclonal and polyclonal antibody therapy
•Graft irradiation
Complications of Long-term Immunosuppression
•Nephrotoxicity in patients treated with cyclosporine or tacrolimus contribute to late renal allograft loss and native renal failure in patients receiving extra-renal organs (heart, liver, lung)
•Post-transplant lymphoproliferative disorder: B-cell proliferation with spectrum from benign proliferation that responds to lowering of immunosuppression to malignant B-cell lymphoma requiring chemotherapy. Associated with Epstein Barr virus (EBV).
•Cardiovascular disease: Particularly common in renal transplant patients and patients taking rapamycin
A 24-year-old woman presents 3 weeks after kidney transplant with fever of 102 degree. What is the most likely cause?
Bacterial infection.

Timing of post-transplant infections. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Management of Immunosuppressed Patient with Fever
•History and physical exam with a focus on wound infection, graft tenderness, dysuria, cough, rash, and diarrhea
•Labs/Tests: Urinalysis, chest X-ray, CBC, chemistry, blood cultures
•Empiric antibiotics until culture results return
•Up to 1 month post-transplant: Most commonly caused by bacterial infection in wound, lung, urinary tract, central line associated bacteremia, Clostridium difficile colitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


